Continuous daily treatment with an estrogen and progestin provides an alternative therapeutic regimen to sequential hormone replacement therapy. Regular withdrawal bleeding in women who receive sequential therapy is a common reason for discontinuation of this treatment regimen. Doren and associates examined compliance, relief of climacteric symptoms and maintenance of lumbar bone density in women receiving sequential estrogen-progestin or continuous combined therapy.
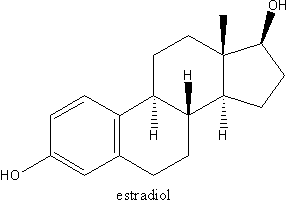
A total of 210 early and late postmenopausal women were randomized to receive either estradiol valerate, 2 mg daily, plus medroxyprogesterone acetate, 5 mg daily tor 12 days each month to induce withdrawal bleeding, or estradiol, 2 mg daily, plus estriol, 1 mg daily, and norethisterone, 1 mg daily, to maintain amenorrhea. Women in a control group did not receive any medication. Patients were evaluatea every six months for two years.
After one year, compliance was 93 percent in the group that received continuous therapy; at two years, compliance among these women was 73 percent. Compliance rates were 66 percent at one year and 49 percent at two years among women who received sequential therapy. Relief of climacteric symptoms did not differ in either group. The most common reasons for discontinuation of sequential therapy were the presence of withdrawal and irregular bleeding. Among women who received continuous therapy, discontinuation of therapy for the same reason was significantly less. Another major reason cited for dropout among women who received continuous therapy was the significant failure of the drug to control climacteric symptoms.
After hvo years, amenorrhea was achieved in 90 percent of the patients in the group receiving continnous combined therapy. In the group receiving sequential therapy, 82 percent of the patients still had regular withdrawal bleeding after two years. Weight and body height did not change in either group. Bone mineral density in the continuous therapy group was increased after two years. Differences from baseline compared with control subjects wene significant after both one year and two years. Compared with the control group, the group receiving sequential therapy did not have significant changes in bone mineral density after two years. Differences in bone mineral density among women in both study groups were sigmficant after two years. Among women in the control group, changes in bone mineral density were insignificant. Response to both therapies was as good in late as in early postmenopausal women and in women with low initial bone density.
The authors conclude that maintenance of amenorrhea in women who received continuous combined hormone replacement was the primary reason for improved compliance. Although preservation of bone mineral density was supenor in the continuous therapy group, neither treatment group achieved satisfactory climacteric symptom relief. (Doren M, et al. Superior compliance and efficacy of continuous combined oral estrogenprogestogen replacement therapy in postmenopausal women. Am J Obstet Gynecol 1995;173:14-51.)
COPYRIGHT 1996 American Academy of Family Physicians
COPYRIGHT 2004 Gale Group