Shortly after the combined therapy arm of the Women's Health Initiative (WHI) Study (which concluded that Prempro (1) increases a woman's risk of breast cancer, stroke, and cardiovascular disease) was halted, a group of women's health experts were interviewed on Seattle's public radio station. The experts were unanimous: "estrogens cause cancer, and women shouldn't take them." If only it was that simple! Since then, new research has appeared that calls many of our initial impressions from the WHI trial into question. Some of these questions are:
1. How much of an increase in adverse outcomes was associated with Prempro use? The base rates of breast cancer, stroke and myocardial infarction were low in the WHI Trial. Thus the relatively large percentage increases in these outcomes implies only a small number of additional cases. As one reporter put it, "Last year, 6 million post-menopausal American women woke up to the front-page news that their hormone replacement treatment was increasing their chances of getting breast cancer by 26%, stroke by 41% and heart attacks by 29%. What the percentage changes actually represented, though, was a change in a rate--an additional seven to eight women per 10,000 were diagnosed with these disorders.... Death rates were not increased at all." (2)
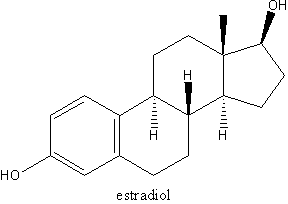
2. Which component of Prempro caused the adverse outcomes? Or was it the combination? Some of the larger post-WHI studies are summarized in Table 1. Although some of the trials suffer methodologically because they were not placebo controlled, they have the strength of large numbers. A study of 3663 women from Sweden found a large percentage increase in breast cancer cases in women who took estrogen + progestin continuously (as the women in the WHI Trial did). Women who took estrogen + progestin sequentially (to mimic the natural menstrual cycle) had a smaller increase in breast cancers, which did not reach statistical significance. Women who took estradiol alone had no increase in breast cancer risk. (3)
A study of 1739 women from France concluded: "[t]he results of the present study, in long-term users of a combination of transdermal estradiol and a progestin closer to progesterone than MPA [medroxyprogesterone acetate, used in the WHI], do not show any increase in breast cancer risk." (4)
A study from the Fred Hutchinson Cancer Research Center in Seattle found increased risk of breast cancer for women taking estrogen + progestin, but no increased risk for women taking estrogen alone. (5)
The largest study to date, the aptly named Million Women Study from Britain, (6) described a gradient of breast cancer risk, with estrogen + progestin associated with the greatest increase in breast cancer risk, and estrogen alone associated with a smaller, but statistically significant, increase in breast cancer risk.
Finally, the estrogen-only arm of the WHI trial was halted in early March 2004. (7) The study concluded that, "with an average of nearly 7 years follow-up completed, estrogen alone does not appear to affect ... heart disease.... At the same time, estrogen alone appears to increase the risk of stroke and decrease the risk of hip fracture. It has not increased the risk of breast cancer...." (Emphasis added).
One of the confounding factors in the studies cited is that the women who received only estrogen had in almost all cases had their uterus removed, and were thus sampled from a different population than women receiving combined HRT. It is possible that there is a difference between women with intact uteruses and women without them that confers additional breast cancer risk. Nevertheless, at present the evidence strongly suggests that combined HRT with a synthetic progestin increases breast cancer risk much more than estrogen-only HRT. Evidence regarding estrogen-only HRT is mixed: some studies show no increased breast cancer risk, but the largest, most statistically powerful study finds a small but significant increase in risk with estrogen alone.
3. This leads us to the next important question: Are bioidentical estrogens safer than synthetic or equine estrogens? One of the tragedies of the WHI trial is that the only active treatments offered were Prempro and Premarin. Without head-to-head comparisons of bioidentical HRT formulations and Prempro/Premarin, it is not possible to state definitively that bioidentical HRT is safer. There is ample evidence that estrogens, at least under certain conditions, are capable of inducing mutagenic and genotoxic changes. (8) Critical factors include the estrogen dose, the patient's individual metabolic profile, and the relative amounts of various estrogens present. But the magnitude of estrogen-related carcinogenesis is relatively small: up to a 29% increase in breast cancer risk with estrogens alone compared to roughly a 1000% increase in lung cancer risk for smokers compared to non-smokers.
In order to reconcile and unify the clinical studies that have appeared to date, we need to add one more piece to the puzzle: the effect of estrogen dose. It is widely assumed that adverse effects of estrogens are dose-related. The original recommended dose of Premarin (the conjugated equine estrogen component of Prempro) was 1.25 mg. Subsequently; it was lowered to 0.625 mg (the dose used in the WHI trial). Recently, a 0.3 mg formulation was approved (although enlightened practitioners experimented with these lower doses as far back as the 1980s9). The same pattern is evident for estradiol. Early formulations contained 2 mg, which was subsequently lowered to 1 mg. Dr. Jay S. Cohen recommended 0.5 mg in 2001. 10 Last year, a study was published in JAMA demonstrating beneficial effects on bone health with an estradiol dose of 0.25 mg. (11)
What dose of estradiol replaces estrogens at normal premenopausal ranges? The answer to this question is complicated by the fact that the interconversion between estradiol and estrone is shifted toward estrone after menopause. And elevated estrone concentrations are associated with an increased risk of breast cancer. (12) In Figure 1, I have plotted the urinary estrone output for 22 post-menopausal women whose hormones were tested at Meridian Valley Laboratory, 19 of whom were receiving estradiol orally in various doses. Note that at estradiol doses above 0.25 mg, urinary estrone output is uniformly above normal premenopausal levels. At estradiol doses of 1 mg, urinary estrone output is roughly four times higher than the upper limit for normal pre-menopausal women.
[GRAPHIC OMITTED]
[GRAPHIC OMITTED]
[GRAPHIC OMITTED]
Figure 1 only shows evidence for excessive estrone in urine. What do blood tests tell us? In many cases, only serum estradiol is measured, so the rate of conversion to estrone is unknown. But where this information is available, it indicates elevated serum estrone in post-menopausal women receiving high-dose estrogen replacement therapy. The package insert for one product (13) that provides 1 mg of estradiol indicates that the mean peak serum estradiol level is around 100 pg/ml, while the mean peak estrone level is around 500 pg/ml. For comparison, the median estrone levels in premenopausal women measured by one popular radioimmunoassay are: follicular phase 62 pg/ml, luteal phase 65 pg/ml, and peri-ovulatory 123 pg/ml. The package insert for this methodology gives expected estrone values in post-menopausal women receiving estrogen replacement therapy (probably conjugated equine estrogens 0.625 mg) of up to 346 pg/ml, (14) much higher than the normal premenopausal levels.
[GRAPHIC OMITTED]
[GRAPHIC OMITTED]
This may help us understand some of the differences in Table 1. The French study that found no increase in breast cancer risk with estradiol, dealt with women receiving low-dose transdermal estradiol. Clearly, we can expect the best results when estradiol is given at lower doses that result in more physiological estrone serum and urine concentrations. It seems that those who set the original recommended doses at supra-physiological levels may have done a great disservice to post-menopausal women.
In summary, the factors known to be associated with the most adverse outcomes in estrogen replacement therapy are: (1) use of synthetic progestins in combinations with estrogens, (2) use of continuous rather than sequential estrogen administration, and (3) excessive estrogen dose. The main arm of the WHI trial managed to combine all three in a worst-case scenario that, not surprisingly, gave negative results.
More research on bioidentical hormone replacement is urgently needed. There is compelling laboratory evidence that natural progesterone is safer than synthetic progestins. (15, 16) Clinical trials are needed to confirm this. Also high on the research agenda are oral and transdermal low-dose estradiol, as well as estriol alone and in combination with estradiol. Finally, we must develop a better understanding of laboratory monitoring of HRT--what to measure, in which body fluids, and when to measure it.
References
1. Conjugated equine estrogens plus the synthetic progestin medroxyprogesterone
2. Eisenstadter I. Countdown to ignorance. Barron's December 1, 2003, p. 35.
3. Olsson HL, Ingvar C, Bladstrom A. Hormone replacement therapy containing progestins and given continuously increases breast carcinoma risk in Sweden. Cancer. 2003 Mar 15;97(6): 1387-92.
4. de Lignieres B, de Vathaire F, Fournier S, Urbinelli R, Allaert F, Le MG, Kuttenn F. Related Articles, Links Abstract Combined hormone replacement therapy and risk of breast cancer in a French cohort study of 3175 women. Climacteric. 2002 Dec;5(4):332-40.
5. Li CI, Malone KE, Porter PL, Weiss NS, Tang MT, Cushing-Haugen KL, Daling JR. Related Articles, Links Abstract Relationship between long durations and different regimens of hormone therapy and risk of breast cancer. JAMA. 2003 Jun 25;289(24):3254-63.
6. Beral V; Million Women Study Collaborators. Related Articles, Breast cancer and hormone-replacement therapy in the Million Women Study. Lancet. 2003 Aug 9;362(9382):419-27.
7. http://www.nlm.nih.gov/databases/alerts/estrogen_alone.html
8. Friel PN. Laboratory Evaluation of Estrogen Metabolism. TLIDP 245:62-66; December 2003.
9. Wright JV, personal communication.
10. Cohen JS. Over Dose: The Case Against the Drug Companies. New York: Penguin Putnam (2001).
11. Prestwood KM, Kenny AM, Kleppinger A, Kulldorff M, Related Articles, Links Abstract Ultralow-dose micronized 17beta-estradiol and bone density and bone metabolism in older women: a randomized controlled trial. JAMA. 2003 Aug 27;290(8):1042-8.
12. Friel PN, ibid.
13. Activella, Physicians Desk Reference 2002.
14. Estrone RIA, DSL-8700, Diagnostic Systems Laboratories, Inc. 1999.
15. Wright JV, Morgenthaler J. Natural Hormone Replacement for Women Over 45. Smart Publications (1997).
16. Thomas T, Rhodin J, Clark L, Garces A. Progestins initiate adverse events of menopausal estrogen therapy. Climacteric. 2003 Dec;6(4):293-301.
by Patrick Friel, BS
Correspondence:
Patrick Friel
801 SW 16th Street, Suite 126
Renton, Washington 98055 USA
425-271-8689
COPYRIGHT 2005 The Townsend Letter Group
COPYRIGHT 2005 Gale Group