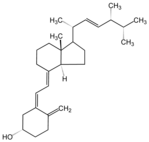
Vitamin D serves to maintain mineral homeostasis by regulation of calcium absorption in the gut and reabsorption by the kidney, and regulation of bone remolding. Vitamin D also acts as a necessary cofactor for insulin secretion. The main sources of vitamin D are ergocalciferol (D2) and cholecalciferol, the former normally available in food and the latter produced in the skin by ultraviolet radiation of 7-dehydrocholesterol. Both of these compounds are hydroxylated in the liver to form 25-hydroxyvitamin D (25[OH]D), which is the major circulating metabolite precursor to the hormonally active form, 1,25-dihyroxyvitamin D (1,25[OH]2D). Hydroxylation of 25(OH)D metabolite, stimulated by parathyroid hormone (PTH), takes place mainly in the kidney and produces the hormonally active metabolite 1,25(OH)2D. The 25(OH)D precursor is widely used to assess the efficacy of vitamin D repletion and has a slower clearance rate from the circulatory stream than 1,25(OH)2D.
Obesity is associated with alterations in the vitamin D endocrine system. The levels of serum intact PTH and 1,25(OH)2D are elevated in morbidly obese patients and levels of 25(OH)D have been found to be reduced. It is likely that obesity associated vitamin D insufficiency is due to a decreased bioavailability of vitamin D3 from cutaneous and dietary sources because of its excessive deposition in body fat compartments. Hypovitaminosis D has been proposed as a risk factor for hypertension, metabolic syndrome, impaired glucose tolerance, and type 2 diabetes.
In order to test the hypothesis that low levels of 25(OH)D negatively influence insulin sensitivity, researchers investigated the relation between serum 25(OH)D and insulin sensitivity in morbidly obese women who had undergone biliopancreatic diversion (BPD) and were reevaluated after 5 years and zero years of follow-up. BPD is a type of malabsorptive bariatric surgery that markedly improves insulin sensitivity and lipid metabolism but greatly reduces circulating 25(OH)D and increases PTH levels. The group studied included 116 white, morbidly obese women aged 20 years to 35 years. None of the subjects had relevant endocrine or non-endocrine disease. They were not taking any medications, except that subjects after BPD were prescribed oral supplementation of 525 mg/day sulfate iron, 1 g/day calcium carbonate, 1 tablet/day multivitamins and 400,000 UI intramuscularly D 2 every 2 weeks.
The subjects were studied before and 5 years and 10 years following BPD. Body composition was estimated by isotopic dilution. Peripheral insulin sensitivity was measured by the EHC procedure. BPD is essentially a malabsorptive surgical procedure. It consists of an approximate 60% distal gastric resection with stapled closure of the duodenal stump. The residual volume of the stomach is approximately 300 mL. The small bowel is transected at 250 cm from the ileocecal valve, and its distal end is anastomosed to the remaining stomach. Prevalence of hypovitaminosis D was 76% in the obese status and 91% and 89% at 5 years and 10 years after BPD, respectively, despite ergocalciferol supplementation. 25(OH)D concentration decreased from 39.2 [+ or -] 22.3 in obesity (p = 0.0001) to 27.4 [+ or -] 16.4 and 25.1 [+ or -] 13.9 nM 5 and 10 years after BPD, respectively. Whole-body glucose uptake increased from 24.27 [+ or -] 4.44 at the baseline to 57.29 [+ or -] 11.56 and 57.71 [+ or -] 8.41 micromol/kgfat free mass per minute 5 and 10 years after BPD, respectively (p = 0.001). Predictor of 25(OH)D was fat mass (R2 = 0.26,p = 0.0001 in obesity; R2 = 0.20,p = 0.0001) and BMI correlated with fat mass (R2 = 0.19; p = 0.0001) and BMI (R2 = 0.053;p = 0.01) and inversely with M value (R2 = 0.16;p= 0.0001), but only in obese subjects.
Low vitamin D levels were observed in morbidly obese individuals both before and after BPD. Low 25(OH)D did not imply increased insulin resistance after BPD, a condition where, probably, more powerful determinants of insulin sensitivity overcome the low circulating 25(OH)D levels. However, researchers feel that this data cannot exclude some kind of influence of vitamin D status on glucose and insulin metabolism.
M. Manco, M. Calvani, G. Nani, et al. Low 25-hydroxyvitamin D does not affect insulin sensitivity in obesity after bariatrie surgery. Obes Res; 13:1692-1700 (October 2005). [Correspondence: Melania Manco, Department of Internal Medicine and Surgery, Catholic University, School of Medicine, 484 Pineta Sacchetti, 00168 Rome, Italy. E-mail: melania.manco@rm.tmicatt.it].
COPYRIGHT 2005 Frost & Sullivan
COPYRIGHT 2006 Gale Group