Immunoglobulin A (IgA) has been a special interest of mine as a major yardstick in assessing and treating endocrine-immune diseases. IgA is the most abundant antibody and is especially important in mucosal immunity. It is an essential protective factor against infectious agents, allergens, and foreign proteins that enter the body via the mouth, nose, upper respiratory tracts, intestines, and the reproductive tract. (1)
In humans, IgA deficiency is recognized as the most frequent immunodeficiency. (2) Older studies suggest that up to two-thirds of individuals with IgA deficiency are healthy, but such conclusions are based on healthy blood donor subjects in whom deficiency has been determined from initial screening without any follow-up. (3) Recent studies indicate that as many as 80% of those who are IgA deficient, but healthy, may develop synopulmonary infections, allergies, autoimmune diseases, and gastrointestinal diseases, especially celiac disease, as well as gut and lymphoid malignancies. (4)
In animals, I routinely find low IgA blood levels associated with malabsorption and intestinal tract inflammation. This impairs the animal's ability to absorb both nutrients and medications. An IgA deficiency is seen in gingival buccal inflammation, glossitis, esophagitis, gastric enteritis, and food sensitivities.
[GRAPHIC OMITTED]
IgA deficiency is also present in the following: respiratory system problems such as rhinitis, hay fever, pharyngitis, pneumonitis, and asthma; inflammatory problems of the kidneys, bladder, and urethra (often kidney and bladder stones are consequences of the imbalance); inflammatory reproductive tract disorders involving the uterus, ovaries, vagina (and frequently in early abortion cases); inflammatory joint disorders such as rheumatoid arthritis; and in patients who develop vaccine reactions.
It should be noted that these findings of IgA deficiency do not occur exclusively, that is, they typically appear as part of an overall pattern of humoral immune deficiency. I also test for IgM and IgG levels and find that low IgA is usually accompanied with similarly low levels of IgG and IgM. It should also be noted that if in fact antibody readings are not all decreased there is a strong possibility of inaccurate lab results, since antibodies tend to rise or fall across the board, rather than in isolation.
Causes of IgA Deficiency
In my experience, compromised immunity--including IgA deficiency--among canines and felines stems from endocrine-immune destabilization originating with the zona fasciculata's inability to produce adequate cortisol.
Cortisol, a pivotal anti-inflammatory hormone, is the primary secretion of the adrenal glands in dogs and humans. (5) It also promotes the release of glucose to fuel the emergency response to danger and regulates the immune system. Normal cortisol activity is almost certainly required for proper immune response, according to leading glucocorticoid researchers. (6)
A cortisol deficiency in cats and dogs, which I first reported in 1976, appears to be largely a genetic defect (7) and quite likely exacerbated by current breeding practices. (8) I have found that deficient cortisol and IgA-related diseases occur through generations of families.
Other possible causes of cortisol deficiency include stress and toxicity, which may be significant acquired causes of cortical dysfunction. Harvey points out that the adrenal gland is the most vulnerable organ in the endocrine system for toxins, and within the adrenal gland the majority of effects occur in the cortex. Such disturbances can "fundamentally affect the whole body physiology and biochemistry." (9) Cortisol release is controlled by a classical feedback loop within the hypothalamic-pituitary-adrenal axis. The hormone is stimulated by hypothalamic corticotropic-releasing factor (CRF) and pituitary adrenocorticotropic hormone (ACTH). When blood concentrations rise to a certain level, cortisol inhibits CRF secretion. This then inhibits ACTH and cortisol secretion.
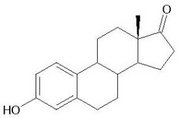
The androgens dehydroepiandrosterone (DHEA) and dehydroepiandrosterone sulfate (DHEAS) are the most abundant circulating hormones in the body. Known as prohormones because they metabolize into other hormones, these substances are primarily made in the zona reticularis strata of the adrenal cortex. They convert to androstenedione, androstenediol, testosterone, and further to the estrogen compounds estrone and estradiol. (10)
Androstenedione is the most important precursor of estrone, the most abundant circulating estrogen in postmenopausal women. Androstenediol, converted from DHEA, has inherent estrogenic activity. (11)
When the zona fasciculata cannot make enough cortisol, or for some reason the cortisol is excessively bound (inactive) and thus not recognized by the system, more ACTH is released by the pituitary to stimulate more cortisol. The zona reticularis also responds to ACTH. This tissue, as noted above, produces androgens that convert in some degree to estrogen compounds.
Excess estrogen promotes CRF release from the hypothalamus and more ACTH from the pituitary. This errant cycle appears to introduce a physiologically significant amount of extra estrogen into the system. Studies in humans show that estrogens inhibit cortisol synthesis by specific interference with enzyme activity. (12) If there is a cortisol deficiency to begin with, added estrogen would appear to exacerbate the deficiency and worsen the overall imbalance.
The term "estrogen dominance" has become popular in recent years. It is generally thought of as a symptom-inducing imbalance between estrogen and progesterone in women resulting from excess estrogen generated by ovarian activity, birth control pills, estrogen-like compounds in food, and other estrogen-mimicking compounds in the environment. A problem of excess estrogen, originating with dysfunction in the adrenal cortex, has not been considered. In animals, I have repeatedly found elevated estrogen levels in female patients who are intact--though out of estrus--or spayed as well as intact or neutered males. The assumption is that the excess estrogen stems from adrenal precursors.
Hormone balance is regarded as a crucial factor in the regulation of immune and inflammatory responses. Generally, estrogens in physiologic concentrations enhance humoral immune responses and depress cellular-mediated responses. At higher and pharmacological concentrations they have a number of inhibitory actions. Elevated estrogen, for instance, is associated with atrophy of the thymus gland. Androgens tend to suppress both humoral and cellular types of immune mechanisms. (13) However, the complex mechanisms through which sex hormones regulate immune and inflammatory responses are poorly understood. (14)
From a veterinary clinical experience of 38 years based on testing and treating thousands of animals, low cortisol and elevated estrogen clearly exert negative, and often catastrophic effects on the immune system. These effects consistently include lost disease protection as measured by reduced IgA, as well as low IgG, IgM, and T cell counts, and observable clinical signs of inflammation and disease. After so many cases, it has become abundantly clear to me that hormones in balance uphold immune system homeostasis, and hormonal imbalance destabilizes the system.
Testing
I developed an endocrine-immune blood test that monitors cortisol; total estrogen; T3 and T4 thyroid hormone; and IgA, IgM, and IgG antibody counts. Comprehensive tests like these are not routinely utilized by either veterinarians or physicians. I initially included T cell counts in the protocol but dropped it because of the added lab costs to clients.
Cortisol itself, even if the value is normal, may be bound (inactive) to varying degrees in different patients. This is why it is essential to look at cortisol-estrogen-immunoglobulin relationships. The practitioner will recognize a cortisol problem if the estrogen level is high and the immunoglobulins are low.
Standard tests measure only one component of estrogen: estradiol. Total estrogen is a more accurate measurement since estrone levels can vary. Estrogens can exert a dramatic blocking effect on cortisol and thyroid hormones; just a slight variation out of the normal range is enough to cause hormonal and immune complications. In the presence of elevated estrogen, thyroid hormone may be bound or rendered inactive to varying degree, enough to slow down overall metabolism, and trigger additional problems. Thyroid activity may, in fact, be significantly compromised even if the thyroid values in the blood test appear normal.
The critical value of this blood test is that it offers a comparative view of endocrine-immune relationships. In this case, the relationships are usually low cortisol, high estrogen, and low immune cells. After two weeks it is important to retest, and periodically thereafter. Retesting provides a gauge for determining the accuracy of the therapy and for making adjustments as needed. If the immunoglobulin values increase, and symptoms decrease, the course of treatment is correct.
Treatment
Endocrine-immune imbalance is treated in a straightforward way. Cortisone preparations have many of the chemical actions of cortisol. They are, in fact, converted to cortisol in the body. The central modality I have used for 30 years is cortisol replacement with relatively low dosages of various cortisone preparations.
A second key modality, necessary in canine cases, is the parallel use of thyroid supplementation. (For some apparent species variation, only 10% of feline cases require thyroid.) Elevated estrogen has a binding effect on thyroid hormone. As a result, metabolic activity may become retarded, impairing detoxification and the liver's ability to process the cortisone medication. Thus, even low-dosage cortisone may accumulate in the body and, over time, create side effects. By giving cortisol and thyroid replacement simultaneously, at least in dogs, the patient is able to effectively utilize and process the former without side effects. Adjunctive thyroid should be considered in applying this approach to humans.
I consider 70-170 mg/dl the normal range for IgA in dogs and cats. Below 60 mg/dl suggests the presence of malabsorption wherein patients are unable to absorb oral cortisone. In such cases, animals are treated with IV (if they are critical) or IM cortisone. Malabsorption can be a significant factor even though there are no obvious clinical signs. Retesting after two weeks usually shows an increase in the IgA level. When IgA reaches 60 mg/dl, most animals are able to take oral medications. A small percentage requires continued IM treatment.
Correction of the endocrine-immune imbalance with appropriate low-dosage cortisone (along with thyroid replacement in dogs) generally restores immunocompetence and health, even in critical cases. Animals deteriorate when therapy is stopped and signs of previous illness return.
William Jefferies, emeritus clinical professor of internal medicine at the University of Virginia, has reported in great detail on the safe and effective use of long-term physiologic dosages of cortisone for a variety of human illnesses involving adrenocortical deficiency--allergies, autoimmune disorders, and chronic fatigue, to name but a few. This clinical perspective has been essentially ignored by the medical community because, as Jefferies notes, the "unique situation in which a normal hormone, one that is essential for life, has developed such a bad reputation that many physicians and patients are afraid to use it under any circumstances." (15)
Jefferies maintains that indefinite replacement with physiologic dosages of cortisone will benefit many, if not all, human patients with chronic allergies and autoimmune disorders, and that replacement should not be stopped upon initial remission. (16)
The treatment funds an adrenocortical deficit, corrects a hormonal derangement, resets the metabolism, and restores effectiveness to the immune system. Used therapeutically, it can save animals who might otherwise be destined for euthanasia. Used preventively to determine the presence of imbalance in asymptomatic animals, it can help avoid future suffering and premature death.
Human Health Implications
Does this endocrine-immune disturbance exist in humans? And if so, can a similar treatment protocol be applied?
The imbalance exists in every animal cancer case I have tested. Therapy outcomes are usually positive when combined with excision, chemotherapy, or radiation, even in advanced cases.
The feline immunodeficiency virus (FIV) involves a retrovirus similar to HIV. Veterinarians routinely euthanize symptomatic cats, yet I have a 70% recovery rate among such patients. They remain disease-free as long as they are maintained on low-dosage cortisone. Cats testing positive for the virus do not develop clinical signs once they go--and stay--on the program. Perhaps when a human is exposed to the HIV virus, whether or not he or she develops symptoms of AIDS may depend on the strength of their endocrine-immune connections. If an imbalance is found through testing, correction with appropriate hormone replacement could be a significant strategy for both prevention and therapy.
Can this imbalance contribute to human inflammatory bowel conditions? There is currently an epidemic of inflammatory gut conditions among dogs and cats. The imbalance, revealed by low IgA, is present in all affected animals tested. When the imbalance is corrected with therapy, IgA rises, absorption improves, and clinical signs resolve.
The same approach works for IgA-related conditions elsewhere. Animals with other chronic bowel disorders (including food allergies), respiratory and urinary tract disorders, and anaphylactic and vaccine reactions invariably have abnormal IgA levels, and improve after treatment.
I suggest that interested physicians test for the same range of hormonal-immune relationships in humans that I test for in animals: cortisol, total estrogen, thyroid T3 and T4, and IgA, IgG, and IgM immunoglobulins. Other factors could be added, such as T cells and the androgen precursors of estrogen, in order to develop a more precise picture. Researchers have begun looking at the immune and inflammatory modulating effects of androgen/estrogen ratios and concentrations. (17)
My clinical findings indicate there is a significant need to test for IgA in routine diagnostics, both human and veterinary, because of the importance of mucosal immunity for health. Currently, this is not done.
What is "Normal"? The Case for Standardizing Blood Level Scores
I requested several nationally known laboratories to provide the high and low levels against which they measured the blood samples physicians had provided. (See the chart) The wide variation in results seems inexplicable until one realizes that labs are largely responsible for determining "normal" ranges on their own--and often they base that determination on the last 200 to 300 blood tests run, rather than a set standard.
As a result, physicians tend to distrust lab results--and with good reason. Without a national standard defining "normal," it is problematic to determine if a score is abnormal. Standardizing "normal" levels among labs would allow physicians to evaluate readings more accurately and consistently.
The discrepancies make meaningful comparisons, consultations, and discussion difficult among interested physicians. A patient may be healthy according to one laboratory's standard for normal, but unhealthy according to another's. Standardized CBC and blood chemistry levels are more or less accepted. Why is there not a similar standardization in major immune factors to help in diagnosis and treatment?
An additional factor to consider for female patients is the fluctuating nature of ovarian estrogen. The level of total estrogen will obviously vary according to monthly cycle, age, use of birth control pills, and/or estrogen replacements. One physician who uses hormones routinely in his practice was surprised to find that his sickest postmenopausal (non-ERT) patients had high estrogen levels and low antibody counts. A possible reason for this is the impact of low/bound cortisol and added estrogen from adrenal androgen conversion--a frequently overlooked source of estrogen. Estrogen synthesis is known to increase in nonovarian tissues as a function of age and body weight. (18) Even postmenopausal women may actually be in a state of relative estrogen dominance.
Accurate test results among reproductive age women must account for and quantify ovarian estrogen's normal fluctuations throughout the menstrual cycle. This can be done by testing reproductive age females twice, once on the seventh day, when ovarian estrogen reaches its lowest level, and again on the twenty-first day, when estrogen is highest. The difference between the two values will reflect endogenous and exogenous non-ovarian estrogen in the system.
The clinician might also want to obtain a 24-hour urine sample from the patient in order to test for active T3, T4, cortisol, total estrogen, and any other relevant markers. This would allow for a comparison of blood values, which may test normal but in fact involve significantly bound hormones. Without the urine test for comparison it can be difficult to determine if a hormone is available to the system or not.
Humans, like most canines, may require long-term thyroid replacement in addition to cortisone. Many humans have low thyroid despite normal values in blood tests. If thyroid function is low and the body's detoxification processes are operating sluggishly, even physiologic dosages of cortisone could accumulate over time and generate the side effects typical of pharmacologic dosages. This was my initial experience in treating canines until adjunctive thyroid replacement was introduced.
Conclusion
I have not found comparable imbalances described in veterinary literature to match the scope of health-destroying suppression/destabilization of the immune system found in household pets created by deficient or bound cortisol and elevated estrogen.
In animals, genetics appears to play a major role. In humans, congenital adrenal hyperplasia (CAH) has some similarities. This condition is characterized by a deficiency of cortisol and an increase in androgens, the result of a deficiency in the adrenal enzymes that produce cortisol. Once considered a rare inherited disorder with severe manifestations, a mild form is said to be common although frequently undiagnosed. Patients with the mild form are often unable to mount sufficient stress responses to trauma and infection. (19)
Is it possible that a similar enzyme disturbance could be operating in household pets? This may be the case, however, I have not tested for enzyme deficiencies nor for the androgen levels.
There are at least two clear dissimilarities. CAH involves hypertrophy of the adrenal glands and frequent deficiency of aldosterone, the mineralocorticoid produced by the outer layer of the cortex. No such situations are present in animals with the endocrine-immune imbalance.
One can speculate that a cortisol defect could be passed on to offspring if both parents are affected. In generations of animals an escalating severity of conditions related to this mechanism takes place. Might there be a parallel development among humans, with allergies and malabsorption in one generation and autoimmune diseases and cancer in the next?
Toxicity, as Harvey's work indicates, is another plausible explanation for adrenal malfunction.
Selye's famous work a half-century ago demonstrated that cortisol deficiency is a clear consequence of prolonged stress and contributes to some of the "diseases of civilization." (20)
Jefferies has examined the effects of mild cortisol deficiency due either to primary adrenal malfunction or secondary to inadequate stimulation by the pituitary or hypothalamus. He has reported that physiologic dosages of cortisone can improve a number of human disorders.
Recently, other medical researchers have reported successful applications of low-dosage cortisone in rheumatoid arthritis and polymyalgia rheumatica, a systematic inflammatory disorder of the aged. (21) CAH is treated, in part, with cortisone replacement. (22)
The veterinary clinical experience shows that a low-dosage cortisone approach is hugely beneficial and safe for restoring lost immune competence, including deficient IgA, and reversing clinical signs of disease. In this approach, testing for a serum IgA level, serves as a useful indicator at baseline of a hormonal disturbance to immune function, and specifically mucosal tissue immunity and inflammation. Once therapy has been initiated it again serves as an indicator of therapeutic progress. IgA counts are not generally conducted, however, it may be of great diagnostic and therapeutic value to do so.
Open-minded veterinarians who have applied this testing and therapy approach have obtained excellent results. It has not been tested, however, in controlled studies. Nor has it been studied in humans. Such research is beyond the scope of clinicians, however, a controlled study on this testing and treatment method could produce major diagnostic and treatment break-throughs for humans.
Alfred Plechner, DVM, is the author of Pets at Risk: From Allergies to Cancer, Remedies for an Unsuspected Epidemic and Endocrine-Immune Mechanisms in Animals and Human Health Implications. Contact Dr. Plechner through his web site: www.drplechner.com
References
1. Takahashi, I, Kiyono, H. Gut as the largest immunologic tissue. Journal of Parenteral Enteral Nutrition, 1999; 23: Suppl S7-12.
2. Primary immunodeficiency diseases. Report of an IUIS scientific group. Clinical and Experimental Immunology, 1999; 118 (supplement 1): 1-17.
3. Cunningham-Rundles, C. Disorders of the IgA system. In: Stiehm ER, ed. Immunologic disorders in infants and children, 4th ed. Philadelphia: WB Saunders, 1996:423-42.
4. Koskinen, S. Long-term follow-up of health in blood donors with primary selective IgA deficiency. Journal of Clinical Immunology, 1996; 16: 165-70.
5. Nelson, Don H., Samuels, L. T., A Method for the Determination of 17-Hydroxy Corticosteroids in Blood: 17-Hydroxy Corticosterone in the Peripheral Circulation. The Journal of Clinical Endocrinology and Metabolism, 1952, 12: 519-26.
6. Munck, A., Guyre, P. M. Glucocorticoid effects on immune responses. Unpublished paper.
7. Plechner, A. J., Shannon, M. Canine immune complex diseases. Modern Veterinary Practice, November 1976; 917. Plechner A. J. An effective veterinary model may offer therapeutic promise for human conditions: roles of cortisol and thyroid hormones. Medical Hypotheses, 2003, 60 (3): 309-14).
8. Lemonick, M. D. A Terrible Beauty: An obsessive focus on show-ring looks is crippling, sometimes fatally, America's purebred dogs. Time, December 12, 1994; 65.
9. Harvey, P. W. The Adrenal in Toxicology: Target Organ and Modulator of Toxicity, Bristol, PA (Taylor & Francis), 1996: 7.
10. Parker, L. N. Adrenal androgens. In: Endocrinology (ed: DeGroot), Third Edition, Philadelphia: W.B. Saunders Co, 1995: 1836-47.
11. Adams, J. B. Control of secretion and the function of C19-delta 5-steroids of the human adrenal gland. Molecular and Cellular Endocrinology 1985, 41: 1-17.
12. Gell, J. S., et al. Effect of estradiol on DHEAS production in the human adrenocortical cell line, H295R. Journal of the Society for Gynecologic Investigation, 1998, 5: 144-48.
13. Cutolo, M., Seriolo, B., Villaggio, B., Pizzorni, C., Craviotto C, Sulli A. Androgens and estrogens modulate the immune and inflammatory responses in rheumatoid arthritis. Annals of the New York Academy of Sciences, June 2002, 966: 131-42.
14. Cid, M., Schnaper, H. W., Kleinman, H. Estrogens and the vascular endothelium. Annals of the New York Academy of Sciences, June 2002, 966: 143-57.
15. Jefferies, W. McK. Mild adrenocortical deficiency, chronic allergies, autoimmune disorders and the chronic fatigue syndrome: A continuation of the cortisone story. Medical Hypotheses, 1994; 42; 183-189.
16. Jefferies, ibid.
17. Cutolo, M., et al. Androgens and estrogens modulate the immune and inflammatory responses in rheumatoid arthritis. Annals of the New York Academy of Sciences, June 2002, 966: 131-142.
18. Gruber, C. J., et al. Production and actions of estrogens. New England Journal of Medicine, 2002, 346 (5): 340-52).
19. Deaton, M., et al. Congenital adrenal hyperplasia: Not really a zebra. American Family Physician, March 1, 1999: 1190.
20. Selye, H. Studies on adaptation. Endocrinology, 1937, 21; 169 (17).
21. Hickling. P., et al. Joint destruction after glucocorticoids are withdrawn in early rheumatoid arthritis. British Journal of Rheumatology, 1998; 37: 930-936. Cutolo M, et al. Cortisol, dehydroepiandrosterone sulfate, and androstenedione levels in patients with polymyalgia rheumatica during twelve months of glucocorticoid therapy. Annals of the New York Academy of Sciences, June 2002, 966: 91-96.
22. Deaton, M., et al, op. cit., 1190.
by Alfred J. Plechner, DVM
COPYRIGHT 2005 The Townsend Letter Group
COPYRIGHT 2005 Gale Group