Think of menopause as a beginning. It's the chance to renew your commitment to a healthier lifestyle. All the changes your body is experiencing result in you taking a closer look at your health. During this time, you may have a lot of questions, especially about hormone replacement therapy (HRT). Taking supplemental estrogen may lower your risk of heart attacks and osteoporosis, but it could increase the chance of breast cancer in some cases.
Here are answers to some common concerns women have.
Q. Why am I gaining weight as I approach menopause?
A. Blame age, inactivity, and your declining metabolism--not the coming of menopause.
Metabolism, your body's internal calorie burner, drops 2 percent a year in your 40s, says Dr. Steven R. Goldstein, an obstetrics/gynecology professor at New York University. That means you need to eat less and exercise more to keep your weight steady.
"It's a myth that hormone replacement therapy causes weight gain," he says. Indeed, women on hormone replacement therapy gain an average of 2 pounds in the three years around menopause. But women who don't use HRT gain an average of 4 pounds.
Q. Can taking HRT cause cancer?
A. The latest studies, including a recent National Cancer Institute study, show that HRT does boost a woman's risk of breast cancer--though by how much depends on the years of use and type of HRT, says Dr. Mary Laya of the Women's Health Care Center at the University of Washington Medical Center in Seattle.
Use of estrogen alone increases your risk by 1 percent a year. Use of estrogen plus progesterone increases risk by 3 percent a year. Your doctor can best assess your situation with a computer program known as the Gail Model. Women with a uterus need to take progestin with estrogen to prevent uterine cancer, says Dr. Laya.
Q. Are "natural" estrogens as effective as prescription drugs?
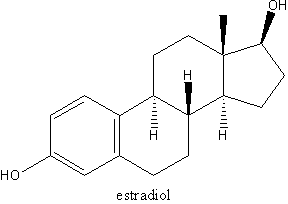
A. "Natural" estrogens--or the plant-based estrogens found in soy, black cohosh, and dong quai--are much weaker forms of estrogen than prescription drugs, such as Premarin, says Dr. Susan M. Lark, author of The Estrogen Decision.
As a result, natural estrogens may help control mild hot flashes, depending on the woman. But soy, along with prescription alternatives, will not adequately protect against heart disease and brittle bones, which are greater risks after menopause. "Plant estrogens are one thousand-fold less powerful than prescription estrogens," says Dr. James Liu, director of reproductive endocrinology at the University of Cincinnati. "The amount of soy products you'd need to ingest would be enormous to get the same benefits."
And adding plant estrogens to your diet in your 40s may be too late, says Dr. Carolyn Runowicz, president of the Society of Gynecologic Oncologists and coauthor of The Menopause Book: A Guide to Health and Well-Being for Women After Forty. "In Asia, where menopausal side effects are few, benefits may result because women start eating soy early in life. Also, they actually eat the product with soy in it, like tofu, instead of taking a pill."
Pills won't do the job. A Mayo Clinic study of 177 women reported in the March Journal of Clinical Oncology that supplements did not lessen or stop hot flashes. Additionally, ingredients in supplements, including the level of estrogen, aren't guaranteed since supplements aren't subject to Food and Drug Administration (FDA) standards.
Recent studies of menopausal women at Montefiore Medical Center in the Bronx, where Dr. Runowicz works, indicate a possible link between the estrogenic herb black cohosh and uterine cancer, which is estrogen-driven. "The only sources of estrogen we could find in these women were herbal supplements," she says.
Q. What's perimenopause? How do you know when you're in it?
A. Perimenopause begins 5 to 10 years prior to menopause. During this time the ovaries' production of eggs slows, progesterone dwindles, and estrogen levels vary--sometimes surging and sometimes waning.
Most women enter this phase around age 45 and may notice symptoms such as irregular periods, hot flashes, insomnia, and poor concentration. "It's hard to know if these are symptoms of menopause, aging, or just circumstances in your life," Dr. Runowicz says. "It's an age when people in their lives may be dying, women may be going through divorce, and their kids may be leaving home."
Some women have no signs of pending menopause. In those cases, a doctor can detect perimenopause through blood tests of estrogen and a follicle-stimulating hormone.
Q. Is taking estrogen through a patch more efficient than a pill?
A. Postmenopausal women who take estrogen have a much lower rate of cardiovascular disease than women who don't take it. And each hormonal replacement therapy has its advantages. The patch releases hormones directly into your bloodstream through your skin and needs changing only every three days to a week, Dr. Runowicz says.
The pill, taken daily, boosts HDL or "good" cholesterol by 6 to 8 percent and lowers LDL or "bad" cholesterol by up to 15 percent within weeks--compared to six months for the patch. The pill is speedier because estrogen goes directly to the liver, where the body produces and metabolizes cholesterol.
Q. Can I take birth control right up until menopause starts?
A. Yes, as long as you're not a smoker and don't have cardiovascular disease. A follicle-stimulating-hormone test taken during your pill-free week can alert you once you have entered menopause.
Q. How do I survive hot flashes?
A. Four out of five women will experience hot flashes during perimenopause. A hot flash lasts from 30 seconds to five minutes and may be followed by the chills. "The good news is that most women only have severe hot flashes for a year to 30 months at most--and then they're over the hump," says Dr. Goldstein, who also coauthored the book Could It Be Perimenopause?
There are alternative ways to reduce flashes if you don't want to use HRT. Some women find it effective to avoid caffeine, alcohol, spicy foods, and hot beverages. Others lower stress through deep breathing and other relaxation techniques. Dr. Barbara Soltes, director of Women's Health Research Center at Rush-Presbyterian St. Luke's Medical Center in Chicago, recommends taking low-dose birth control pills during perimenopause.
A study by Bowman Gray Medical School in North Carolina showed that women were able to reduce hot flashes noticeably by taking 2 tablespoons of soy powder daily. Some doctors believe Siberian ginseng, dong quai, and black cohosh (80-160 mg) or vitamin E (400-800 IU) also may help, but benefits may stem from the placebo effect or power of suggestion. Indeed, placebo-controlled trials show no benefit for black cohosh or vitamin E, say Dr. Runowicz and Dr. James Liu, director of reproductive endocrinology at the University of Cincinnati.
In addition to HRT, Paxil and other antidepressants can alleviate hot flashes.
Q. How can menopause affect your sex life?
A. Some women experience vaginal dryness, which generally can be relieved with a lubricant such as Vagisil, Astroglide, or Replens. Estring, a low-dose estrogen ring inserted into the upper part of the vagina, also can restore estrogen to the area for more than three months. There are vaginal creams, but Dr. Runowicz warns against using them. "A woman has to be very skilled to get the tiny amount needed into the vagina."
Exercise can also help. It promotes blood flow throughout the body.
"Menopause should be viewed as the prime of life," Dr. Soltes says. "This is a time when you've achieved many of your goals and can switch careers, go to school, or pick up new hobbies. Plus, you no longer have to fear getting pregnant. It's a new freedom."
Nonetheless, sexual drive may decline, but it's a matter of age. "It's a protective mechanism," Dr. Runowicz says. "If you had the libido of an 18-year-old and the heart of 60-year-old, you could get yourself into trouble."
Q. I'm worried about osteoporosis. What are the other options beside HRT?
A. Bone loss is greatest in the first 5 to 10 years after menopause and can be assessed through a painless bone-density test. Ask your doctor about getting an exam.
Weightlifting and weight-bearing exercise--such as dancing, running, walking, stair climbing, or cross-country skiing--can help fight bone loss, if done at least two hours a week, according to the National Osteoporosis Foundation. Also, taking 1,500 mg of calcium, 600 mg of magnesium, and 400 mg of vitamin D a day is essential.
In addition to a calcium supplement, you can take Fosamax (Alendronate), a prescription drug that inhibits the osteoclasts that break down bone. Other options include taking SERMS (selective estrogen receptor modulator) or Evista (Raloxifene). The FDA is expected to approve two new treatments, Tibolone and Estrogel, sometime this year.
COPYRIGHT 2000 Meredith Corporation