Pertussis, or whooping cough, is a highly contagious respiratory illness caused by Bordetella pertussis. Outbreaks of the disease are now occurring every three to four years in highly immunized populations throughout the United States and are a significant health threat despite widespread vaccination and effective therapy. Unfortunately, pertussis vaccine provides only transient protection. Infected adults and adolescents with mild disease are the reservoir for more severe infection in infants and young children.
Family physicians can reduce the morbidity and mortality of pertussis and help to control outbreaks through primary vaccination, early diagnosis, antibiotic therapy and prophylaxis, and case reporting to public health authorities. The Advisory Committee on Immunization Practices has recently changed its recommendations to include use of acellular pertussis preparations in children as part of the primary vaccination series against diphtheria, pertussis and tetanus (DPT). The revised recommendations are included in this review of the epidemiology, clinical characteristics, laboratory diagnosis, therapy and outbreak control strategies for pertussis.
Epidemiology
Pertussis has been a reportable disease in the United States since 1922. The number of pertussis cases in this country peaked in 1938 at 260,000. After the whole-cell pertussis vaccine was licensed in 1949, these numbers dropped dramatically to a historic low of 1,010 cases in 1976. During the past decade, an average of 2,900 cases and five to six deaths have been reported annually.[1,2] Pertussis outbreaks have occurred cyclically since the early 1980s, with large increases in incidence in 1983, 1986, 1990 and 1993.[3] The incidence of pertussis in the United States continues to rise: 6,467 cases were reported in 1996. The disease is also a significant cause of morbidity and mortality worldwide.[4]
Pathophysiology
Pertussis is caused by the gram-negative bacillus B. pertussis, a strict anaerobe whose only known reservoir is humans. B. pertussis produces many biologically activesubstances that are thought to be responsible for its clinical syndrome; the most significant of these substances are pertussis toxin and filamentous hemagglutinin. Transmission is by aerosolized droplets containing organisms coughed by infected persons. The incubation period is usually six to 10 days but ranges from five to 21 days. Infected persons can transmit the disease after the first week of incubation and remain infectious until three weeks after the onset of symptoms. Pertussis has no distinct seasonal pattern.
Clinical Characteristics
The clinical course of pertussis infection is divided into three stages: catarrhal, paroxysmal and convalescent (Table 1). The catarrhal stage lasts one to two weeks and consists of mild upper respiratory infection symptoms with progressive cough. Because the early symptoms are minimal, the diagnosis of pertussis is rarely considered during this stage. However, the recovery rates of viable organisms and positive cultures are highest at this time.
DIRECT FLUORESCENT ANTIBODY TESTS
The direct fluorescent antibody (DFA) test, performed on nasopharyngeal smears, is also used to diagnose pertussis. DFA is a rapid test and has a higher positive predictive value when used in outbreak investigations.[13] Interpretation of the test requires an experienced reader and is made difficult by cross-reacting antigens found on other nasopharyngeal organisms. The DFA test has variable sensitivity and specificity, and is not totally reliable when used alone.[1,4] Results are available within one day and are useful in the diagnosis, but the possibility of false-positive results requires continued attempts at culture confirmation of all suspected cases.[13]
SEROLOGY
Pertussis serology is currently available from microbiology reference laboratories and can provide support in the diagnosis of suspected cases of pertussis. Serology is of questionable value because the natural history of pertussis immunity is not fully understood. The sensitivity of serologic diagnosis can exceed that of culture. In one study,[14] serology was found to have a sensitivity of 87 percent in the diagnosis of pertussis. However, this degree of sensitivity is reached only when both acute and convalescent serum specimens are obtained, and requires assays of three different Ig subclasses versus two different pertussis antigens.
Currently, no single test offers acceptable sensitivity and specificity in the diagnosis of pertussis. One reason is that reliable reference values for serologic titers have not been established. Another is that multiple subclasses of antipertussis immunoglobulin, with widely varying half-lives, are produced in response to both vaccination and natural infection. This precludes distinguishing between natural infection and vaccination with a single serum specimen. With further understanding of pertussis immunity, including the serologic correlates of protection and the establishment of accurate reference values, serologic diagnosis of pertussis may be possible with a minimum of assays and specimens.
In summary, the diagnosis of pertussis is generally based on clinical history with supporting, frequently nonspecific, laboratory data. Laboratory tools are limited by the pathophysiology of pertussis infection, technologic shortfalls and an incomplete understanding of pertussis immunity.
Management
Optimal management of pertussis during an outbreak includes complete immunization of all susceptible children; a high index of suspicion for the disease; early recognition and treatment of infected persons and contacts, and case reporting to public health authorities.
ANTIBIOTIC THERAPY
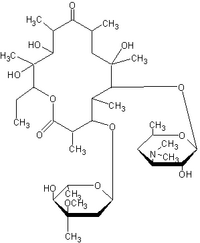
Erythromycin (E-mycin, Eryc, Ery-Tab) is the drug of choice at any clinical stage of pertussis (Table 3). Five days of erythromycin therapy will reliably eradicate organisms, but a 10 percent relapse rate occurs with treatment courses of less than 14 days.[2,11] Some experts prefer to use the erythromycin estolate preparation (Ilosone), because higher blood levels are produced. Erythromycin shortens the course of illness when administered early.[8,15] After the onset of the paroxysmal stage of pertussis, antibiotics do not alter the clinical course, but they can clear the organism from the nasopharynx and thus limit the spread of disease.[16] Trimethoprim-sulfamethoxazole (Bactrim, Septra) is an effective alternative for patients who cannot tolerate erythromycin. Preliminary information, not supported by controlled clinical trials, suggests that other potentially effective alternatives may be azithromycin (Zithromax) or clarithromycin (Biaxin).[17]
The acellular DTaP vaccine is now recommended for use interchangeably with the whole-cell preparation in all patients for the entire primary vaccination series, because DTaP has greater efficacy and causes fewer side effects than the whole-cell DTP. In the near future, the acellular preparation is likely to be used exclusively in the primary vaccination series.
Local pain reactions and fever are common occurrences following whole-cell DTP administration and can be controlled with acetaminophen. These reactions are less frequent with DTaP administration, but acetaminophen can be used if needed. Although whole-cell DTP vaccine has never been proved to cause serious neurologic illness, several epidemiologic studies have demonstrated that the vaccine, in rare cases, is associated with acute encephalopathy. The estimated risk of this adverse event is zero to 10.5 episodes per 1 million vaccinations.[26] The only contraindications to vaccination are immediate anaphylaxis or encephalopathy occurring within seven days of vaccine administration and not due to another identifiable cause.[27]
Vaccination also controls the spread of disease during an outbreak. Infants should be given DPT or DTaP vaccine on an accelerated schedule during outbreaks. This should begin at age four weeks with vaccination again at six, 10 and 14 weeks of age.[28] All exposed children under age seven who have not received all four doses in the primary series should complete the series at the minimum intervals. Those under age seven who have completed the primary series but have not received a dose of DTP or DTaP vaccine within three years prior to exposure should be given a booster dose.[1] Children who have a history of pertussis, either culture-positive disease or typical symptoms with an epidemiologic link to a culture-proved case, do not need additional pertussis vaccination.[26]
Immunization of adolescents and adults is controversial. Since infected persons in these groups are the usual source of infection in younger children, several authors have suggested that new immunization programs should include regularly scheduled booster doses for adolescents and adults, using acellular vaccine preparations.[29] However, routine booster immunization of adolescents and adults is not currently recommended. Although the new acellular vaccines are safe and effective,[30,31] their long-term efficacy has not been established. The development of more effective primary vaccination in childhood may be the most prudent and cost-effective way to decrease the reservoir of pertussis infection.
The opinions and assertions contained herein are the private views of the authors and are not to be construed as official or as reflecting the views of the Army Medical Department or the Army Service at large.
REFERENCES
[1.] Atkinson W, Furphy L, Gant J, Mayfield M. Pertussis. In: Epidemiology and prevention of vaccine-preventable diseases. Atkinson W, et al., eds. 2d ed. Atlanta, Gal: Centers for Disease Control and Prevention, Department of Health and Human Services, 1995:57-72.
[2.] Centers for Disease Control and Prevention. Summary of notifiable diseases, United States 1994. MMWR Morb Mortal Wkly Rep 1994;43:1-80.
[3.] Centers for Disease Control and Prevention. Pertussis--United States, January 1992-June 1995. MMWR Morb Mortal Wkly Rep 1995;44:525-9.
[4.] Muller AS, Leeuwenburg J, Pratt DS. Pertussis: epidemiology and control. Bull World Health Organ 1986:64:321-31.
[5.] Feigin RD, Cherry JD, eds. Pertussis. In: Textbook of pediatric infectious diseases. 3d ed. Philadelphia: Saunders, 1992:1208-18.
[6.] Sprauer MA, Cochi SL, Zell ER, Sutter RW, Mullen JR, Englender SJ, et al. Prevention of secondary transmission of pertussis in households with early use of erythromycin. Am J Dis Child 1992;146:177-81.
[7.] Bortolussi R, Miller B, Ledwith M, Halperin S. Clinical course of pertussis in immunized children. Pediatr Infect Dis J 1995;14:870-4.
[8.] Bass JW. Pertussis: current status of prevention and treatment. Pediatr Infect Dis 1985;4:614-9.
[9.] Farizo KM, Cochi SL, Zell ER, Brink EW, Wassilak SG, Patriarca PA. Epidemiological features of pertussis in the United States, 1980-1989. Clin Infect Dis 1992;14:708-19.
[10.] Postels-Multani S, Schmitt HJ, Wirsing von Konig CH, Bock HL, Bogaerts H. Symptoms and complications of pertussis in adults. Infection 1995;23:139-42.
[11.] Feigin RG. Pertussis (whooping cough). In: Berman RE, Kliegman RM, Nelson WE, Vaughan VC III, eds. Nelson textbook of pediatrics. 14th ed. Philadelphia: Saunders, 1992:724-5.
[12.] Patriarca PA, Biellik RJ, Sanden G, Burstyn DG, Mitchell PD, Silverman PR, et al. Sensitivity and specificity of clinical case definitions for pertussis. Am J Public Health 1988;78:833-6.
[13.] Onorato IM, Wassilak SG. Laboratory diagnosis of pertussis: the state of the art. Pediatr Infect Dis J 1987;6:145-51.
[14.] Halperin SA, Bortolussi R, Wort AJ. Evaluation of culture, immunofluorescence, and serology for the diagnosis of pertussis. J Clin Microbiol 1989;27:752-7.
[15.] Bergquist SO, Bernander S, Dahnsjo H, Sundelof B. Erythromycin in the treatment of pertussis: a study of bacteriologic and clinical effects. Pediatr Infect Dis J 1987;6:458-61 [Published erratum appears in Pediatr Infect Dis J 1987;6:1035].
[16.] Statement on management of persons exposed to pertussis and pertussis outbreak control. Can Commun Dis Rep 1994;20:193-200.
[17.] Alexander ER, Debolt C. Pertussis alert. Seattle-King County Department of Public Health; July 1996:1-5.
[18.] Badr-El-Din MK, Aref GH, Kassem AS, Abdel-Moneim MA, Abbassy AA. A beta-adrenergic stimulant, salbutamol, in the treatment of pertussis. J Trop Med Hyg 1976;79:218-9.
[19.] Pavesio D, Ponzone A. Salbutamol and pertussis [Letter]. Lancet 1977;1(8003):150-1.
[20.] Peltola H, Michelsson K. Efficacy of salbutamol in treatment of infant pertussis demonstrated by sound spectrum analysis. Lancet 1982;1(8267):310-2.
[21.] Chandra H, Rao CS, Karan S, Mathur YC. Evaluation of betamethasone and isoniazid along with chloramphenicol in the management of whooping cough. Indian Pediatr 1972;9:70-3.
[22.] Zoumboulakis D, Anagnostakis K, Albanis V, et al. Steroids in treatment of pertussis. A controlled clinical trial. Arch Dis Child 1973;48:51-4.
[23.] American Academy of Pediatrics. Pertussis. In: 1994 Red book: report of the Committee on Infectious Diseases. 23rd ed. Elk Grove Village, Ill.: American Academy of Pediatrics, 1994:356.
[24.] De Serres G, Boulianne N, Duval B. Field effectiveness of erythromycin prophylaxis to prevent pertussis within families. Pediatr Infect Dis J 1995; 14:969-75.
[25.] Steketee RW, Wassilak SG, Adkins WN Jr, Burstyn DG, Manclark CR, Berg J, et al. Evidence for a high attack rate and efficacy of erythromycin prophylaxis in a pertussis outbreak in a facility for the developmentally disabled. J Infect Dis 1988;157:434-40.
[26.] Centers for Disease Control and Prevention. Update: Vaccine side effects, adverse reactions, contraindications, and precautions-recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Morb Mortal Wkly Rep 1996; 45(RR-12):22-31.
[27.] Centers for Disease Control and Prevention. Diphtheria, tetanus, and pertussis: recommendations for vaccine use and other preventive measures. Recommendations of the Immunization Practices Advisory Committee (ACIP). MMWR Morb Mortal Wkly Rep 1991;40:1-28.
[28.] Onorato IM, Wassilak SG, Meade B. Efficacy of whole-cell pertussis vaccine in preschool children in the United States. JAMA 1992;267:2745-9.
[29.] Cherry JD. Nosocomial pertussis in the nineties [Editorial]. Infect Control Hosp Epidemiol 1995; 16:553-5.
[30.] Shefer A, Dales L, Nelson M, Werner B, Baron R, Jackson R. Use and safety of acellular pertussis vaccine among adult hospital staff during an outbreak of pertussis. J Infect Dis 1995;171:1053-6.
[31.] Poland GA. Acellular pertussis vaccines: new vaccines for an old disease. Lancet 1996;347:209-10.
PAUL T. SCOTT, CPT, MC, USA is a third-year resident in the Madigan Army Medical Center Department of Family Practice, Ft. Lewis, Wash. He received his medical degree from the George Washington University School of Medicine and Health Sciences, Washington, D.C.
JEFFREY B. CLARK, LTC, MC, USA is a senior fellow in the faculty development program at Madigan Army Medical Center. He earned his medical degree at East Carolina University, Greenville, N.C., and served a residency in family practice at Silas B. Hays Army Community Hospital, Ft. Ord, Calif.
WILLIAM F. MISER, LTC, MC, USA is director of the faculty development program at Madigan Army Medical Center. He previously served as residency director of the family practice residency program at Tripler Army Medical Center. A graduate of Ohio State University College of Medicine, Columbus, he completed a residency in family practice at Dwight David Eisenhower Army Medical Center, Ft. Gordon, Ga.
Address correspondence to Paul T. Scott, M.D., Department of Family Practice, Madigan Army Medical Center, Ft. Lewis, WA 98431-5000.
COPYRIGHT 1997 American Academy of Family Physicians
COPYRIGHT 2004 Gale Group