On May 31, 2002, the Women's Health Initiative (WHI) announced that the combined estrogen and progestin arm of the study was halted because the numbers of breast cancers, blood clots, and cardiac events exceeded the preset limits.1 In February 2004, the estrogen-only arm of the study was stopped as well, thus ending the intervention phase of the study.2
Since that time, many menopausal and postmenopausal women have discontinued hormone therapy (HT) due to fear of these risk factors, and are experiencing negative consequences of low estrogen levels, including urogenital atrophy. One alternative to HT for the treatment of urogenital atrophy is vaginal estrogen therapy. An often overlooked method of vaginal treatment is the estradiol acetate vaginal ring.
* Menopausal Symptoms
The acute symptoms of menopause are primarily vasomotor (hot flashes) and sleep disturbances. Vasomotor symptoms are usually short-lived. Nonhormonal treatments such as low-dose antidepressants (venlafaxin) are currently under investigation for relief of vasomotor symptoms. Chronic symptoms such as urogenital atrophy and osteoporosis become more important as the length of time after menopause increases. Osteoporosis can be at least partially treated by bisphosphonates, selective estrogen receptor modulators (SERMS), and lifestyle changes (calcium supplements, weight bearing exercise, and no smoking or drinking alcohol).
An estimated 15% of premenopausal and 10% to 40% of postmenopausal women experience dryness, burning, pruritis, irritation, and dyspareunia.3 Declining levels of estrogen contribute to atrophy of supporting tissues in the pelvic area, increasing the risk of prolapse and possibly predisposing older women to lower urinary tract symptoms.
Hypermobility of the bladder base and intrinsic urethra weakness increase the risk for stress urinary incontinence. Changes in the lactic acid metabolism and vaginal pH may increase the risk for infection.3 Oral estrogen therapy (ET) or HT have successfully treated these symptoms, but now that many women have discontinued HT, alternative treatments are necessary.
* Using the Vaginal Ring
Unlike oral HT, vaginal application of estrogen relieves urogenital atrophy without systemic effects. Also unlike oral estrogen therapy, progestins are not required for vaginal tablets or occasional estrogen cream use. Continuous use of vaginal estrogen cream or use of the higher dose systemic HT vaginal ring requires progestin for women with an intact uterus to prevent uterine endometrial proliferation.
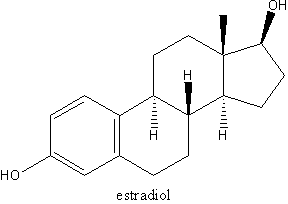
The Estring vaginal ring releases a low dose of estradiol (7.5 ug/24 hours) directly to the vaginal mucosa consistently over 90 days. Local administration of estrogen eliminates the metabolism of estradiol to estrone in the gut, resulting in a more physiological estradiol-to-estrone ratio.5 Patient acceptability is high6 because there is less "mess" than with vaginal cream, inadvertent overdose is not possible, and it only needs to be changed every 3 months.
Studies of the estradiol ring show that it is equal to Premarin cream in restoring the maturation of vaginal mucosa, decreasing vaginal pH and decreasing the number of urinary tract infections (UTIs) by 90%.7-9 Systemic absorption is minimal, leaving plasma estradiol levels unchanged, no detectable pharmacodynamic effects, minimal rates of drug interaction, and therefore, a high margin of safety.10 It is for this reason that vaginal estradiol rings may be considered for use by patients with breast cancer for the treatment of urogenital symptoms.11
* Vaginal Ring Benefits
The issue of endometrial stimulation, which is a problem for oral estrogen users, does not seem to be a problem with Estring. Naessen12 found no significant increase in endometrial thickness in 60 postmenopausal women using the vaginal ring.
Interestingly, there may be a beneficial lipid effect from vaginal ring use. These same investigators found that LDL levels, LDL:HDL ratios, total cholesterol, and apolipoprotein B levels all decreased with the use of vaginal rings.13 Also, bone metabolism and bone density were positively affected by vaginal ring use.
Why does the ring benefit lipid level and bone metabolism if it is not systemically absorbed in significant amounts? It's apparently possible that low estrogen levels over time cause the number of estrogen receptors in the body to increase and an up-regulation of these receptors occurs, resulting in a therapeutic effect with a very low dose.13
Sexual difficulties caused by vaginal atrophy are decreased with the use of the vaginal ring and, according to one study, most women and their partners reported no discomfort during sexual intercourse with the ring in place.14 Of course, all postmenopausal women should be encouraged to use vaginal lubricants for sexual activity, and vaginal moisturizers to reduce vaginal dryness, if needed. Finally, a recent Cochran Review15 found the estradiol vaginal ring an effective and acceptable treatment for vaginal atrophy. Its use should be complemented with health teaching about diet, exercise, and substance abuse, for all menopausal women.
REFERENCES
1. Rossouw JE, Anderson GL, Prentice RL, et al: Writing Group for the Women's Health Initiative Investigators. Risks and benefits of estrogen plus progestin in healthy postmenopausal women: Principal results from the Women's Health Initiative randomized controlled trial. JAMA 2002;288(3):321-333.
2. Anderson GL, Limacher M, et al: Women's Health Initiative Steering Committee. Effects of conjugated equine estrogen in postmenopausal women with hysterectomy. JAMA 2004;291:1701-1712.
3. Willhite L, O'Connell M: Urogenital atrophy: Prevention and treatment. Pharmacotherapy 2001;21(4):464-480.
4. Ouslander JG: Aging and the lower urinary tract. Am J Med Sci 1997;314:214-218.
5. Pharmacia and Upjohn. Product Monograph: Estring 1996.
6. Nachtigall L: Clinical trial of the estradiol vaginal ring in the U.S. Maturitas 1995;22 Supplement:543-547.
7. Barentsen R, van de Weijer P, Schram J: Continuous low dose estradiol versus estriol vaginal cream for urogenital atrophy. Eur J Obstet Gynaecol Reprod Biol 1997;71(1):73-80.
8. Eriksen B: A randomized, open, parallel-group study on the preventative effect of an estradiol-releasing vaginal ring (Estring) on recurrent urinary tract infections in postmenopausal women. AJOG 1999;180(5):1072-1079.
9. Henriksson L, Stjernquist M, Boquist L, et al: A one-year multicenter study of efficacy and safety of a continuous, low-dose, estradiol-releasing vaginal ring (Estring) in postmenopausal women with symptoms and signs of urogenital aging. AJOG 1996:176(1):85-92.
10. Gabrielsson J, Wallenbeck I, Birgerson L: Pharmacokinetic data on estradiol in light of the estring concept. Acta Obstetricia et Gynecologica Scandinavivca Supplement 1996;163:26-31.
11. Pritchard K: The role of hormone replacement therapy in women with a previous diagnosis of breast cancer and a review of possible alternatives. Ann Oncol 2001;12:301-310.
12. Naessen T, Rodriguez-Macias K: Endometrial thickness and uterine diameter not affected by ultra=-low doses of 17B-estradiol in elderly women. AJOG 2002;186:944-947.
13. Naessen T, Rodriguez-Macias K, Lithell H: Serum lipid profile improved by ultra-low doses of 17B-estradiol in elderly women. J Clin Endocrinol Metabl 2001:86-2757-2762.
14. Data on file. Pharmacia & Upjohn Company, Kalamazoo, Mich, 1006. [Pharmacokinetic Summary, US Trial Report (US), Australian Trial Report (AUS), Investigator's Brochure (IDB), Safety Update 03/31/95, ESTRING European Monograph, Pharmacia & Upjohn Forecast.]
15. Suckling J, Lethaby A, Kennedy R: Local oestrogen for vaginal atrophy in postmenopausal women (Cochrane Methodology Review). In: The Cochrane Library, Issue 4, 2003, Chichester, UK: John Wiley & Sons, Ltd.
Mary M. Cothran, PhD, CRNP Sandra Engberg, PhD, CRNP
ABOUT THE AUTHORS
At the University of Pittsburgh School of Nursing, Dr. Cothran is an assistant professor in the nurse practitioner program and Dr. Engberg is chair of the Department of Health Promotion and Development.
Copyright Springhouse Corporation Jul 2004
Provided by ProQuest Information and Learning Company. All rights Reserved