GAITHERSBURG, MD. -- Entecavir, an oral antiviral drug that has several advantages over currently available treatments for chronic hepatitis B, was approved recently by the Food and Drug Administration.
The approval came after the unanimous recommendation of all 18 members of FDA's Antiviral Drugs Advisory Committee who agreed that the risk-benefit appraisal of entecavir supported its approval for treating chronic hepatitis B virus (HBV) infections in adults. Despite concerns about a theoretical risk of malignancies in humans, the panel voted in favor of approval, citing the very real risk of hepatocellular carcinoma associated with chronic HBV, the safety and effectiveness data in 48-week trials of more than 1,000 patients who were either treatment naive or refractory to lamivudine, and the lack of significant evidence of resistance to date.
There is "no question" entecavir is very effective at reducing viral load, said Leonard Seeff, M.D., senior scientist for hepatitis research at the National Institute of Diabetes and Digestive and Kidney Diseases, Bethesda, Md., who is a member of the panel.
"We need other treatments, and this drug has advantages that others don't--namely, at least at this point, a lower rate of mutant strains developing and no nephrotoxicity," he remarked.
Both he and the other panel members agreed that entecavir should be considered a first-line therapy for treatment-naive patients, emphasizing that the development of resistance needs to be followed closely.
The drug's manufacturer, Bristol-Myers Squibb (BMS), has agreed to conduct a large postmarketing study to determine whether the increased risk of lung tumors and other malignancies seen in rodents would occur in humans, and whether resistant strains would develop with a longer duration of treatment. The multinational trial would aim to enroll 12,500 patients worldwide, randomize them to entecavir or another HBV drug treatment, and follow them for malignancies and progression of liver disease for 5-8 years, according to BMS.
But the panel was concerned that the company could have problems enrolling enough patients in the trial, because entecavir was shown to be more effective than lamivudine in trials.
Panel members also suggested that patients may have to be followed for longer periods.
In preclinical studies, the incidence of lung tumors and other malignancies was increased significantly in rodents exposed to entecavir, mostly at very high doses. To date, however, no increase in malignancies has been detected in clinical trials.
BMS will market entecavir under the trade name Baraclude.
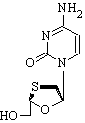
Entecavir is a nucleoside analogue that is a potent, selective inhibitor of HBV replication. Currently available treatments for chronic HBV include interferon, approved in 1992, which is administered subcutaneously and is limited by its side effect profile. The first effective oral treatment for HBV, lamivudine (Epivir), a nucleoside analogue, was approved in 1998, but its usefulness is limited by the emergence of resistant strains. Adefovir dipivoxil (Hepsera), a nucleotide analogue approved in 2002, is active against lamivudine-resistant virus, but can cause nephrotoxicity.
At the meeting, BMS presented the results of clinical trials, including three phase III studies comparing entecavir with lamivudine in more than 1,500 patients with chronic HBV infections and active liver inflammation, including HBeAg-negative and HBeAg-positive patients who had not been treated with a nucleoside, and HBeAg-positive patients who were refractory to lamivudine. The patients in the trials did not have HIV.
In all three groups, a significantly greater proportion of those treated with entecavir than of those treated with lamivudine met the primary end point, histologic improvement in liver biopsy after 48 weeks of treatment. Among the treatment-naive patients, 70%-72% of those on entecavir met this end point vs. 61%-62% of those on lamivudine. Among lamivudine-refractory patients, 55% met this end point, vs. 28% of those who remained on lamivudine.
In all three groups, the mean reduction in HBV DNA was significantly greater among those treated with entecavir, and significantly more patients on entecavir had normalization of ALT levels than did those treated with lamivudine, with the greatest difference among the lamivudine-refractory patients (61% vs. 15%). Among the HBe-positive patients, seroconversion rates were greater among those treated with entecavir, although the differences were not statistically significant.
BY ELIZABETH MECHCATIE
Senior Writer
COPYRIGHT 2005 International Medical News Group
COPYRIGHT 2005 Gale Group