Abstract
BACKGROUND: There is a lack of consensus about the safety of estrogen replacement therapy, especially with regard to its impact on a woman's risk for breast cancer. Elevated urinary or serum estrone and estradiol concentrations in postmenopausal women are associated with a moderately elevated risk of breast cancer. METHODS: Twenty-four-hour urinary steroid hormone profiles, including the measurement of estrone, estradiol, and estriol, were conducted for 35 postmenopausal women receiving oral estradiol at doses from 0.025-2.0 mg/day. RESULTS: Urinary excretion of estradiol exceeded premenopausal reference range values in women taking estradiol at doses greater than 0.5 mg/day. Urinary estrone excretion exceeded premenopausal reference range values in women taking estradiol doses of 0.25 mg/day or higher. Literature data indicate serum estrone concentrations also markedly exceed premenopausal reference ranges when estradiol is administered orally at a dose of 1 mg/day. CONCLUSIONS: The previously recommended oral dose of estradiol (1-2 mg/day) results in urinary excretion of estrone at values 5-10 times the upper limit of the reference range for premenopausal women. Retrospective studies associating oral estradiol with increased risk of breast cancer may reflect overdose conditions. Based on current knowledge, a prudent dose ceiling for oral estradiol replacement therapy of 0.25 mg/day is proposed.
(Altern Med Rev 2005;10(1):36-41)
Introduction
"The dose makes the poison."--Paracelsus (1493-1541)
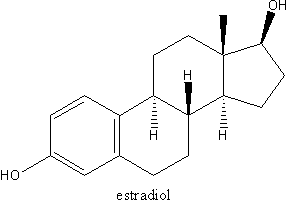
Under laboratory conditions, estrogens are capable of both initiating and promoting malignancies. (1) A number of human breast cancer risk factors, such as early age at menarche and late age at menopause, reflect lifetime estrogen exposure. (2) Furthermore, epidemiological studies of estrogen concentrations in serum and urine demonstrate postmenopausal women with higher estrogen concentrations--especially in the case of estrone--are at elevated risk for developing breast cancer, compared to postmenopausal women with lower estrogen concentrations. (23) There is considerable evidence estrogens act as promoters of human breast cancer, although the evidence that estrogens act as breast cancer initiators is weaker. (4,5) Thus, while it seems reasonable to conclude estrogen replacement therapy for women during menopause results in an increase in breast cancer risk, the results of many retrospective and prospective studies of hormone replacement therapy (HRT) are inconsistent.
The Women's Health Initiative study found conjugated equine estrogens taken continuously at a dose of 0.625 mg/day, in combination with the synthetic progestin medroxyprogesterone, are associated with a modest but statistically significant increase in breast cancer risk. (6) But a study of the same conjugated equine estrogen regimen taken without a synthetic progestin, in women who had hysterectomies, found no increase in breast cancer risk.(7) However, the United Kingdom's "Million Women Study" of HRT found an elevated risk of breast cancer, even in women taking estrogens only (conjugated equine estrogens or estradiol orally), although the increase was not as great as for women taking estrogens combined with synthetic progestins. (8)
Studies of HRT in women with a history of breast cancer have also yielded conflicting results. A retrospective U.S. study found women with a history of breast cancer who received HRT (79% estrogen-only), had a 66-percent reduction in breast cancer mortality, compared to women with a history of breast cancer not receiving HRT. (9) A retrospective Australian study reached similar conclusions. (10) Two recent prospective studies of HRT in women with prior breast cancer found a large increase in breast cancer recurrence with HRT in one, but no increase in the other. (11) It is important to understand the reasons for such divergent results.
In the course of conducting comprehensive, 24-hour urinary steroid hormone profiles on hundreds of women receiving various formulations of HRT, the authors have recognized that women taking what were considered, until recently, standard HRT doses consistently excreted quantities of estrogens greatly in excess of those seen in healthy, non-pregnant, premenopausal women. This report presents data for women taking oral estradiol. The results suggest the dose of estrogen used may be an important determinant of adverse effects, including estrogen-related cancers.
Subjects
The data reported here were collected from the results of 24-hour urinary steroid hormone profiles conducted for clinical purposes on 35 women taking oral estradiol. Women submitted, along with urine specimens, a questionnaire on the use of hormones, other medications, and menopausal symptoms. The questionnaires were used as part of the laboratory quality assurance program, for review of test results, and for consultations with the physicians who ordered the tests. The women in this study represent 35 consecutive patients taking oral estradiol, with or without estriol, who submitted a questionnaire, and who took their prescribed estradiol dose on the day of collection. Data were collected over approximately one year.
The median age of the sample was 54 years (span 43-80). Fifteen women had hysterectomies. Twenty-seven women took progesterone (24 orally and three transdermally). In each case, estradiol doses were stable for one month or longer. The median estradiol dose was 0.5 mg/day (span 0.025-2.0 mg/ day). Twenty-one women took estriol in addition to estradiol.
Materials and Methods
Steroid analysis was performed using standard methods. Steroids were isolated from urine by solid phase extraction (C18 columns, United Chemical Technologies; Bristol, PA), eluted with methanol, and the methanolic extract was evaporated to dryness. The residue was reconstituted in acetate buffer, hydrolyzed overnight with sulfatase/beta-glucuronidase, and extracted with ethyl acetate after internal standard addition. The ethyl acetate extract was evaporated to dryness, and the methyloxime/trimethylsilyl (MOX/ TMS) derivatives of the steroids were prepared. The final derivatized extracts were dissolved in hexane, washed with de-ionized water, and an aliquot of the hexane phase was injected into the gas-chromatographmass spectrometer (GC-MS).
The GC-MS system included an Agilent 6890 GC with a 7683 Autosampler, an Agilent 5973N MSD, and an Enhanced MSD Chemstation data system. A 30 m x 0.25 mm ID, 0.25 micron film thickness dimethylpolysiloxane column was used, with helium (1.9 mL/min) as the carrier gas. Analytes were separated during a 32-minute temperature program, and the estrogens were identified and quantified using selected ion monitoring. with three ions for each analyte. Calibration was performed with derivatized standards prepared from pure analytical reference materials (Steraloids: Newport, R.I.). The laboratory's reference ranges for urinary estrogen excretion are presented in Table 1. (12)
Results
Urinary concentrations of estradiol and estrone were related to estradiol dose in a linear fashion. Linear regression of urinary estradiol concentration as a function of estradiol dose resulted in a coefficient of determination of [r.sup.2] = 0.917 (p<0.001). Linear regression of urinary estrone concentration as a function of estradiol dose resulted in a coefficient of determination of [r.sup.2] = 0.870 (p<0.001).
Urinary estradiol excretion as a function of estradiol dose is presented in Figure 1. The fraction of the estradiol dose excreted unchanged in the urine was 10 [+ or -] 4 percent (mean [+ or -] SD). At estradiol doses up to 0.5 mg/ day, urinary estradiol excretion values were within the reference range for non-pregnant, premenopausal women.
Urinary estrone concentrations as a function of estradiol dose are shown in Figure 2. The fraction of the estradiol dose excreted as estrone was 30 [+ or -] 9 percent (mean [+ or -] SD). In this case, doses of 0.25 mg/day or higher were associated with estrone excretion rates that exceed reference range values for non-pregnant, premenopausal women. In the 14 women who took estradiol without estriol, estriol excretion amounted to 6 [+ or -] 4 percent (mean [+ or -] SD) of the estradiol dose.
Discussion
This study demonstrates that, in the urine matrix, what were until recently standard doses of estradiol (1-2 mg/24 hr) result in excessive excretion of estradiol and especially estrone. The question of whether standard estrogen replacement doses represent replacement or overdose has been raised previously. In 1994, Tepper et al reported that 57 percent of women treated with 2 mg estradiol demonstrated serum estradiol concentrations in excess of those expected in premenopausal women; (13) serum estrone concentrations were not reported. It is well established that the interconversion between estradiol and estrone strongly favors estrone after menopause, raising the possibility that even if estradiol concentrations are within premenopausal limits, estrone concentrations may exceed them. (14)
If low endogenous estrogen production of the postmenopausal study subjects is ignored, the mean urinary recovery of estradiol (as estradiol, estrone, and estriol) was 46 percent of the oral dose. The remainder of the dose should be accounted for by other urinary estrogen metabolites not measured, and estrogen excretion in the feces, which can account for 10-25 percent of the body load. (15, 16) Diet has a significant influence on estrogen metabolism, with vegetarians exhibiting lower endogenous estrogen plasma concentrations and higher fecal excretion. (16) Smoking also alters the metabolism of estrogens. (17) Unfortunately, data were not available regarding the smoking or diet status of the women in this study.
Epidemiological studies demonstrate that serum and urine estradiol and estrone concentrations are positively associated with breast cancer risk in postmenopausal women. (2, 3) In women receiving conjugated equine estrogens, serum estrone concentration is positively associated with increased mammographic density, a strong risk factor for the development of breast cancer. (18) A recently published study of a large European cohort found postmenopausal women in the highest quartile for urinary estrone had 2.5 times the risk of developing breast cancer compared to women in the lowest quartile; women in the highest quartile for urinary estradiol had 1.7 times the risk of developing breast cancer compared to the lowest quartile. (2) Since urinary estrone values for postmenopausal women receiving daily doses of 1-2 mg estradiol greatly exceeded those routinely seen even in premenopausal women, there is reason for concern that these levels may raise breast cancer risk.
The question can be asked whether urinary estrogen data adequately reflect serum estrogen concentrations. A recent study of estradiol replacement therapy in normal women and those with renal failure included the measurement of serum estrone concentrations. (19) In Table 2, results for the healthy control subjects from that study are compared with estrone concentrations for pre- and postmenopausal women, measured by a widely used radioimmunoassay. (20) In agreement with the urinary data presented here, serum estrone concentrations in postmenopausal women taking 1.0 mg/day estradiol exceed premenopausal reference values by approximately a factor of four.
It is of considerable interest that the recommended dose of estradiol has been decreasing steadily. In 2001, Cohen suggested 0.5 mg was an adequate dose for many postmenopausal women, rather than the normally recommended dose of 1-2 mg/day. (21) In 2003, Prestwood et al demonstrated beneficial effects on bone density at a daily oral estradiol dose of 0.25 mg. (22) In 2004, an ultra-low dose transdermal estradiol formulation delivering 14 mcg/day, and demonstrating favorable impact on bone density, was introduced. (23) A similar pattern is evident in the recommended dose of conjugated equine estrogens. Initial recommended doses were 1.25 mg/day. (21) Subsequently, the recommended dose was lowered to 0.625 mg/day, and recently the U.S. Food and Drug Administration approved a 0.3-mg formulation. (21)
Estradiol replacement therapy at oral doses of 1-2 mg/day results in serum and urine estrone concentrations resembling those seen in pregnancy. However, there is an important difference between the estrogens present with estradiol replacement and those during pregnancy--estriol concentrations are much higher during pregnancy than during estradiol replacement. (24) Experimental and epidemiological studies suggest a high concentration of estriol may be necessary to modulate the impact of the high concentrations of estradiol and estrone seen in pregnancy. (24, 25)
Estrogen dose is only one important variable in determining the risk-benefit profile for hormone replacement therapy. By far, the strongest association between estrogen replacement therapy and breast cancer occurs when it is co-administered with the synthetic progestin medroxyprogesterone. (26, 27) The added risk of breast cancer when estrogens can be taken without a synthetic progestin is much less in some studies, and non-existent in others. We propose one important reason for the current uncertainty about the safety of estrogen-only replacement therapy is that estrogen doses have varied from study to study, and the preferred doses have been decreasing over time. Long-term retrospective studies, such as the Million Women Study, may be biased against estrogen replacement, because many patients received estrogen dosages that, in hindsight, were clearly excessive. Based on the data presented here, an oral estradiol dose of 0.25 mg/day or less should result in serum and urinary estrone concentrations within or slightly above the premenopausal reference range. This seems to be a prudent dose ceiling given our present level of knowledge.
Acknowledgement
We are grateful for the dedication and expertise of Michael Allender, who was responsible for sample preparation throughout the study.
References
(1.) Mitrunen K, Hirvonen A. Molecular epidemiology of sporadic breast cancer. The role of polymorphic genes involved in oestrogen biosynthesis and metabolism. Mutat Res 2003;544:9-41.
(2.) Key T, Appleby P, Barnes I, et al. Endogenous sex hormones and breast cancer in postmenopausal women: reanalysis of nine prospective studies. J Natl Cancer Inst 2002;94:606-616.
(3.) Onland-Moret NC, Kaaks R, van Noord PA, et al. Urinary endogenous sex hormone levels and the risk of postmenopausal breast cancer. Br J Cancer 2003;88:1394-1399.
(4.) Wiseman RA. Breast cancer: critical data analysis concludes that estrogens are not the cause, however lifestyle changes can alter risk rapidly. J Clin Epidemiol 2004;57:766-772.
(5.) Wren BG. Do female sex hormones initiate breast cancer? A review of the evidence. Climacteric 2004;7:120-128.
(6.) Rossouw JE, Anderson GL, Prentice RL, et al. Risks and benefits of estrogen plus progestin in healthy postmenopausal women: principal results from the Women's Health Initiative randomized controlled trial. JAMA 2002;288:321-333.
(7.) Anderson GL, Limacher M, Assaf AR, et al. Effects of conjugated equine estrogen in postmenopausal women with hysterectomy: the Women's Health Initiative randomized controlled trial. JAMA 2004;291:1701-1712.
(8.) Beral V; Million Women Study Collaborators. Breast cancer and hormone-replacement therapy in the Million Women Study. Lancet 2003;362:419-427.
(9.) O'Meara ES, Rossing MA, Daling JR, et al. Hormone replacement therapy after a diagnosis of breast cancer in relation to recurrence and mortality. J Natl Cancer Inst 2001;93:754-762.
(10.) Durna EM, Wren BG, Heller GZ, et al. Hormone replacement therapy after a diagnosis of breast cancer: cancer recurrence and mortality. Med J Aust 2002;177:347-351.
(11.) HABITS Steering and Data Monitoring Committees. HABITS (hormonal replacement therapy after breast cancer--is it safe?): a randomized comparison trial stopped. Obstet Gynecol Surv 2004;59:442-443.
(12.) Burtis CA. Tietz Textbook of Clinical Chemistry. 3rd ed. Philadelphia, PA: W.B. Saunders Company; 1999.
(13.) Tepper R, Goldberger S, Cohen I, et al. Estrogen replacement in postmenopausal women: are we currently overdosing our patients? Gynecol Obstet Invest 1994;38:113-116.
(14.) Coelingh Bennink HJ. Are all estrogens the same? Maturitas 2004;47:269-275.
(15.) Alvarez-Vasquez RB, Axelrod D, Frenkel K, et al. Influence of postmenopausal hormone replacement therapy on an estrogen metabolite biomarker of risk for breast cancer. Horm Metab Res 2003;35:358-361.
(16.) Adlercreutz H, Gorbach SL, Goldin BR, et al. Estrogen metabolism and excretion in Oriental and Caucasian women. J Natl Cancer Inst 1994;86:1076-1082.
(17.) Mueck AO, Seeger H. Smoking, estradiol metabolism and hormone replacement therapy. Arzneimittelforschung 2003;53:1-11.
(18.) Ursin G, Palla SL, Reboussin BA, et al. Post-treatment change in serum estrone predicts mammographic percent density changes in women who received combination estrogen and progestin in the Postmenopausal Estrogen/ Progestin Interventions (PEPI) Trial. J Clin Oncol 2004;22:2842-2848.
(19.) Stehman-Breen C, Anderson G, Gibson D, et al. Pharmacokinetics of oral micronized beta-estradiol in postmenopausal women receiving maintenance hemodialysis. Kidney Int 2003;64:290-294.
(20.) Estrone RIA Package Insert, DSL-8700, Diagnostic Systems Laboratories, Inc. 1999.
(21.) Cohen JS. Over Dose: The Case Against the Drug Companies. New York, NY: Penguin Putnam; 2001.
(22.) Prestwood KM, Kenny AM, Kleppinger A, Kulldorff M. Ultralow-dose micronized 17beta-estradiol and bone density and bone metabolism in older women: a randomized controlled trial. JAMA 2003;290:1042-1048.
(23.) Ettinger B, Ensrud KE, Wallace R, et al. Effects of ultralow-dose transdermal estradiol on bone mineral density: a randomized clinical trial. Obstet Gynecol 2004;104:443-451.
(24.) Melamed M, Castano E, Notides AC, Sasson S. Molecular and kinetic basis for the mixed agonist/ antagonist activity of estriol. Mol Endocrinol 1997;11:1868-1878.
(25.) Siiteri PK, Sholtz RI, Cirillo PM, et al. Prospective study of estrogens during pregnancy and risk of breast cancer. http:// cdmrp.army.mil/bcrp/era/abstracts2002/p13_chemoprevention/9919358_abs.pdf
(26.) Ross RK, Paganini-Hill A, Wan PC, Pike MC. Effect of hormone replacement therapy on breast cancer risk: estrogen versus estrogen plus progestin. J Natl Cancer Inst 2000;92:328-332.
(27.) Li CI, Malone KE, Porter PL, et al. Relationship between long durations and different regimens of hormone therapy and risk of breast cancer. JAMA 2003;289:3254-3263.
Patrick N. Friel, BS--Steroids Department, Meridian Valley Laboratory Correspondence address: 801 SW 16th, Suite 126, Renton, WA 98055 E-mail: steroids@meridianvalleylab.com
Christa Hinchcliffe, ND--Private practice, Tahoma Clinic, Renton, WA
Jonathan V. Wright, MD--Medical Director, Tahoma Clinic, Renton, WA
COPYRIGHT 2005 Thorne Research Inc.
COPYRIGHT 2005 Gale Group