Byline: D. Reddy
Epilepsy affects 50 million people worldwide. Women may be afflicted with catamenial epilepsy, a form of epilepsy related to the menstrual cycle. In catamenial epilepsy, seizures are clustered around the monthly cycle. Despite the availability of several standard and newer antiepileptic drugs, there is no specific and effective therapy for catamenial epilepsy. Moreover, the exact pathophysiology of catamenial seizures remains unclear. It is well known that progesterone possess anticonvulsive properties. The level of this hormone drops near the end of the cycle, leaving women more vulnerable to catamenial epilepsy. Recent studies have shown how progesterone protects women against seizures. Progesterone plays two roles in the brain. First, it binds to progesterone receptors in the brain, which help regulate the reproductive functions. Second, progesterone gets metabolized to allopregnanol-one in the brain called a neurosteroid. We found that allopregnanolone plays a crucial role in seizure protection. The withdrawal from this neurosteroid, which occurs during the menstrual cycle, could provoke seizures. Consequently, we suggest that neurosteroid replacement could be a novel therapeutic approach for catamenial epilepsy.
Introduction
Epilepsy is a neurological condition characterized by repeated seizures, which are clinical manifestations of abnormal electrical discharges in the brain. Epilepsy is the second most common neurological disorder in India.[1],[2] Epilepsy affects an estimated 7 million people in India, and 50 million worldwide. Approximately 40% of them are women. The prevalence of epilepsy is 0.7% in India, which is comparable to the United States and other developed nations. The estimated incidence rate ranges from 40 to 60 per 100,000 population per year. The WHO estimated that approximately 80% people with epilepsy live in developing countries and most of them do not get adequate medical treatment. Among the two distinct epileptic seizures (partial and generalized), the bulk of cases in India belong to generalized seizures. Antiepileptic drugs (AEDs) are the mainstay for the treatment of epilepsy, and generally suppress seizure occurrence. [Table 1] None of these agents, however, meet the characteristics of an ideal AED, that is, protecting against seizures without inducing adverse effects that impair the patient's quality of life . Despite many advances in epilepsy research, the pharmacotherapy of epilepsy remains largely empirical owing to the lack of understanding of the underlying pathology. Moreover, approximately 30% of people with epilepsy have "intractable seizures" that do not respond to even the best available treatment.
Epilepsy is characterized by the unpredictable occurrence of seizures. However, there is a form of epilepsy, called catamenial epilepsy, which does not adhere to this lack of pattern. Catamenial epilepsy, from the Greek katomenios meaning "monthly", is a disorder that affects up to 70% of women with epilepsy. It is characterized by seizures that cluster around specific points in the menstrual cycle. [Figure 1] There are three patterns: perimenstrual, periovulatory, and inadequate luteal-phase seizures. However, t he bulk of attention is focused on the most common type, perimenstrual. In the primary clinical type, perimenstrual catamenial epilepsy, the seizures are clustered in an approximately 7-day period surrounding the menstruation.[3] Many women with this condition experience an increase in seizure activity before, during, or after the onset of menstruation. Catamenial seizures are common among women with focal or generalized epilepsy. Despite emerging information, very few physicians seem to know about menstrual cycle-related seizures. The diagnosis of catamenial epilepsy is mainly based on the assessment of menstruation and seizure records. A detailed diary of seizures and menstrual cycle would be important for accurate diagnosis of catamenial epilepsy. In general, a twofold or greater increase in seizure frequency during a particular phase of the menstrual cycle could be considered as catamenial epilepsy. A detailed understanding of the pathophysiology is essential for the development of rational approaches for the prevention and treatment of catamenial epilepsy.
Pathophysiology
Catamenial epilepsy has been identified and studied for many years with early reports from as long ago as 1881. Despite that, the molecular mechanisms beneath the development of this condition are not well understood. There is presently no specific treatment, and often, conventional therapies have a disappointing lack of effect. Recently, studies have suggested that various hormonal changes that are experienced during the menstrual cycle play a large role in the increased seizure susceptibility. The specifics of these fluctuations and their effect on and in the brain in relation to epilepsy must be determined in order to develop specific, targeted therapies. Many different possibilities for the development of catamenial epilepsy have been proposed, from fluctuations in antiepileptic drug levels to changes in the fluid and electrolytes balance.[4], [5] AEDs provide satisfactory control of seizures in most patients, but some AEDs such as phenytoin, carbamazepine, and phenobarbital are potent inducers of liver cytochrome P450 enzymes.[6] This AED-induced enzyme induction leads to enhanced metabolism of steroid hormones,[7] which may play a role in breakthrough seizures in women. Moreover, the use of the enzyme-inducing AEDs phenobarbital, phenytoin, and carbamazepine increases serum sex hormone-binding globulin (SHBG) concentration in women with epilepsy, which may result in diminished concentrations of "free" or "biologically active" forms of steroid hormones. Overall, cyclical changes in the circulating levels of estrogens and progesterone are now widely accepted to be important in the development of this disease. [Figure 1] Research has shown that female sex hormones can act on certain cells in the brain, particularly those in the area of the temporal lobe. Generally, estrogens are found to be proconvulsant, whereas progesterone has the opposite effect and reduce seizures.[5] Alternations in seizure activity may also be seen during changes in reproductive status (i.e., while entering puberty, during pregnancy, or after menopause).
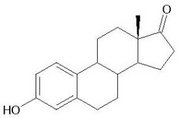
Estrogen
There are three biologically active forms of estrogen: 17?-estradiol, dominant in pre-menopausal women; estriol, the major form of estrogen during pregnancy; and estrone, which is prevalent after menopause. Estradiol has been shown in many studies to have significant proconvulsant effect.[8] It facilitates various forms of induced seizures and has been shown to worsen seizures in women with epilepsy. On a cellular level, estradiol, aside from its normal reproductive effects, enhances neural excitation and suppresses inhibition. It also creates changes in the physical properties of some neurons (increase in excitatory dendritic spine density in the hippocampus), resulting in increased potential for seizures. It has been observed that there is a relationship between the ratio of estrogen to progesterone and the level of seizure occurrence.[9],[10] An increase in this ratio during certain periods in the menstrual cycle could create the increase in seizure susceptibility observed in catamenial epilepsy.
Progesterone
Progesterone has long been known to have anticonvulsant properties.[11],[12] Both animal models and human clinical studies have shown the efficacy of progesterone in reducing both the frequency and severity of seizures. The clustering of seizures around the beginning of menstruation corresponds with a significant drop in the levels of progesterone circulating in the body and an increase in the estrogen: progesterone ratio. There is strong evidence that, rather than the increase in estrogens, it is the decrease or "withdrawal" of progesterone that partly stimulates catamenial seizure exacerbation. These withdrawal effects could be highly relevant in "perimenstrual" catamenial epilepsy.[4],[5] The luteal catamenial seizures can be attributed to the diminished progesterone level that occurs during inadequate luteal phase cycles.
Neurosteroids
Evidence shows that the antiseizure effects of progesterone are due to allopregnanolone, a metabolite of progesterone.[11],[13] Allopregnanolone is a member of a class of compounds known as "neurosteroids." Neurosteroids are steroids that are synthesized locally in the brain and have a strong and rapid effect on neural excitability.[14] Allopregnanolone is a potent, broad-spectrum anticonvulsant neurosteroid. It has been shown to protect against various forms of induced seizures. Recently it has been discovered that allopregnanolone is a potent positive modulator of GABAA receptors.[14],[15] GABA is the primary inhibitory neurotransmitter in the brain.[15] Allopregnanolone has specific, distinct binding sites on GABAA receptors that are separate from those for GABA, benzodiazepines, and barbiturates. [Figure 2] At normal physiological levels, it is sufficient to activate these receptors. This suggests that an abrupt "withdrawal" of allopregnanolone at the onset of menstruation could decrease the inhibitory effect and possibly exacerbate seizures.[16],[17]
Animal models
There is no specific animal model of catamenial epilepsy. Conventional models based on acute seizure induction are not suitable for testing therapies targeted at catamenial epilepsy. Animal models of catamenial epilepsy should be designed to simulate the menstrual cycle with its accompanying changes in seizure susceptibility. There are two categories of new models that partially represent catamenial epilepsy.[5] The first category simulates the rise and fall of estrogen and progesterone at the point in the cycle associated with increased seizure susceptibility,[18] that is, immediately before, and for the first few days of menstruation. Some examples of this model are pseudopregnancy, chronic progesterone treatment, and a progesterone withdrawal model. The second category is based on the naturally occurring estrous cycle or administration of exogenous hormones that simulate the specific stages of the estrous cycle in rats whose ovaries have been removed. There are also in vitro models that utilize cultured neurons that are exposed to steroid hormones to study the molecular mechanisms.
The pseudopregnancy model is based on the hypothesis that abrupt withdrawal of progesterone, and hence allopregnanolone, will cause increased seizure susceptibility. Our team has proposed a pseudopregnancy model where high levels of progesterone were induced over time, and then rapidly withdrawn by treating the animals with finasteride.[18],[19] Finasteride is a 5a-reductase inhibitor that blocks the reduction of progesterone to allopregnanolone. Acute withdrawal produced an increase in seizure susceptibility, whereas a long-term reduction in allopregnanolone levels did not. This is consistent with the pattern of catamenial epilepsy. A model must be validated by satisfying certain criteria. It must show close similarity to an epileptic-type state and should mirror the formation and effects of the disease in humans. The neurosteroid withdrawal model partially meets these criteria and is superior to conventional models for several reasons. It is based on the actual hormonal fluctuations of the menstrual cycle, it closely mimics the origin of catamenial epilepsy in humans, and it allows the study of how naturally occurring neurosteroids affect seizure susceptibility. The actual endocrine conditions may be different in models as compared to people, and because it is only an acute model, there is no provision for study of drug tolerance or other variables over a course of cycles.
Pharmacotherapy
The antiepileptic drugs commonly used in the treatment of seizure disorders are listed in [Table 1]. The conventional antiepileptic drugs are the mainstay for the management of catamenial seizures in women. Approximately one-third of women with epilepsy use more than one antiepileptic drug appropriate to their seizure type.
Traditional approach
Although there are many different drugs that are used in the treatment of epilepsy [Table 1], there is no specific treatment for catamenial epilepsy. This is partly because catamenial seizures are often refractory to conventional antiepileptic drugs such as valproate, phenytoin, and diazepam.[4],[5] Many of these drugs are prescribed for treatment of catamenial epilepsy without direct studies of effectiveness, with their use based primarily on empirical evidence. [Table 2] lists an overview of various drugs investigated for the treatment of catamenial epilepsy. Many patients received these agents as supplements or adjunct drugs in a continuous or intermittent approach for inhibition of catamenial seizures.[20],[21] Most of these drugs are limited severely in their use due to the development of tolerance (e.g., benzodiazepines) and/or are often associated with undesirable side effects such as sedation, depression, and reproductive toxicity. Hormonally based treatments, such as medroxyprogesterone acetate or natural progesterone, are frequently very effective [Table 2], but could cause undesirable hormonal and reproductive adverse effects.
Acetazolamide
Acetazolamide is the prototype of a class of agents that are potent inhibitors of carbonic anhydrase, a key enzyme involved in NaHCO<sub>3</sub> reabsorption and water balance in the kidney. Carbonic anhydrase is also present in the brain. Acetazolamide has been used empirically for years for the treatment of refractory epilepsy and catamenial seizures.[22],[23] Recently, the efficacy of acetazolamide was tested in 20 women with catamenial epilepsy.[24] Approximately 30% to 40% of subjects showed significant reduction in overall seizure frequency and severity. However, loss of efficacy (tolerance) is a problem reported by many women treated with acetazolamide.
Benzodiazepines
Benzodiazepines such as clonazepam and clobazam are positive allosteric modulators of GABAA receptor and broad-spectrum antiseizure agents. Clonazepam is highly useful in the therapy of absence and myclonic seizures, but was associated with tolerance to its antiseizure effects.[25] Clobazam has been found to be an effective agent for the treatment of catamenial epilepsy.[26], [27] Clobazam (20 to 30 mg/day) was administered intermittently from 2 to 4 days before menses probably to avoid the tolerance usually associated with continual therapy. The most common adverse effects of clobazam are sedation and depression. However, cross-tolerance to benzodiazepines have been described in animal model due to long-term exposure to neuroactive steroids.[28] which could affect the clinical utility of benzodiazepines in catamenial epilepsy.
Medroxyprogesterone acetate (MPA)
Medroxyprogesterone acetate is a widely investigated progestin-only contraceptive agent. MPA treatment in women with catamenial seizures found that it produces a 39% reduction in seizure frequency at a mean follow-up of 1 year.[21], [29] Suppression of seizures was evident when the patients were treated with parenteral MPA at dosages that were designed to halt regular menstrual cycle. Therefore, it is conceivable that long-term MPA therapy is associated with undesirable reproductive disturbances.
Natural progesterone
Cyclic natural progesterone use has been demonstrated as an effective treatment for catamenial and non-catamenial seizures in women.[20], [30], [31] Progesterone is efficiently absorbed after oral administration as lozenges, and rectal administration as suppositories. Progesterone was given at 100 to 200 mg, t.i.d. on days 15 to 28 of menstrual cycle. In a 3 month investigation of cyclic natural progesterone therapy, 23 of 25 (92%) women with intractable seizures completed the trial. Average monthly seizure frequency was reportedly reduced by 54% to 68% during the 3 month treatment period.[31] A 3 year follow-up report finds that 15 of the women continued on the same antiepileptic drug and progesterone protocol. These women continued to have a very substantial (62% to 74%) reduction in seizure frequency.[20] An NIH sponsored study is currently determining whether progesterone supplements can help reduce seizure frequency in women with epilepsy.[20] Although natural progesterone therapy benefits some women with catamenial epilepsy, it is associated with undesired hormonal side effects such as breakthrough bleeding, breast tenderness, and amenorrhea.
Experimental evidence from studies in animal models and clinical data is consistent with the possibility that the antiseizure effects of progesterone are due to its metabolic conversion to neurosteroids, principally allopregnanolone.[11],[32],[33],[34]. Therefore, synthetic GABAA receptor modulating neurosteroids, which are devoid of such hormonal actions, could provide a rational alternative approach to therapy.
Novel treatments
The neurosteroid withdrawal hypothesis presents the possibility for novel, and highly effective treatments. Using the catamenial epilepsy model, we evaluated the hypothesis that neurosteroid "replacement" is an effective and a rational therapy for catamenial epilepsy.[19], [35] During this seizure-prone state, the activity of conventional antiepileptic drugs, including diazepam and sodium valproate, is reduced, possibly accounting for the clinical impression that catamenial seizures are unusually drug resistant. Unexpectedly, neurosteroids that positively modulate GABAA receptors actually have enhanced anticonvulsant potency in the model, providing support for a neurosteroid "replacement" approach to the treatment of catamenial epilepsy.[19], [35] Overall, these observations suggest that neurosteroids represent a specific treatment approach for perimenstrual catamenial seizure exacerbations. It does suggest that cyclic replacement therapy would be highly effective. Here, the efficacy of neurosteroids in periovulatory and inadequate luteal phase seizures remain unclear. Unfortunately, natural neurosteroids are ineffective for perimenstrual treatment. They are orally inactive, have a very short (minutes) half-life, and have the potential to get converted to compounds that create undesirable hormonal effects. The synthetic version of allopregnanolone called ganaxolone is available.[36] Ganaxolone was designed to overcome the limitations of naturally occurring neurosteroids with significant improvements in pharmacokinetic and therapeutic properties.
Ganaxolone is a synthetic 3?-methyl analogue of allopregnanolone.[36] The 3?-methyl substituent minimizes metabolism at the 3a-hydroxyl group and so ganaxolone is orally active, is not converted to the hormonally active 3-keto form, and hence lacks hormonal side effects. Similar to allopregnanolone, ganaxolone is a potent positive allosteric modulator of GABAA receptors and a broad-spectrum anticonvulsant agent. The anticonvulsant potency of ganaxolone is enhanced in the period following neurosteroid withdrawal in a rat model of catamenial epilepsy, while the potencies of two reference anticonvulsants, diazepam and valproate are reduced.[19] Recently, a total of more than 500 people have received ganaxolone in several phase II clinical trials.[37] Safety and tolerability in the human experience have been impressive, except a dose-dependent sedation. In a preliminary study, ganaxolone was evaluated in women with catamenial epilepsy.[38] Patients received oral ganaxolone (300 mg/day, bid) starting on day 21 of the menstrual cycle and continuing through the third full day following the beginning of menstruation. During the 4 months of this ganaxolone "pulse" therapy, patients had a marked decrease in their catamenial seizures. Ganaxolone is still at development stage, but researchers hope that this agent may provide a specific treatment option for catamenial epilepsy.
Given the neurosteroid's critical role in catamenial seizures and ganaxolone's enhanced potency, the later may offer a rational approach for the treatment of perimenstrual catamenial epilepsy without producing hormonal side effects. Because of its unique modulatory profile, ganaxolone could be effective in cases where other GABAA receptor modulators fail to offer seizure protection because ganaxolone modulates most GABAA receptors with distinct subunits.[36]
Conclusion
There are approximately 50 million people with epilepsy worldwide, and approximately 40% of them are women. Women with catamenial epilepsy have seizures clustered around their monthly cycle. However, currently there is no specific treatment for this neuroendocrine condition. The cause of catamenial epilepsy is unknown, but it must be uncovered in order to develop prevention and treatment techniques. The altered balance of estrogens, progesterone, and neurosteroids seem to play a clear role in increased seizure susceptibility. Several antiepileptic drugs are used in catamenial epilepsy therapy. However, catamenial seizures are not successfully treated currently with these conventional antiepileptic drugs. The drugs used to control epilepsy may also affect a woman's hormones. There is little information to whether catamenial seizures in humans really represent an epileptogenic process or are merely an exacerbation of existing seizure disorder. It is suggested that because of repeated triggers due to withdrawal cycles, some women might develop epileptogenicity resulting in catamenial epilepsy, while catamenial seizure exacerbation could be ascribed to neurosteroid withdrawal in preexisting epileptic condition. However, there is no validated model to prove this hypothesis on the development of catamenial seizures. Much has been learned about this disease, but there is much more that is yet to be learned.
References
1. Bharucha NE. Epidemiology of epilepsy in India. Epilepsia 2003;44:9-11.
2. Gourie-Devi M, Gururaj G, Satishchandra P, Subbakrishna DK. Prevalence of neurological disorders in Bangalore, India: A community-based study with a comparison between urban and rural Areas. Neuroepidemiology 2004,23:261-8.
3. Herzog AG, Klein P, Ransil BJ. Three patterns of catamenial epilepsy. Epilepsia 1997;38:1082-8.
4. Foldvary-Schaefer N, Falcone T. Catamenial epilepsy: pathophysiology, diagnosis, and management. Neurology 2003;61:2-15.
5. Reddy DS. Pharmacology of catamenial epilepsy. Meth Find Exp Clin Pharmacol 2004;26:547-61.
6. Rogawski MA and Loescher W. The neurobiology of antiepileptic drugs. Nature Neurosc Rev 2004;5:553-64.
7. Isojarvi JI, Tauboll E, Herzog AG. Effect of antiepileptic drugs on reproductive endocrine function in individuals with epilepsy. CNS Drugs 2005;19:207-23.
8. Buterbaugh GG. Estradiol replacement facilitates the acquisition of seizures kindled from the anterior neocortex in female rats. Epilepsy Res 1989;4:207-15.
9. Bonuccelli U, Melis GB, Paoletti AM, Fioretti P, Murri L, Muratorio A. Unbalanced progesterone and estradiol secretion in catamenial epilepsy. Epilepsy Res 1989;3:100-6.
10. Logothetis J, Harner R, Morrel F. The role of estrogens in catamenial exacerbation of epilepsy. Neurology 1959;9:352-60.
11. Reddy DS, Castenada DA, O'Malley BW, Rogawski MA. Anticonvulsant activity of progesterone and neurosteroids in progesterone receptor knockout mice. J Pharmacol Exp Ther 2004;310:230-9.
12. Lonsdale D, Burnham WM. The anticonvulsant effects of progesterone and 5a-dihydroprogesterone on amygdala-kindled seizures in rats. Epilepsia 2003;44:1494-9.
13. Wang M, Seippel L, Purdy RH, B?ckstr ?m T. Relationship between symptom severity and steroid variation in women with premenstrual syndrome: Study on serum pregnenolone, pregnenolone sulfate, 5a-pregnane-3,20-dione and 3a-hydroxy-5a-pregnan-20-one. J Clin Endocrinol Metab 1996;81:1076-82.
14. Reddy DS. Pharmacology of endogenous neuroactive steroids. Crit Rev Neurobiol 2003;15:197-234.
15. Lambert JJ, Belelli D, Peden DR, Vardy AW, Peters JA. Neurosteroid modulation of GABAA receptors. Prog Neurobiol 2003;71:67-80.
16. Smith SS, Gong QH, Hsu FC, Markowitz RS, ffrench-Mullen JMH, Li X. GABAA receptor a4-subunit suppression prevents withdrawal properties of an endogenous steroid. Nature 1998;392:926-30.
17. Laidlaw J. Catamenial epilepsy. Lancet 1956;271:1235-7.
18. Reddy DS, Kim HY, Rogawski MA. Neurosteroid withdrawal model of perimenstrual catamenial epilepsy. Epilepsia 2001;42:328-36.
19. Reddy DS, Rogawski MA. Enhanced anticonvulsant activity of ganaxolone after neurosteroid withdrawal in a rat model of catamenial epilepsy. J Pharmacol Exp Ther 2000;294:909-15.
20. Herzog AG. Progesterone therapy in women with epilepsy: A 3-year follow-up. Neurology 1999;52:1917-8.
21. Zimmerman AW, Holden KR, Reiter EO, Dekaban AS. Medroxyprogesterone acetate in the treatment of seizures associated with menstruation. J Pediatr 1973;83:959-63.
22. Ansell B, Clarke E. Acetazolamide in treatment of epilepsy. Br Med J 1956;1: 650-61.
23. Ross IP. Acetazolamide therapy in epilepsy. Lancet 1958;2:1308-9.
24. Lim LL, Foldvary N, Mascha E, Lee J. Acetazolamide in women with catamenial epilepsy. Epilepsia 2001;42:746-9.
25. Haigh JR, Feely M. Tolerance to the anticonvulsant effect of benzodiazepines. Trends Pharmacol Sci 1988;9:361-6.
26. Feely M, Calvert R, Gibson J. Clobazam in catamenial epilepsy: A model for evaluating anticonvulsants. Lancet 1982;2:71-3.
27. Feely M, Gibson J. Intermittent clobazam for catamenial epilepsy: tolerance avoided. J Neurol Neursurg Psychiatry 1984;47:1279-82.
28. Reddy DS, Rogawski MA. Chronic treatment with the neuroactive steroid ganaxolone in the rat induces anticonvulsant tolerance to diazepam but not to itself. J Pharmacol Exp Ther 2000;295:1241-8.
29. Mattson RH, Cramer JA, Caldwell BV, Siconolfi BC. Treatment of seizures with medroxyprogesterone acetate: preliminary report. Neurology 1984;34:1255-8.
30. Herzog AG. Intermittent progesterone therapy and frequency of complex partial seizures in women with menstrual disorders. Neurology 1986;36:1607-10.
31. Herzog AG. Progesterone therapy in women with complex partial and secondary generalized seizures. Neurology 1995;45:1660-2.
32. Kokate TG, Banks MK, Magee T, Yamaguchi S, Rogawski MA. Finasteride, a 5a-reductase inhibitor, blocks the anticonvulsant activity of progesterone in mice. J Pharmacol Exp Ther 1999;288:679-84.
33. Frye CA, Rhodes ME, Walf A, Harney J. Progesterone reduces pentylenetetrazol-induced ictal activity of wild-type mice but not those deficient in type I 5a-reductase. Epilepsia 2002;43:14-7.
34. Herzog AG, Frye CA. Seizure exacerbation associated with inhibition of progesterone metabolism. Ann Neurol 2003;53:390-1.
35. Reddy DS, Rogawski MA. Enhanced anticonvulsant activity of neuroactive steroids in a rat model of catamenial epilepsy. Epilepsia 2001;337-44.
36. Reddy DS, Woodward R. Ganaxolone: A prospective overview. Drugs Future 2004;29:227-42.
37. Monaghan EP, Navalta LA, Shum L, Ashbrook DW, Lee DA. Initial human experience with ganaxolone, a neuroactive steroid with antiepileptic activity. Epilepsia 1997;38:1026-31.
38. McAuley JW, Moore JL, Reeves AL, Flyak J, Monaghan EP, Data J. A pilot study of the neurosteroid ganaxolone in catamenial epilepsy: Clinical experience in two patients. Epilepsia 2001;42:85.
COPYRIGHT 2005 Medknow Publications
COPYRIGHT 2005 Gale Group