Management of the menopausal woman is more of an art than a science. For patients plagued by urogenital atrophy or vasomotor symptoms, such as hot flashes, night sweats, and insomnia, female hormones are among the most effective treatments.
Norra MacReady
They come in a variety of pills, creams, and patches that contain a range of active ingredients in a wide array of dosages.
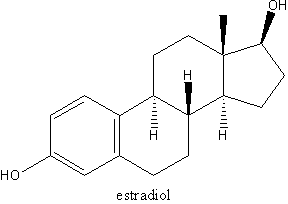
Until recently, hormone replacement therapy (HRT) was also used to help prevent other conditions that become common in older women, such as cardiovascular disease or osteoporosis. However, the results of several recent studies showed that women who took a widely prescribed estrogen-progestin combination had an increased risk of breast cancer and cardiovascular events, compared with women treated with placebo, especially after 5 or more years. This forced physicians and patients to reevaluate their use of these products. Currently they are recommended primarily to treat the vasomotor symptoms of menopause or atrophy of urogenital tissue. For most women at risk of heart disease or osteoporosis, other treatments are available.
The variety of hormone types and vehicles makes comparison across products difficult. Most physicians take a trial-and-error approach. Currently experts recommend that a woman use HRT for up to 2-3 years and then start tapering her use. Exogenous estrogen by itself increases the risk of endometrial cancer, so women with an intact uterus who take estrogen must take progesterone to counter that risk.
A menopausal woman also needs an overall management strategy tailored to her unique needs, including counseling on diet and exercise and recommendations on the use of over-the-counter items such as soy products and vaginal lubricating agents.
COPYRIGHT 2003 International Medical News Group
COPYRIGHT 2003 Gale Group