Definition
Lymphadenitis is the inflammation of a lymph node. It is often a complication of a bacterial infection of a wound, although it can also be caused by viruses or other disease agents. Lymphadenitis may be either generalized, involving a number of lymph nodes; or limited to a few nodes in the area of a localized infection. Lymphadenitis is sometimes accompanied by lymphangitis, which is the inflammation of the lymphatic vessels that connect the lymph nodes.
Description
Lymphadenitis is marked by swollen lymph nodes that are painful, in most cases, when the doctor touches them. If the lymphadenitis is related to an infected wound, the skin over the nodes may be red and warm to the touch. If the lymphatic vessels are also infected, there will be red streaks extending from the wound in the direction of the lymph nodes. In most cases, the infectious organisms are hemolytic Streptococci or Staphylococci. Hemolytic means that the bacteria produce a toxin that destroys red blood cells.
The extensive network of lymphatic vessels throughout the body and their relation to the lymph nodes helps to explain why bacterial infection of the nodes can spread rapidly to or from other parts of the body. Lymphadenitis in children often occurs in the neck area because these lymph nodes are close to the ears and throat, which are frequent locations of bacterial infections in children.
Causes & symptoms
Streptococcal and staphylococcal bacteria are the most common causes of lymphadenitis, although viruses, protozoa, rickettsiae, fungi, and the tuberculosis bacillus can also infect the lymph nodes. Diseases or disorders that involve lymph nodes in specific areas of the body include rabbit fever (tularemia), cat-scratch disease, lymphogranuloma venereum, chancroid, genital herpes, infected acne, dental abscesses, and bubonic plague. In children, tonsillitis or bacterial sore throats are the most common causes of lymphadenitis in the neck area. Diseases that involve lymph nodes throughout the body include mononucleosis, cytomegalovirus infection, toxoplasmosis, and brucellosis.
The early symptoms of lymphadenitis are swelling of the nodes caused by a buildup of tissue fluid and an increased number of white blood cells resulting from the body's response to the infection. Further developments include fever, often as high as 101-102°F (38-39°C) together with chills, loss of appetite, heavy perspiration, a rapid pulse, and general weakness.
Diagnosis
Physical examination
The diagnosis of lymphadenitis is usually based on a combination of the patient's history, the external symptoms, and laboratory cultures. The doctor will press (palpate) the affected lymph nodes to see if they are sore or tender. Swollen nodes without soreness are often caused by cat-scratch disease. In children, the doctor will need to rule out mumps, tumors in the neck region, and congenital cysts that resemble swollen lymph nodes.
Although lymphadenitis is usually diagnosed in lymph nodes in the neck, arms, or legs, it can also occur in lymph nodes in the chest or abdomen. If the patient has acutely swollen lymph nodes in the groin, the doctor will need to rule out a hernia in the groin that has failed to reduce (incarcerated inguinal hernia). Hernias occur in 1% of the general population; 85% of patients with hernias are male.
Laboratory tests
The most significant tests are a white blood cell count (WBC) and a blood culture to identify the organism. A high proportion of immature white blood cells indicates a bacterial infection. Blood cultures may be positive, most often for a species of staphylococcus or streptococcus. In some cases, the doctor may order a biopsy of the lymph node.
Treatment
Medications
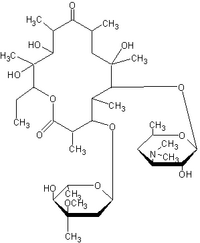
The medications given for lymphadenitis vary according to the bacterium or virus that is causing it. If the patient also has lymphangitis, he or she will be treated with antibiotics, usually penicillin G (Pfizerpen, Pentids), nafcillin (Nafcil, Unipen), or cephalosporins. Erythromycin (Eryc, E-Mycin, Erythrocin) is given to patients who are allergic to penicillin.
Supportive care
Supportive care of lymphadenitis includes resting the affected limb and treating the area with hot moist compresses.
Surgery
Cellulitis associated with lymphadenitis should not be treated surgically because of the risk of spreading the infection. Pus is drained only if there is an abscess and usually after the patient has been started on antibiotic treatment. In some cases, a biopsy of an inflamed lymph node is necessary if no diagnosis has been made and no response to treatment has occurred.
Prognosis
The prognosis for recovery is good if the patient is treated promptly with antibiotics. In most cases, the infection can be brought under control in three or four days. Patients with untreated lymphadenitis may develop blood poisoning (septicemia), which is sometimes fatal.
Prevention
Prevention of lymphadenitis depends on prompt treatment of bacterial and viral infections.
Key Terms
- Hemolytic
- Able to break down or dissolve red blood cells. The bacteria that cause lymphadenitis are hemolytic.
- Hernia
- The bulging of a part of the intestine or other organ through its surrounding wall of tissue. Most hernias are in the abdominal cavity. An inguinal hernia is located in the groin area.
- Lymph nodes
- The glandlike masses of tissue in the lymphatic system that contain lymphocytes. The lymph nodes also filter lymph, which is a clear yellowish tissue fluid that carries lymphocytes and fats throughout the body.
- Lymphangitis
- Inflammation of the lymphatic vessels. It often occurs together with lymphadenitis.
- Septicemia
- The presence of bacteria and their toxins in the bloodstream. Septicemia is sometimes called blood poisoning.
- Any of several species of spherical bacteria that occur in groups of four or irregular clusters. frequently cause skin infections.
- Any of several species of bacteria that are spherical in shape and form pairs or chains. cause scarlet fever, tonsillitis, and pneumonia, and are often involved in lymphadenitis.
Further Reading
For Your Information
Books
- Berman, Stephen, and Ken Chan. "Ear, Nose, & Throat." In Current Pediatric Diagnosis & Treatment, edited by William W. Hay, Jr., et al. Stamford, CT: Appleton & Lange, 1997.
- Grossi, Carlo E., and Peter M. Lydyard. "Lymph Nodes." In Encyclopedia of Immunology, vol. II, edited by Ivan M. Roitt, and Peter J. Delves. London: Academic Press, 1992.
- Hall, Joseph G. "Lymphatic System." In Encyclopedia of Immunology, vol. II, edited by Ivan M. Roitt, and Peter J. Delves. London: Academic Press, 1992.
- "Infectious Disease: Superficial Infections." In The Merck Manual of Diagnosis and Therapy, vol. I, edited by Robert Berkow, et al. Rahway, NJ: Merck Research Laboratories, 1992.
- Tierney, Lawrence M., Jr. "Blood Vessels & Lymphatics." In Current Medical Diagnosis & Treatment 1998, edited by Lawrence M. Tierney, Jr., et al. Stamford, CT: Appleton & Lange, 1997.
Gale Encyclopedia of Medicine. Gale Research, 1999.