It seems that bio-identical hormones are all the rage these days. But what exactly are they? How are they made? And, are they safe?
In my years of treating and doing research with women and teaching doctors, I have been keenly interested in finding what is healthy for women concerning their ovaries and reproduction. For example, I predicted the recent negative results of the Women's Health Initiative trial of estrogen and progestin more than 10 years ago. Although some of us will need treatment after menopause, the blanket prescription of bio-identical hormones to all menopausal women is no wiser than past widespread use of Premarin and Provera.
What are bio-identical hormones?
Bio-identical hormones are the same as, or identical to, hormones made by our bodies. We used to use the term "natural" to describe these hormones, but natural seems to encompass many things. One could say that the estrogens in pregnant mare's urine (brand name: Premarin) are natural - but only for horses. Bioidentical hormones are only available by prescription. This is true even if they are "compounded" or made into a medical form by a local pharmacist.
How are bio-identical hormones made?
That varies depending on the hormone. I know most about progesterone so I'll use that as an example. Progesterone is made from a vegetable base. However, bio-identical progesterone was not a medicine humans could take until about a decade ago when we learned to mix it with peanut oil in very small bits, a process known as micronization. Oral micronized progesterone (brand name: Prometrium) can be absorbed through the stomach lining and continue to be an active hormone. Progesterone is also used as a compounded or manufactured cream but we don't yet know the effective doses.
Although most of us refer to bioidentical hormones in relation to menopause treatment, there are other hormones that are bio-identical, such as calcitonin (brand name Miacalcin, made from salmon) and human insulin, created genetically using bacteria. In other words, bio-identical hormones have been with us for years.
What are the differences between bio-identical hormones and synthetic ones?
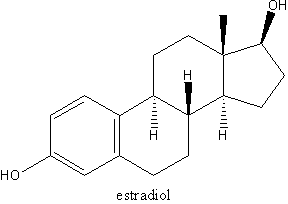
Bio-identical hormones are identical to hormones our bodies make. They talk to cells through specific receptors that are made for them. For example, bio-identical estradiol (a type of estrogen) in patch form, gel or cream (brand names: Estragel, Estradot, Tri-Est, Bi-Est) acts just like the estradiol our ovaries secrete into the bloodstream. However, bioidentical estradiol in pill form (brand names: Estrace, Tri-Est, Bi-Est) has the negative effect of increasing blood clots because it is not natural for estrogen to enter the bloodstream through the stomach. Pill estrogen, even if it is bio-identical, goes from the stomach to the liver and stimulates it to make clotting factors.
Are bio-identical hormones a major medical advance?
The answer is both yes and no. For example, some of the created hormones like medroxyprogesterone (brand name: Provera, and generic ones) are very close to bio-identical progesterone. Other progestins, like those in birth control pills, more closely resemble testosterone.
Oral micronized progesterone has two beneficial effects that medroxyprogesterone doesn't: It helps promote sleep, and is positive for blood vessels. Some early evidence suggests that medroxyprogesterone may make blood vessels cramp up, decreasing blood flow, which can contribute to heart disease. Our preliminary work shows that micronized progesterone makes blood vessels relax so that blood flow improves. However, oral micronized progesterone costs almost three times as much as medroxyprogesterone. For progesterone, the question often boils down to whether a woman is having trouble with sleep. Oral micronized progesterone increases deep sleep by about 15 percent, whereas medroxyprogesterone doesn't. Therefore if you are tossing and turning at night, the higher cost may be worth it.
Have bio-identical hormones been studied as much as synthetic hormones?
In general, the answer is no. However, for many bio-identical hormones, key studies have been done. Most effects of hormones are specific to that kind of hormone. For example, we can expect bio-identical estradiol in topical form to have similar effects on breast cancer risk as Premarin, and bio-identical oral estradiol to have similar effects on stroke as shown by Premarin in the Women's Health Initiative hormone trials. However, many studies are still needed. In the case of progesterone, we know that medroxyprogesterone is effective in treating night sweats. However, we don't yet know whether oral micronized progesterone is as effective as medroxyprogesterone.
For that reason, my colleagues and I are now doing a three-month randomized trial of oral micronized progesterone compared with placebo for menopausal women with moderate to severe night sweats. We have enrolled 51 women and are going to recruit a total of 125. In addition, we are testing for possible effects of progesterone on blood pressure, waist circumference, fasting cholesterol and blood sugar levels as well as on the relaxation of blood vessels. (For more information about this study, log on to the Centre for Menstrual Cycle and Ovulation Research web site: www.cemcor.ubc.ca). We won't know the results for another couple of years.
Who might consider bio-identical hormones?
Bio-identical hormones have some advantages over synthetic hormones, but they are still hormones and shouldn't be used unless needed. Menopause is a normal part of every woman's life cycle. In my best judgment - and my recommendations arise from research, studying the literature as well as my clinical practice - I believe that women who experience early menopause (i.e. before age 40) need to take bio-identical estrogen and progesterone in doses similar to the second half of the menstrual cycle (see Early Menopause on the CeMCOR website) and to continue until reaching age 51. Estrogen first, then progesterone should be tapered and stopped (see "Stopping Estrogen Therapy" on the CeMCOR site).
I also suggest that women who have osteoporosis plus night sweats use estrogen and progesterone for five years and then stop the estrogen. Progesterone builds new bone and could be continued with another bone-loss preventing therapy if needed.
Finally, menopausal women who have been unsuccessful with non-hormonal measures for sleep-disturbing night sweats may consider either medroxyprogesterone or oral micronized progesterone therapy. This can be safely continued, tapering each year until they have stopped (see "Progesterone therapy for Menopausal Women" on the CeMCOR website).
For women with vaginal dryness that is not responsive to non-hormonal gels and lubricants, I prescribe vaginal bio-identical estriol cream (it is only available compounded) in a dose of 0.5 mg once a week.
What is the future for bio-identical hormones?
Women's intense interest in taking bio-identical hormones means that the old synthetic therapies will decrease. Gradually, studies will be performed with the bio-identical hormones in doses that are acceptable and effective.
Menopausal women with surgical menopause (uterus and ovaries removed) who have loving partners yet virtually no sexual response may consider very low doses of bio-identical testosterone as a compounded cream once a week. The ovaries of other menopausal women continue to make enough testosterone - therapy is too risky.
By Dr. Jerilynn C. Prior
Jerilynn Prior is a physician, researcher and specialist in hormones and glands, and professor of medicine and endocrinology at the University of British Columbia in Vancouver. If you wish to view the study references, email her at emcor@interchange.ubc.ca with "Bio-Identical References" in the topic or subject line. Log on to her web site at www.cemcor.ubc.ca for more information.
Copyright Initiatives for Women's Health, Inc. Nov/Dec 2004
Provided by ProQuest Information and Learning Company. All rights Reserved