Vitamin D deficiency is a problem of considerable magnitude that has reemerged as a major public health issue in the United States and several other developed countries. Vitamin D plays a crucial role in calcium homeostasis in the body. Hypovitaminosis D leads to osteomalacia and increased risk of fractures, especially in the elderly. Preliminary research suggests that vitamin D can prevent certain types of cancer and autoimmune diseases. A recent large study has shown the association between severe hypovitaminosis D and persistent, non-specific musculo-skeletal pain, further suggesting that patients with no apparent cause of pain should be assessed and possibly treated for vitamin D deficiency.
Key words: hypovitaminosis D, 1,25-dihydroxyvitamin D, osteomalacia, myopathy, musculoskeletal pain
© 2004 International Life Sciences Institute
doi: 10.1301/nr.2004.sept.354-359
Vitamin D deficiency has plagued mankind for centuries. Indeed, the deficiency of vitamin D was epidemic in most industrialized nations throughout Northern Europe and the United States by the end of the 19th century.1 Severe deficiency of vitamin D manifested itself as rickets in children and osteomalacia in adults. It was thought that children and the elderly were particularly at risk for vitamin D deficiency. The appreciation of the role of vitamin D and sunlight in preventing rickets and the fortification of milk with vitamin D played a major role in the eradication of rickets.1,2 However, the strong public health messages promoting exclusive breastfeeding of infants and urging the avoidance of sun exposure have been associated with a resurgence of rickets, especially in young African-American children.1,3
There is an alarmingly high prevalence of vitamin D deficiency in the United States and Canada.4,5 Several studies have demonstrated the prevalence of vitamin D deficiency to be between 25% and 54% in patients older than 65 years.6 A myriad of factors comes into play when determining the prevalence of vitamin D deficiency in a population. These include the effects of season, latitude, age, and skin pigmentation, as well as social and cultural differences.7,8 Both in the northern and southern hemispheres, countries above a latitude of 42 degrees north and 42 degrees south have a higher prevalence of vitamin D deficiency.4
Although elderly, institutionalized, and disabled individuals are far more prone to developing vitamin D deficiency,9 several studies have shown a large number of younger individuals with this deficiency.10,11 Season plays a role in determining the prevalence of vitamin D deficiency, with a higher number of cases in winter and fall.7,12 Europeans have a high prevalence of vitamin D deficiency, which is even more prevalent in immigrants to these countries.13-16 Australia too has reported a high prevalence of vitamin D deficiency, especially among immigrants.17,18 The reasons for this phenomenon are multifactoral and include low intake of calcium and vitamin D, minimal exposure to sunlight, skin pigmentation, and high parity. Unfortunately, even people living in sunny countries are not exempt from vitamin D deficiency; reasons for this are cultural, including vegetarianism and type of clothing worn.19 African Americans and people with darker complexions are particularly prone to vitamin D deficiency because a higher melanin content in the skin is associated with lower cutaneous synthesis of vitamin D.20,21 In addition, strong lobbying efforts by public health experts and dermatologists to reduce sunlight exposure and widespread use of sunscreen play a contributory role.1,7 Certain disease states, such as chronic renal failure and severe liver failure, cause substantial reductions in serum vitamin D-binding protein, which lowers the serum 25-hydroxyvitamin D concentration. Intestinal malabsorption of digested fats causes loss of fat-soluble vitamins, including vitamin D, thereby leading to deficiency. In addition, the use of certain drugs such as rifampin, phenytoin, and carbamazepine impair vitamin D activation or accelerate its clearance, contributing further to deficiency.11
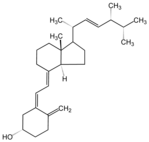
Vitamin D is converted in the body to a steroid hormone that is essential to the development, growth, and maintenance of a healthy skeleton as well as to calcium homeostasis.1 Vitamin D is obtained from the diet, predominantly from fatty fish such as salmon, fortified foods, and dietary supplements. Because fortification of food with vitamin D is unreliable, skin synthesis is thought to be the major contributor.4,6 The majority of vitamin D is manufactured when ultraviolet B (UVB) light with a wavelength of 290-315 nanometers hits a precursor molecule (7-dehydrocholesterol) in the skin.1,4 Previtamin D is formed and is spontaneously converted to vitamin D, which is transported to the liver, where it is converted to 25-hydroxyvitamin D (calcidiol). In the kidneys, 25-hydroxyvitamin D is converted to the active metabolite 1,25-dihydroxyvitamin D (calcitriol), which, together with parathyroid hormone (PTH), regulates calcium levels in the body and influences skeletal calcium resources (Figure 1). Apart from the kidneys, several other tissues, including breast, prostate, and colon, can make 1,25-dihydroxyvitamin D to maintain cell health.
The Food and Nutrition Board (FNB) issued guidelines22 (last published in 1997) for the adequate daily intake of vitamin D. Although it is well established that the recommended 200 international units (IU) per day prevents rickets in children, the "adequate intake" for adults-namely 200 IU per day for people 19 to 50 years old, 400 IU per day for people 51 to 70 years old, and 600 IU per day for people older than 70 years-has now been deemed insufficient.23 In an elegant study published by Heaney et al.,24 it was estimated that people who can't or don't go outdoors may need supplementation of as much as 3000 to 5000 IU per day to maintain an adequate serum 25-hydroxyvitamin D concentration in the absence of substantial cutaneous production of vitamin D.
Plasma 25-hydroxyvitamin D is the best clinical indicator of vitamin D status because it represents the combined contribution from cutaneous synthesis and dietary intake of vitamin D.4 It is well established that the lower limit of the normal range for 25-hydroxyvitamin D (15 ng/mL) is insufficient to maintain adequate skeletal integrity.11 There is strong evidence to show that a serum level of at least 20 ng/mL of 25-hydroxyvitamin D is required to maintain calcium homeostasis without developing secondary hyperparathyroidism. In fact, adults over 49 years old may require a serum 25-hydroxyvitamin D level of at least 50 nmol/L to achieve the optimum parathyroid hormone levels.25
Vitamin D is essential for skeletal health, and severe deficiency is associated with defective mineralization of skeletal tissue, leading to rickets in children or its equivalent, osteomalacia, in adults. More subtle levels of vitamin D insufficiency can lead to secondary hyperparathyroidism and increased bone turnover, both of which play a critical role in age-related bone loss and osteoporotic fractures. When circulating levels of 25-hydroxyvitamin D remain chronically low (
The association of pain with hypovitaminosis D as the initial presentation in children with rickets was first described in Kashmir, the northernmost Indian state.27 Of the 100 children studied, 85% did not have the clinical features of rickets, but all of the children had elevated serum alkaline phosphatase and persistent pain in their lower extremities. Dietary vitamin D deficiency and inadequate exposure to sun were causal factors. Initiation of vitamin D therapy relieved lower extremity pain and normalized serum alkaline phosphatase levels. In 1991, Gloth et al.28 described an unusual pain syndrome in five patients with vitamin D deficiency. The pain had a hyperesthetic quality and did not respond to analgesics, including opiate derivatives or tricyclic antidepressants. The pain resolved promptly and dramatically with the administration of ergocalciferol, and the patients also demonstrated improved vitamin D status. A few case reports have demonstrated the pain of osteomalacic myopathy in vitamin D-deficient patients.16,29 A case series in Western New York by Prabhala et al.30 demonstrated severe myopathy associated with vitamin D deficiency. The patients in this series experienced prompt resolution of their pain and muscle weakness after vitamin D therapy. A study of 360 patients in Saudi Arabia showed that vitamin D deficiency is a major contributor to lower back pain.31 Although Saudi Arabia enjoys a sunny climate throughout the year, excessive heat and cultural issues such as the clothing worn by Muslim women, together with the burden of pregnancy and lactation, lead to the endemic status of vitamin D deficiency manifested as chronic lower back pain.
The largest cross-sectional study demonstrating the association of persistent, nonspecific musculoskeletal pain with severe hypovitaminosis D was recently carried out by Plotnikoff and Quigley.32 One hundred and fifty patients in a large community university health center in Minneapolis, Minnesota (45 degrees North), were recruited for this study. The subjects represented six ethnic groups, and were broadly divided into immigrant (83 patients) and nonimmigrant (67 patients) categories. The immigrant ethnic groups were East African (Somalian), Hispanic (Mexican), and South Asian (Hmong, Cambodian, or Laotian). The nonimmigrant ethnic groups were African American (sub-Saharan, Central, and West African), white (Scandinavian and Northern European), and American Indian (Lakotan, Dakotan, and Ojibwe). The study was carried out between February 2000 and June 2002 in patients between the ages of 10 and 65 years old.
The patients had persistent, nonspecific musculoskeletal pain. None had been diagnosed with fibromyalgia, temporomandibular disorder, or complex regional pain syndrome. The patients had no medical condition that would decrease the production, absorption, or hydroxylation of vitamin D or cause the increased clearance or decreased action of its active metabolite, 1,25-dihydroxyvitamin D. Two of the patients were seropositive for hepatitis C but had normal serum transaminases, two patients had a history of prednisone use, and two were using inhaled corticosteroids. All of the patients had previously tried over-the-counter and prescription analgesics without relief. Less than 10% were taking vitamin D supplements, and more than 90% had been evaluated for their persistent musculoskeletal pain one year or more before recruitment. None of the patients had been tested previously for hypovitaminosis D. Serum 25-hydroxyvitamin D levels were obtained by radio immunoassay.
Deficiency was characterized as profound if the 25-hydroxyvitamin D levels were 4 ng/mL or less; severe if the levels were 5 to 8 ng/mL; moderately severe if the levels were 9 to 12 ng/mL; moderate if the levels were 13 to 16 ng/mL; and marginal if the levels were 17 to 20 ng/mL. The cutoff level of less than 3 ng/mL was considered equal to 2 ng/mL for analysis. Results were evaluated for statistical significance with Student's t tests and analysis of variance (ANOVA) tests. Seasons were defined by the solar calendar. Normal childbearing age was defined as 36 years or younger. The calculated coefficient of variation (interassay and intra-assay) was 10%.
The prevalence of hypovitaminosis D in this population of non-elderly, non-housebound outpatients with persistent, nonspecific musculoskeletal pain refractory to standard pharmaceutical therapy was 93% (140/150, mean 12.8 ng/mL; 95% confidence interval [CI], 11.18-12.99 ng/mL). One hundred percent of African-American, East-African, Hispanic, and American-Indian patients had deficient levels of vitamin D (
The Plotnikoff and Quigley study32 is important because it showed that in the United States, the risk of hypovitaminosis D is not bound to traditional risk categories such as children and the elderly. It is of concern to see that more than 90% of patients in this study had deficient levels of serum 25-hydroxyvitamin D. The mean value of 12.8 ng/mL was between the moderately severe and the moderately deficient range. Similar mean serum 25-hydroxyvitamin D concentrations were seen across all groups of the study, regardless of immigrant status, sex, race, or season. By contrast, younger patients were significantly more deficient in vitamin D than older patients. Women of childbearing age had moderately severe vitamin D deficiency, and nearly half of them had severe or profoundly deficient levels. The possibility of osteomalacia as a diagnosis was not suspected in these patients despite extensive contact with the health care system.
The authors point out that this study had several limitations. First, age-, sex-, and ethnically matched control patients were not recruited for comparison. second, the study was conducted at a single center in Minnesota (45 degrees north) where the prevalence of hypovitaminosis D may be large. Third, the value of what constitutes "normal" serum 25-hydroxyvitamin D levels-20 ng/mL for the purposes of this study-was based on data from previous studies that were biologically based rather than population based. Serum calcium, phosphorus, osteocalcin, alkaline phosphatase, cyclic adenosine monophosphate, and urinary calcium and phosphate levels were not determined, and no bone densitometry or roentrographic study was done. Fourth, the serum 25-hydroxyvitamin D level was reported only once in the study, which cannot reflect the duration of deficiency. Finally, there was no intervention done in this study to increase 25-hydroxyvitamin D levels, hence it is unclear whether the musculoskeletal pain experienced by these patients was secondary to their low vitamin D states.
Our review suggests that physicians may be wise to suspect hypovitaminosis D in patients with persistent nonspecific musculoskeletal pain. This is especially true for patients from areas with prolonged winter and relative lack of and/or exposure to sunshine. In addition, given the relatively high prevalence of hypovitaminosis D, physicians should consider the possibility of this deficiency in all patients with any cause of intestinal malabsorption, including inflammatory bowel disease, celiac disease, and pancreatic insufficiency, as well as patients with chronic renal failure.11,30
1. Holick MF. Vitamin D: a millennium perspective. J Cell Biochem. 2003;88:296-307.
2. Gannage-Yared MH, Tohme A, Halaby G. Hypovitaminosis D: a major worldwide public health problem [in French]. Presse Med. 2001;30:653-658.
3. Kreiter SR, Schwartz RP, Kirkman HN Jr, Charlton. PA, Calikoglu AS, Davenport ML. Nutritional rickets in African American breast-fed infants. J Pediatr. 2000;137:153-157.
4. Calvo MS, Whiting SJ. Prevalence of vitamin D insufficiency in Canada and the United States: importance to health status and efficacy of current food fortification and dietary supplement use. Nutr Rev. 2003;61:107-113.
5. Rucker D, Allan JA, Fick GH, Hanley DA. Vitamin D insufficiency in a population of healthy western Canadians. CMAJ. 2002;166:1517-1524.
6. McKenna MJ. Differences in vitamin D status between countries in young adults and the elderly. Am J Med. 1992:93:69-77.
7. Norman AW. Sunlight, season, skin pigmentation, vitamin D, and 25-hydroxyvitamin D: integral components of the vitamin D endocrine system. Am J Clin Nutr. 1998;67:1108-1110.
8. Gloth FM 3rd, Gundberg CM, Hollis BW, Haddad JG Jr, Tobin JD. Vitamin D deficiency in homebound elderly persons. JAMA. 1995;274:1683-1686.
9. Semba RD, Garrett E, Johnson BA, Guralnik JM, Fried LP. Vitamin D deficiency among older women with and without disability. Am J Clin Nutr. 2000;72: 1529-1534.
10. Tangpricha V, Pearce EN, Chen TC, Holick MF. Vitamin D insufficiency among free-living healthy young adults. Am J Med. 2002;112:659-662.
11. Thomas MK, Lloyd-Jones DM, Thadhani RI, et al. Hypovitaminosis D in medical inpatients. N Engl J Med. 1998:338:777-783.
12. Margiloff L, Harris SS, Lee S, Lechan R, Dawson-Hughes B. Vitamin D status of an outpatient clinic population. Calcif Tissue Int. 2001;69:263-267.
13. Kauppinen-Makelin R, Tahtela R, Loyttyniemi E, Karkkainen J, Valimaki MJ. A high prevalence of hypovitaminosis D in Finnish medical in- and outpatients. J Intern Med. 2001;249:559-563.
14. Serhan E, Newton P, Ali HA, Walford S, Singh BM. Prevalence of hypovitaminosis D in Indo-Asian patients attending a rheumatology clinic. Bone. 1999; 25:609-611.
15. Datta S, Alfaham M, Davies DP, et al. Vitamin D deficiency in pregnant women from a non-European ethnic minority population-an interventional study. BJOG. 2002;109:905-908.
16. Nellen JF, Smulders YM, Jos Frissen PH, Slaats EH, Silberbusch J. Hypovitaminosis D in immigrant women: slow to be diagnosed. BMJ. 1996;312: 570-572.
17. Diamond TH, Levy S, Smith A, Day P. High bone turnover in Muslim women with vitamin D deficiency. Med J Aust. 2002;177:139-141.
18. Skull SA, Ngeow JY, Biggs BA, Street A, Ebeling PR. Vitamin D deficiency is common and unrecognized among recently arrived adult immigrants from The Horn of Africa. Intern Med J. 2003;33:47-51.
19. Gannage-Yared MH, Chemali R, Yaacoub N, Halaby G. Hypovitaminosis D in a sunny country: relation to lifestyle and bone markers. J Bone Miner Res. 2000:15:1856-1862.
20. Nesby-O'Dell S, Scanlon KS, Cogswell ME, et al. Hypovitaminosis D prevalence and determinants among African American and white women of reproductive age: third National Health and Nutrition Examination Survey, 1988-1994. Am J Clin Nutr. 2002:76:187-192.
21. Perry HM 3rd, Miller DK, Morley JE, et al. A preliminary report of vitamin D and calcium metabolism in older African Americans. J Am Geriatr Soc. 1993; 41:612-616.
22. Institute of Medicine, National Academies. Dietary Reference Intakes for Calcium, Phosphorus, Magnesium, Vitamin D and Fluoride. Washington, DC: National Academies Press; 1997:250-287.
23. Utiger RD. The need for more vitamin D. N Engl J Med. 1998;338:828-829.
24. Heaney RP, Davies KM, Chen TC, Holick MF, Barger-Lux MJ. Human serum 25-hydroxycholecalciferol response to extended oral dosing with cholecalciferol. Am J Clin Nutr. 2003:77:204-210.
25. Malabanan A, Veronikis IE, Holick MF. Redefining vitamin D insufficiency. Lancet. 1998;351:805-806.
26. Glerup H, Mikkelsen K, Poulsen L, et al. Hypovitaminosis D myopathy without biochemical signs of osteomalacic bone involvement. Calcif Tissue Int. 2000;66:419-424.
27. Masood H, Narang AP, Bhat IA, Shah GN. Persistent limb pain and raised serum alkaline phosphatase the earliest markers of subclinical hypovitaminosis D in Kashmir. Indian J Physiol Pharmacol. 1989; 33:259-261.
28. Gloth FM 3rd, Lindsay JM, Zelesnick LB, Greenough WB 3rd. Can vitamin D deficiency produce an unusual pain syndrome? Arch Intern Med. 1991;151:1662-1664.
29. Russell JA. Osteomalacic myopathy. Muscle Nerve. 1994;17:578-580.
30. Prabhala A, Garg R, Dandona P. Severe myopathy associated with vitamin D deficiency in western New York. Arch Intern Med. 2000;160:1199-1203.
31. Al Faraj S, Al Mutairi K. Vitamin D deficiency and chronic low back pain in Saudi Arabia. Spine. 2003; 28:177-179.
32. Plotnikoff GA, Quigley JM. Prevalence of severe hypovitaminosis D in patients with persistent, nonspecific musculoskeletal pain. Mayo Clin Proc. 2003;78:1463-1470.
This review was prepared by Ranjan Mascarenhas, C.V., M.D., and Sohrab Mobarhan, M.D. Dr. Mascarenhas is with the Department of Internal Medicine and Dr. Mobarhan is with the Department of Internal Medicine and the Division of Gastroenterology, Hepatology and Nutrition, Loyola University Medical Center, Maywood, IL 60153.
Copyright International Life Sciences Institute and Nutrition Foundation Sep 2004
Provided by ProQuest Information and Learning Company. All rights Reserved