Letters from AFI Readers
Send us your letters: A Friend Indeed, Main Floor - 419 Graham Ave., Winnipeg MB R3C 0M3 Or A Friend Indeed, P.O. Box 260, Pembina ND 5827-0260 - Or email us at afi@afriendindeed.ca
Hot flashes and cigarettes DEAR AFI: I am 53 years old and I have been suffering terribly from hot flashes, at least five times a day if not more. My best friend tells me that the reason I'm burning up is the fact that I smoke about a pack a day. Do cigarettes cause hot flashes? - C.M.
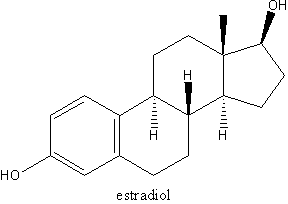
AFI: Smokers do tend to report more hot flashes. Why this happens is not entirely clear. Perhaps it has something to do with the chemicals in cigarettes interfering with estrogen production and action in the body. As well some smokers are very thin and this may also add to their problems with hot flashes. Fat cells produce estrogens and thus women who are thinner often report more hot flashes. You are probably well aware of all the negative effects of smoking cigarettes. As you age, it becomes even more important that you try to kick your cigarette habit. You are at the age where heart disease becomes more of an issue for women, and smoking is certainly a major contributor to that problem. We encourage you to seriously try to quit smoking (or at least cut down), and you will likely find that your hot flashes improve as will many other things. You may have tried to quit in the past; take heart that it often takes many tries to succeed. The Winnipeg Women's Health Clinic has a journal, Catching Our Breath, especially written for women who are trying to reduce or stop smoking (email: afi@afriendindeed.ca). It is designed to help you look at the specific issues that women have with respect to smoking. (Please see AFI, Jan/Feb 2004 Cigarettes: A woman's best friend? for a more extensive discussion of these issues and list of resources.)
The birth control pill at my age?
DEAR AFI: I went without a period for 14 months and then I menstruated again. My doctor was concerned enough to send me to a gynecologist. This new doctor told me that I should take progesterone for about a week. Then I am supposed to go on the birth control pill to regulate my period and to keep the uterine lining from building up, which I was told could cause endometrial cancer. Also, I have had cysts on my ovaries off and on for years and have had fibroids removed from my uterus. I've never taken the birth control pill, and at 49 years of age, I certainly don't want to start now. What else can I do? - J.K.
AFI: Any bleeding after you have not had a period for a year is a matter of concern. In the best case scenario, it could be a sign of too much estrogen in your system. In the worst case, this can be a sign of cancer of the uterus. Often when this happens, a woman undergoes a procedure called an endometrial biopsy to see what is happening with the uterine lining. We assume that you had this done and your doctor felt that all you needed was some progesterone. Taking the progesterone once is usually a good idea as it counteracts the estrogen and will usually take care of the built-up lining due to the excessive estrogen. As to what you need to do in the future, there are several options. The birth control pill is one of these options but by no means the only one. Other options include: 1) To wait and see what happens. If you bleed again, you would need to be investigated with a biopsy. Even if you don't bleed, some doctors would suggest a repeat biopsy in six months just to see how things are in the uterus. 2) Take progesterone for 10 to 12 days a month for the next six months. The theory behind this is that if you had bleeding it means you have enough estrogen in your body, so the birth control pill would not be necessary. The progesterone alone would be sufficient to protect your uterus from the estrogen.
Out of joint
DEAR AFI: In 2003, I had surgery on both of my rotator cuffs, which were damaged because of all the skiing I have done over the years. They were fine until about six months ago when they started getting stiff and hurting again. I have been told that sometimes menopause causes joint pain. Is this true? I sure don't want to have to go through surgery again. - D.J.
AFI: Some women do report joint pains that come around the time of the menopause. How and why this happens is not entirely clear. Usually these symptoms improve as women move past the menopausal transition. This may or may not be contributing to your pain as it sounds like you have other reasons for having sore shoulders.
Bio-identical hormones forever?
DEAR AFI: I was very interested in your feature in the November/December 2004 issue on bio-identical hormones. I have been taking HRT (Estrace and Prometrium) for the last four years. My doctor wants to switch me to a topical estrogen to reduce my chances of heart disease. She says that the oral estrogen can increase my risk of blood clots (which was confirmed in your feature). I went on HRT because I began to suffer from headaches that interfered with work that no remedy could help, but HRT did. I also have osteopenia. I'm afraid of getting off HRT because of the headaches and I worry about my bones. What do you suggest? - M.F.
AFI: It is quite common to be nervous about stopping hormones, particularly if you feel that they have been helpful. However the side effects of hormones are such that it is likely to be useful to see where your body is at without them. You may be surprised how your body has changed over the past four years and how well you can cope without them. If your bones are a concern, there are many other ways to help preserve them. HRT is no longer considered the first or best treatment to reduce your risk of osteoporosis. Exercise, calcium, vitamin D and not smoking are easy and risk-free ways to preserve your bones. There are other non-hormonal medications that can also help with issues related to bones. Headaches, particularly migraines, usually go away after the menopausal transition is complete. There are some additional concerns about a person with headaches being on hormones due to an increased risk of stroke in migraine sufferers. Other measures may also help to reduce the risk of your headaches returning. Exercise, regular hours of sleep, eating frequent small meals and avoiding food triggers such as red wine, chocolate, and old cheese should increase your likelihood of success. Taking a calcium supplement that also includes magnesium may also be helpful as some studies have suggested that magnesium may help prevent migraines. You could likely start to wean yourself gradually off of hormones. This weaning process should take approximately six months or so to complete. An estrogen gel or cream can help in this process as you have more control over the dose of estrogen you are taking and you can more smoothly taper down your hormone dose. Good luck.
Copyright Initiatives for Women's Health, Inc. Mar/Apr 2005
Provided by ProQuest Information and Learning Company. All rights Reserved