Three events signal a new era for injectable contraceptives:
* A multinational epidemiological study by the World Health Organization (WHO) produced largely reassuring findings about the 3-month injectable depot medroxyprogesterone acetate (DMPA) and cancer. Previous controversy about DMPA had arisen from animal studies.
* The United States Food and Drug Administration (US FDA) approved DMPA as a contraceptive in 1992, 25 years after the manufacturer, the Upjohn Company, first applied. As a result, the United States Agency for International Development (USAID) has begun providing DMPA to developing countries; and
* Two new monthly injectables, Cyclofem [TM] and Mesigyna [R], are being introduced after thorough clinical studies by WHO (see pp. 4-5).
Together, these events may clear away some of the constraints that have limited widespread use of this 30-year-old method to a few countries.
Development of Injectables
Research on injectable contraceptives began shortly after the development of oral contraceptives. Karl Junkmann and colleagues at the German pharmaceutical firm Schering AG synthesized the first injectable progestins in 1953 (64, 149) and in 1957 developed norethindrone enanthate (NET EN, or Noristerat [R]), the first injectable contraceptive, which injected every two months (150). The pharmaceutical firm the Upjohn Company synthesized medroxyprogesterone acetate (Provera [R]) in the late 1950s (17). Upjohn conducted the first clinical trials of Provera in its depot, or injectable, form--Depo-Provera [R]--in 1963 (313, 321). Researchers developed the first monthly injectables and conducted clinical trials in the 1960s. The combination of progestin and estrogen that became Cyclofem was first tested in 1968, and the combination that became Mesigyna was first tested in 1974 (223).
US Regulatory History of DMPA
DMPA has always been the most widely used injectable, but the long wait for approval in the US has made it controversial. Upjohn applied for US FDA approval in 1967. At the time progestin-only methods seemed promising because the estrogen in combined oral contraceptives (OCs) caused nausea and vomiting in some women. Researchers suspected as well that estrogen caused blood clots (thromboembolic disease) in some users of combined OCs. These suspicions were later confirmed. Also, progestin-only contraceptive injections fulfilled many of the goals of researchers and family planning providers who wanted to be able to offer a method that was effective, reversible, did not interfere with lactation or require action at the time of sexual relations, and could be easily delivered by rural health care providers.
Nevertheless, the US FDA denied approval of DMPA in 1978, saying that it lacked sufficient evidence demonstrating safety, particularly with regard to breast and cervical cancer (35). A 3-member expert review panel, convened in 1983 at Upjohn's request, upheld the US FDA decision (322).
DMPA Research
Tests of DMPA in beagle dogs and monkeys in the early 1970s raised questions about cancer that delayed US regulatory approval and held back use in many countries. Beagles developed breast tumors and some monkeys developed endometrial tumors in tests then required by the USFDA of any new hormonal contraceptive (148). These studies were influential because at the time there was little information on the long-term effects of DMPA use among women (322). Many experts questioned the relevance to humans of the beagle and monkey studies, however (3, 10, 136, 313, 330, 346).
The WHO Collaborative Study of Neoplasia and Steroid Contraceptives examined the risk of cancer among users of hormonal contraceptives and reached the following conclusions, published largely 1991, about DMPA and cancer:
* Breast cancer: No increased risk overall, but the study found that DMPA users had an increased risk for several years after starting DMPA--perhaps due to accelerated growth of existing tumors. Some of the apparent increase in risk may be explained by detection bias (see p. 14).
* Cervical cancer: No increased risk of invasive cancer.
* Endometrial cancer: Protective effect.
* Ovarian cancer: No increased risk.
* Liver cancer: No increased risk.
The findings about breast and endometrial cancer were the most crucial because they answered the long-standing questions raised by animal studies.
The WHO study provided epidemiologic evidence that humans differ from these animals in their response to hormones. The US FDA no longer requires testing contraceptive hormones for carcinogenicity in beagles (148).
The WHO study led the US FDA to change its position in 1992 and approve DMPA. US FDA approval removed a source of controversy in the history of DMPA: use in developing countries of a drug that was not approved for contraceptive use in the US.
The US had been one of the few countries to withhold approval of DMPA. Over 90 countries had approved DMPA before the US (see Figure 1). Following US approval, India, the Philippines, and several other countries also approved DMPA. By comparison, NET EN is registered in over 60 countries. Registration does not necessarily mean, however, that a product is readily available.
Monthly Injectables
Monthly injectables have been most widely used in China and Latin America. Chinese Injectable Number 1 consists of hydroxyprogesterone caproate and estradiol valerate and has been used by about 1 million women (271). In Latin America at least one million women use dihydroxyprogesterone acetophenide and estradiol enanthate, which was originally developed by Squibb Pharmaceutical Company in the 1960s and marketed under the brand name Deladroxate. Within a few years Squibb withdrew Deladroxate, but the same formulation, manufactured by others, is now marketed in Latin America and Spain under a variety of other brand names (see Table 1). It has not been thoroughly studied (223, 331).
[TABULAR DATA OMITTED]
Two new monthly injectables, Cyclofem and Mesigyna, have completed multinational clinical trials conducted by WHO. They are being introduced in a number of countries.
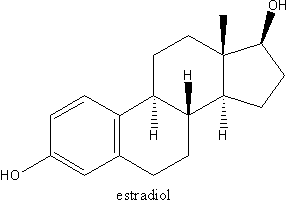
* Cyclofem, previously known as Cycloprovera, combines DMPA and the estrogen estradiol cypionate. The Upjohn Company developed Cycloprovera and turned it over to WHO in 1984.
* Mesigyna, developed by WHO, combines NET EN and the estrogen estradiol valerate.
Introductory trials of Cyclofem have been conducted in Chile, Indonesia, Jamaica, Mexico, Thailand, and Tunisia, and the new injectable has been registered in Guatemala, Indonesia, Mexico, Peru, and Thailand. The Concept Foundation, a private nonprofit organization set up by the Program for Appropriate Technology in Health (PATH) and given rights to Cyclofem by WHO, has licensed manufacturers in indonesia and Mexico to produce Cyclofem and has identified distributors in other countries, primarily in Latin America. The Upjohn Company has obtained rights to Cyclofem in the US and in several other developed and developing countries. Upjohn plans to submit an application for Cyclofem to the US FDA by August 1996 (318).
Schering AG is handling registration, distribution, and marketing of Mesigyna. Schering AG plans to begin marketing Mesigyna in Latin America. Mesigyna is manufactured in Mexico and has been registered in Argentina and Brazil as well as Mexico (74).
With new opportunities to offer injectables, policymakers, program managers, and providers need to reacquaint themselves with these contraceptives: their effectiveness and reversibility, side effects, and noncontraceptive benefits, why women use injectables, and how users respond to side effects. This knowledge can help program staff make decisions concerning communication and service delivery issues posed by injectables (see "Lessons Learned" on back of "DMPA at a Glance".
COPYRIGHT 1995 Department of Health
COPYRIGHT 2004 Gale Group