BOSTON -- Short-term treatment with one or more antiretroviral drugs starting in late pregnancy--in addition to or instead of single-dose nevirapine--may reduce the likelihood that HIV-infected women will transmit the virus to their newborns and that the women will develop nevirapine resistance, research has shown.
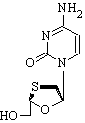
The practice of giving pregnant women with HIV a single dose of nevirapine (Viramune) during labor has significantly reduced maternal/child transmission rates in the developing world. It also has been heralded as an optimal approach for lowering the transmission rates among women in the United States who are identified as HIV positive very late in pregnancy or at the time of labor, and who also may be unlikely to follow extended treatment regimens because of lifestyle or health care inaccessibility.
There is growing evidence, however, that many women who receive this treatment develop mutated strains of the virus that resist future treatment with nevirapine and, potentially, other drugs, said James McIntyre, M.D., at a conference on retroviruses and opportunistic infections.
"While people have been lauding [single-dose nevirapine] as a stunning break-through, others have said it represents a less-than-optimal regimen" to which women in developing countries should not be subjected, said Dr. McIntyre of the perinatal HIV research unit at the University of Witwatersand, Johannesburg, South Africa. "In my country, this has been seen as a U.S. and pharmaceutical company conspiracy."
The value of nevirapine monotherapy should be reassessed, Dr. McIntyre stressed, in light of new evidence suggesting that possible alternatives to the single-dose, single-drug regimen may be as effective at preventing vertical HIV transmission minus the potential for drug resistance.
In one of the studies presented at the conference, which was sponsored by the Foundation for Retrovirology and Human Health, 329 HIV-infected pregnant women in the West African nation of Cote d'Ivoire began therapy with a combination of zidovudine (AZT) and lamivudine (3TC [Epivir in the U.S.]) in their 32nd week of pregnancy through 3 days post partum, in addition to single-dose nevirapine during labor, reported lead investigator Francois Dabis, M.D., of Victor Segalen University in Bordeaux, France. The newborns in the study were treated with AZT for 1 week and a single dose of nevirapine.
The 6-week HIV type 1 (HIV-1) maternal/child transmission rate was 4.7%, representing "among the lowest transmission rates ever reported in Africa," said Dr. Dabis. Single-dose nevirapine alone typically reduces the transmission rate from an estimated 35% to approximately 12%, he noted. (Maternal/child HIV transmission rates in the United States, where women have more access to antiretroviral therapy, are approximately 2%, according to CDC data.)
The drop in nevirapine resistance was even more dramatic, with a reported rate among the mothers of 1.1%. Although the exact mechanism for the reduced resistance rate has yet to be identified, the multidrug strategy "may impair the ability of the virus to mutate into a [nevirapine-] resistant strain," according to Dr. Dabis.
A second study of 1,179 live births conducted in Botswana compared the effect of giving HIV-infected mothers multiweek zidovudine alone versus giving it in combination with single-dose nevirapine. Initially, each mother in the study was given zidovudine from 34 weeks' gestation and each mother/infant pair was randomized to receive blinded maternal and infant single-dose nevirapine or maternal and infant placebo. The study protocol was changed at 17 months because the infant nevirapine placebo was deemed unethical. Under the revised protocol, all infants received nevirapine as soon as possible after birth, while half of the mothers still got placebo, explained lead investigator Roger Shapiro, M.D., of Beth Israel Deaconess Medical Center in Boston.
Before the revision, the 1-month HIV transmission rates in 485 births were 5.3% in babies given nevirapine and 6.2% in babies who received placebo. In the 694 births that occurred during the revised study period, the 1-month transmission rates were 3.7% in babies born to mothers who received nevirapine and 4.3% in babies born to mothers given a placebo. The overall transmission rate for the entire study was approximately 4%, Dr. Shapiro said.
The results suggest that maternal single-dose nevirapine may not be needed to reduce mother/child transmission rates when both mother and infant are treated with zidovudine and when the infant receives nevirapine at birth--an important possibility, given that a substudy of the investigation found that 44% of the women who received the single-dose nevirapine developed resistance mutations, Dr. Shapiro noted.
Although the findings from both studies are promising, "the translation from trials to programs is incredibly challenging," said Mary Glenn Fowler, M.D., chief of maternal-child transmission, Centers for Disease Control and Prevention, Atlanta. "It's important not to be rapidly overoptimistic. We need to see what happens when those women start therapy [after delivery]."
Advocates for AIDS research and treatment agree. A press release issued by the Elizabeth Glaser Pediatric AIDS Foundation stressed the importance of preserving single-dose nevirapine as an option: "Even simple interventions like nevirapine are still available to less than 10% of the women who need them worldwide. Therefore, we must continue to aggressively expand access to services and improve our ability to offer the most effective drug regimens in all instances."
BY DIANA MAHONEY
New England Bureau
COPYRIGHT 2005 International Medical News Group
COPYRIGHT 2005 Gale Group