Question: Is it safe to take black cohosh, red clover, soy and my ERT, Estrace .5 mg daily?
[ILLUSTRATION OMITTED]
Answer: I'm so glad you wrote in with this question because it is a perfect example of how to combine conventional treatment with natural medicine. This integrative medicine approach that you have come up with on your own is not only safe, but in my opinion, is preferred over increasing your Estrace dose to 1 mg. Guidelines from the North American Menopause Society now currently recommends taking the lowest dose of estrogen possible for the shortest amount of time possible. You are doing that by keeping your estrogen dose low and adding the herbs for additional support to relieve symptoms. Some physicians might raise the question that we do not have any scientific evidence on the combined use of herbs for menopause plus estrogen replacement therapy at the same time. That is true. However, there is no indication from any source that this could pose any problem.
Question: I have very heavy periods and have been treated with a high dose progestin and a dilation and curettage (D and C). There were no fibroids or cancerous cells and no mass. I now have heavy bleeding again and my Dr. believes I have adenomyosis and tells me the only way to verify the diagnosis is to remove the uterus. Can you comment on this?
Answer: It's true that the most definitive way to diagnose adenomyosis is a hysterectomy. Some women have a myomectomy for uterine fibroids and then adenomyosis is also noted on the pathology report for the uterine tissue that is removed. However, an MRI is now able to diagnose adenomyosis much of the time. It may be possible to miss it, but in the hands of an excellent radiologist reading the film, this is your best non-surgical option for diagnosis. As you have experienced, adenomyosis can be difficult to treat so from a surgeon's perspective, the hysterectomy gets you both the treatment and the diagnosis. I have treated several cases over the years now and have been able to successfully manage most but not all cases. The success comes with managing the bleeding better, while not necessarily curing the disease. For a woman in her 40s, if the bleeding comes under better control, then she can usually hold on until she reaches menopause. It may be that a regimen of progesterone, herbs for hemorrhage, vitamin A, bioflavonoids and vitamin C could reduce your bleeding. I would encourage you to look for a licensed naturopathic physician in your area along with an acupuncturist who also uses Chinese Herbs.
Question: I've had recurring bladder infections for 3 years that has been successfully treated in the last year with a topical Premarin cream to the external genital area. I'm concerned about synthetic estrogen and was wondering if there is anything else I could take to prevent those infections.
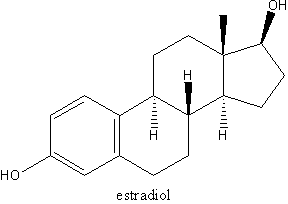
Answer: Topical estrogen to the genital area is a very good use of estrogen for women with atrophic tissue and recurring bladder infections as well as those menopausal women with recurring vaginal infections. I typically use estriol cream or estradiol cream rather than the Premarin cream. Even your conventional doctor is familiar with estradiol cream called Estrace cream. I use compounded estriol cream from a compounding pharmacy. Estradiol and estriol are plant derived and are called natural estrogens because they are biochemically identical to the body's estrogen. Keep in mind though that these are hormones, not herbs. I say this not because I think they are bad, just that I want you to know that. Since you already tried cranberry, I'm not going to recommend that. It might be that with cranberry plus oral lactobacillus acidophilus capsules plus the Estrace cream or Estriol cream 2-3 times per week you may end up being able to reduce your frequency of infections. The proper amount of lactobacillus species in the vagina not only helps to prevent vaginal infections but also bladder infections. It is also important to know that when you use estrogen cream topically without any progesterone, you should not use it more than 2 or 3 times per week. You will want to let your doctor know if you have any bleeding after not having had menses for 6 months. Don't be afraid of topical estrogen. The concerns that you have and have read about hormones essentially do not apply to this very low dose used in the genital area. In addition, very very little of it is absorbed systemically. Vaginal and/or vulvar estrogen treatment for recurring vaginitis, itching or bladder infections due to a lack of estrogen is one of those situations where estrogen creams are a great treatment for women. There is no good herbal substitute. It is safe and very effective. Give your doctor a call and ask for Estrace cream at least then you know you are using a natural hormone versus the Premarin cream.
Question: I have suffered from vaginal yeast infections on and off for a number of years due to a medical misdiagnosis and a long course of antibiotics. I am an unemployed college student; can you tell me an inexpensive solution to my Candida without the radical diet approach so I can banish this beast from my life forever?
Answer: Fortunately, this is probably fairly straightforward. The key is to correct the acid/alkaline balance in your vagina. The vagina's normal pH is acidic. Yeast and bacteria overgrow in an alkaline environment. Therefore, we need to acidify your vagina. The very best treatment I've ever utilized is boric acid suppositories. There is a commercial product available in a capsule in natural foods stores, but you can also make it yourself. For a chronic problem such as yours, you need to do this for at least 2 weeks and up to 4 weeks. Insert one capsule full of boric acid powder into your vagina twice daily. After let's say 4 weeks. Insert one capsule daily only during your menses and only for the next 4 months. This is the best regimen for people who have had chronic recurring yeast vaginitis. Also, there is some evidence that taking 1 cup of acidophilus yogurt or a lactobacillus species (acidophilus and others) capsule daily for several months may also help to repopulate the vagina with the lactobacillus species of bacteria it considers normal and therefore continue to keep it acidic on its own. I don't think you have to do the super strict Candida diet, but I would minimize the white flour, white rice, sugar and alcohol in your diet. These items are essential fuel for Candida. It would be very unusual for the boric acid routine not to work.
As a side note, and for other readers, women with chronic recurring yeast vaginitis also need to be assessed by a practitioner to make sure there is not an underlying immune or endocrine disorder that leads to overgrowth of Candida; examples include diabetes, HIV and hypothyroidism.
Question: Why do vegetables from the nightshade family and citrus cause arthritis to act up? Also, why do acidic foods cause sores in the mouth? I enjoy all of these foods but the side effects are very aggravating.
Answer: Almost any food can aggravate arthritis but the most common foods are wheat, dairy products, beef and the nightshade family (potato, tomato, eggplant, peppers and tobacco). The nightshade foods contain alkaloids called solanine which are thought to inhibit normal collagen repair in the joints or promote inflammatory degeneration of the joint in perhaps one third of people with arthritis. This has yet to be proven but many individuals do find avoiding these foods to be beneficial.
Recurring mouth sores appear to be related to food sensitivities and/or nutrient deficiency. There is considerable evidence that a sensitivity to gluten (a protein found in grains) is the primary cause of recurrent canker sores. Recurring canker sores is a typical manifestation of individuals with celiac disease, a condition with diarrhea and malabsorption due to a sensitivity to gluten. Although you notice a flare-up with the citrus, and this may genuinely be due to an allergy/sensitivity to citrus, it may be that the tissue is already compromised perhaps due to a gluten sensitivity, and then the citrus just puts you over the edge. If you have digestive symptoms, I would check into testing for gluten sensitivity.
Question: I recently began taking birth control pills and read that there is some evidence that St John's wort can interfere with its efficacy. Are there any other common herbs that you know of that cause drug interactions?
Answer: There have been a couple of case reports and now two studies published in the scientific literature that have suggested that the St. John's wort reduced the efficacy of the birth control pill. (reference: Hall S, et al. The interaction between St. Johns wort and an oral contraceptive. Clin Pharmacol Ther 2003;74:525-535) (Pfrunder A, et al. Interaction of St. John's wort with low dose oral contraceptive therapy: A randomized controlled trial. Br J Clin Pharmacol 2003;56:683-690) Both the plant and the medication are metabolized through the same enzyme system in the liver so it is theoretically possible. Regarding other plants that may reduce the efficacy of birth control pills, this is an area where we in fact know very little. There are people who suggest that chaste tree berry may interfere, due to the fact the chaste tree promotes ovulation and oral contraceptives inhibit ovulation. However, I do not agree with this because I believe that chaste tree is much weaker than the birth control pill. Also, there is no evidence that dong quai, wild yam or black cohosh could interfere with oral contraceptives.
Question: I had a hysterectomy in 1981 and am still taking .625 estrogen. My Dr. tells me that I need to go off of it because of the risk of breast cancer. I've been taking it for 20 years. When I reduce to .375, I have many symptoms. I tried black cohosh, red clover, vitamin E and other products, and that doesn't seem to work either. I still have hot flashes at night.
Answer: Your physician is basing his recommendations on the results of the Women's Health Initiative (WHI) which shows that women who take estrogen and progestin for 4 or more years, have an increased risk of breast cancer. There are other studies that show similar findings. However, the results of the WHI for women who had a hysterectomy and are only taking the one medicine, estrogen, showed no increased risk of breast cancer. Other previously published research has also shown that the risk of breast cancer with estrogen only, is much lower than the risk of breast cancer with estrogen and progestin. It is important to remember that the risk of breast cancer for either regimen, is still very low. The risk of breast cancer associated with either family history, obesity, or more than one drink of alcohol per day are each higher than the risk associated with hormones. You have to weigh quality of life issues and how you want to feel day to day versus these risks. Nonetheless, here are some other ideas:
* Check your dose of black cohosh and duration of use. Try 40 mg of standardized extract twice daily and give it 4 weeks before you decide if it is working or not.
* Since you've had problems specifically with nightsweats, take red clover extract 40 mg twice per day along with the above dose of the black cohosh.
* Another option would be to take the .375 dose of estrogen along with black cohosh and/or red clover.
* If none of these work, then try .625 one day and .375 the next day and continue on this alternating regimen. That would at least be lower than the .625 mg every day. You could also request a prescription of bio-identical estrogen. This may have some as yet not well understood advantages over the Premarin.
We could all use some reminder about known methods of reducing our risk of breast cancer: Maintain ideal body weight, drink less than 1 drink of alcohol per day, low fat diet, good fat diet (olive oil, fish, nuts, seeds; avoid partially hydrogenated oils), lots of fruits and vegetables, soy foods, high fiber diet, regular exercise at least 4 times weekly, and try to eliminate pesticides and chemicals in our daily life.
Question: I am 34 years old and I have acne on my chin. I don't have any other signs of a hormonal problem with no facial hairs or anything like that. I tried taking progesterone cream but that did not help. What are your recommendations for my acne problems?
Answer: Although often a simple problem, acne can be difficult to treat. Theories about dietary influences on acne are controversial and contradictory. Chocolate, high fat diets, transfatty acids, sugar and simple carbohydrates have all been implicated. There have been some effects with vitamin A, vitamin E 400 i.u., selenium 200 mcg, zinc 45 mg, and pantothenic acid 2.5 gm four times per day up to two weeks. You have to be careful about the dosage of vitamin A in particular. The dosages that have been shown to be the most effective are high and potentially toxic. A dosage of 10,000-25,000 I.U. per day for 3-6 months should have no negative effects. I have had very good luck with adding some topical treatments such as a topical niacinamide spray, topical Tee tree oil, or treatments with a Dr. Haushka, aesthetician.
I don't know how long you tried the natural progesterone cream, but try it for at least 3 months. Natural progesterone can help many women with acne. It is still possible that there are some hormonal aspects to your acne.
Previously published in Let's Live March 2003
by Tori Hudson, ND
Professor, National College of Naturopathic Medicine and Bastyr University
Medical Director, A Woman's Time
Author, Women's Encyclopedia of Natural Medicine
2067 N.W. Lovejoy * Portland, Oregon 97209 USA
503-222-2322 * womanstime@aol.com
COPYRIGHT 2005 The Townsend Letter Group
COPYRIGHT 2005 Gale Group