* Background.-Cardiovascular toxicity of chemotherapy for testicular cancer is a matter of discussion, since highly efficient agents can achieve cure of the disease, even in the metastasized setting. Acute ischemic events during the treatment period and a persistently elevated serum cholesterol thereafter are observations of particular concern in these patients, and the underlying basic mechanisms are unknown to date.
Objective.-To evaluate etoposide, which is part of the standard treatment for testicular cancer, as a potential cause of atherogenesis in an experimental model.
Setting-Aortic ^sup 125^I-labeled low-density lipoprotein retention was studied in 72 cholesterol-fed rabbits under etoposide treatment and was quantified according to the morphologically assessed type of surface lining. Aortic cholesterol content was determined both by Sudan III staining and quantitatively by a biochemical assay.
Results.-A reduced uptake of ^sup 125^I-labeled low-density lipoprotein in the arterial wall was observed in the etoposide-treated animals, which resulted in a size reduction of sudanophilic areas and cholesterol content. Whereas the breakdown of ^sup 125^I-labeled low-density lipoprotein in the liver was not significantly enhanced, the plasma decay of ^sup 125^I-labeled low-density lipoprotein was faster and serum cholesterol was lower in the etoposide group than in controls.
Conclusion.-Unexpectedly, we found an improvement of arterial wall lipid metabolism under etoposide treatment and can thus exclude this substance as a promoter of atherogenesis in this model.
(Arch Pathol Lab Med. 1999;123:514-518)
To date, cisplatin-containing polychemotherapy is able to cure most patients with testicular cancer, even those with advanced disease.1 Having achieved this therapeutic goal, there is now room for concern over the side effects of this treatment, particularly regarding the fact that patients whose tumors are confined to the testis at the time of diagnosis are treated in an adjuvant setting to reduce the risk of a relapse, which has no influence on overall survival.2
Cardiovascular toxicity during and in the first weeks after treatment has been reported in testicular cancer patients treated with various polychemotherapeutic regimens.3,4 Since Raynaud's phenomenon is a well-described finding in these patients,5 spasms of the coronary arteries due to endothelial damage by bleomycin6 or hypomagnesemia induced by cisplatin7,8 seem to be the most likely causes.
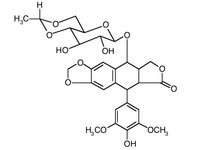
Several anecdotial reports of early-onset coronary artery disease9-11 can be found in the literature, and widespread concern about this issue exists. A strong correlation between the serum cholesterol level measured early in adult life in men and the incidence of cardiovascular disease in midlife has been reported.12 A persistent increase in serum cholesterol levels after therapy in 14 out of 17 patients treated and cured with BEP (bleomycin, etoposide, asplatin) has been observed.13 Although the sustained increase in serum cholesterol levels in some of the patients was confined to the normal range, 7 (41%) of 17 patients had higher than desirable levels of total serum and low-- density lipoprotein (LDL) cholesterol. However, no increased risk of coronary artery disease could be found in several cohorts of patients analyzed in long-term followup.14,15 Etoposide, an epipodophyllotoxin, which is the second most active single agent in germ cell cancer,16 was added as the last drug to this schedule and was therefore, in our opinion, the most likely candidate to raise serum cholesterol without resulting in an increase of cardiovascular events in the retrospective analysis.
Lipid, and in particular arterial wall lipid metabolism, is of key importance in atherogenesis.17 One of the first steps during atherogenesis is enhanced LDL entry into the arterial wall,18 finally resulting in enhanced cholesterol ester accumulation, predominantly intracellularly. Based on the limited knowledge of the interactions of etoposide with the lipid metabolism, we investigate the influences of etoposide on arterial LDL entry, as well as the extent of lipid lesions and cholesterol ester accumulation.
MATERIALS AND METHODS
Experimental Studies
The abdominal aortic endothelium of 6-month-old male New Zealand white rabbits (n = 72) was abraded by a Fogarty catheter. All animals were then fed for 4 weeks with a commercial laboratory chow and water ad libitum. The diet was supplemented with 1% cholesterol. During this 4-week period, 36 rabbits were receiving etoposide (3 mg/kg/day; Vepesid, Bristol, Troisdorf, Germany), while the other 36 rabbits served as controls receiving placebo. Growth and body weight were similar in the 2 groups. After the period of cholesterol-supplemented diet, all 72 animals were injected with 10 (mu)Ci (3.7 x 10^sup 5^ Bq) ^sup 125^I-LDL into the ear vein. Six animals of each group were killed with a blow to their neck at times 1, 3, 6, 12, 24, and 48 hours after injection. Isolation of LDL by Immunoaffinity Chromatography
Blood was drawn from overnight fasting normolipemic volunteers and anticoagulated 1:10 with 3.8% sodium citrate. Polyclonal anti-apo-B antibodies were obtained by immunizing sheep with LDL. Gamma globulins were precipitated from sheep plasma with ammonium sulphate (390 g/L, Sanabo, Vienna, Austria) to a final concentration of 35% and further purified by immunoaffinity chromatography. For this purpose, 3 g of pure LDL were coupled with 400 mL of 0.5 mol/L BrCN-activated Sepharose Cl 4B (Pharmacia, Uppsala, Sweden) according to methods described by Axen et al.19 The immunopurified antibodies were themselves coupled with BrCN-activated sepharose Cl 4B, and this support was used to isolate apo-B-containing lipoproteins (LDL, very low-density lipoprotein) from volunteers plasma: 10 mL of anti-LDL-sepharose Cl 4B gel was poured into a glass column (22 x 2 cm). The gel was extensively washed with 500 mL of isotonic NaCI solution. Ten milliliters of volunteers citrated plasma were recirculated for 30 minutes over the column at a flow rate of 10 mL/ min. The column was then washed with isotonic saline solution until it was free of protein (E 260/280 nm
Radiolabeling of Purified LDL
A final concentration of 10 mg LDL/mL was used for radiolabeling with ^sup 125^I- by the iodine monochloride technique described by McFarlane20 as modified for lipoproteins.2 Briefly, an ICI stock solution (34 (mu)mol / mL 6 mol / L HCI) was purified before labeling by 3 extractions with CHCl3 and diluted 1:100 with aqueous 2 mol/L NaCl. Approximately 1 mg purified lipoproteins (100 (mu)L); 200 (mu)L 1 mol/L glycine buffer, pH 10; about 1 mCi (3.7 x 10^sup 7^ Bq) [^sup 125^I]NaI/10 (mu)L (IRE, Floris, Belgium, in 0.01 mol/L NaOH, >100 mCi [3.7 x 10^sup 9^ Bq]/mL,
Recovery and Decay of Radiolabeled LDL In Vivo
Determination of recovery was performed in vitro by isolation with ultracentrifugation of the single lipoprotein fractions at 10 time intervals (1, 2, 4, 6, 8, 10, 12, 16, 20, and 24 hours) after ^sup 125^ILDL injection and radioactive counting (Packard Instrument Company, Downers Grove, Ill) of each single fraction.
Biodistribution of Radioactivity
After sacrificing the animals, samples of the following tissues were obtained: liver, spleen, gallbladder, heart, lung, thyroid gland, stomach, small bowel, kidney, muscle, adrenal gland, rib, aortic arch, thoracic aorta, and abdominal aorta. The tissues were washed 3 times in cold phosphate-buffered saline at 4 deg C, then blotted dry, weighed, and evaluated for radioactivity in a Packard counter. The results were expressed as percentage of injected dose per gram of tissue (% ID/g of tissue) for the different organs. All the organ counts were corrected for physical decay.
Evaluation of LDL Entry Into the Abdominal Aorta
The abdominal aorta was removed, segments were fixed in 3.5% phosphate-buffered glutaraldehyde (pH 7.4), and histologic sections were used to verify the presence of normal intact endothelial lining, re-endothelialization, or de-endothelialization. Vascular segments were punched out of each of the 3 different lesions, and the radioactivity reflecting the LDL uptake was counted with a gamma counter.
Sudan III staining and a morphological control were also performed. The percentage of surface stained was assessed using photography and planimetry.
Vascular Cholesterol Content
The carefully excised vascular specimens were incubated at 37 deg C for 3 minutes in tris-HCl buffer (300 (mu)L, pH 7.4). The segments were then rinsed in ice-cold tris-HCI buffer. The cholesterol content of the aortic samples was determined after extraction according to the methods described by Folch et at.22^sup ^3H-Cholesterol standard was used to control the efficiency of lipid extraction. A photometric method to estimate cholesterol (CHOD-PAP method; Boehringer, Mannheim, Germany) was applied. The estimation of the protein was performed using the Lowry method.23
Serum Cholesterol
Serum cholesterol was measured by means of enzymatic method (Boehringer).
Prostacyclin Formation
Vascular tissue was incubated in 300 WL of tris-HCl buffer (pH 7.4) at 22 deg C. Prostacyclin formation was assessed by the platelet aggregation inhibition bioassay24 modified according to Sinzinger et al.25 Using human blood anticoagulated with 3.8% sodium citrate, a platelet-rich plasma was prepared by centrifugation (150g, 10 minutes, 22 deg C). Thereafter, platelet-rich plasma was adjusted with platelet-poor plasma to a final platelet count of 250 x 10^sup 3^/ (mu)L. The aggregation induction was done with 1 Fmol/L adenosine diphosphate (Boehringer) in 600 (mu)L platelet-rich plasma samples under constant stirring at 22 deg C in a Born-type aggregometer.26 The inhibition of adenosine diphosphate-induced aggregation was quantified by means of a synthetic PGI^sub 2^ standard (The Upjohn Company, Kalamazoo, Mich). PGI^sub 2^ formation was also controlled by 6-oxo-PGF, formation, its stable derivative, measured by a specific radioimmunoassay (Amersham International, Buckinghamshire, United Kingdom).
Statistical Evaluation
Values are presented as the mean +/- standard deviation. Calculation for significance was performed by an unpaired t test combined with a nonparametric analysis of variance by the Wilcoxon test. Values were considered significant at P
RESULTS
Determination of the recovery showed quite stable LDL binding (Figure 1). Measurement of radioactivity within the arterial wall therefore truly reflected LDL uptake. Over time, there was a slight shift of radioactivity from the LDL to the high-density lipoprotein fraction, showing the physiological transference from LDL to high-density lipoprotein. No significant difference concerning a higher rate of this process (Figure 1) was found in the animals receiving etoposide. Plasma decay of ^sup 125^I-LDL (Figure 2) was faster than in controls, becoming significant (P
As a morphologic confirmation of these findings, the percentage of vascular surface that stained positively with Sudan III (Table 2) was significantly (P
Serum cholesterol in the treated group was significantly lower than in the control group (1261.7 +/- 63.8 mg/dL vs 1756 +/- 70.3 mg/dL). No difference was found in serum high-density lipoprotein levels (30.3 +/- 0.9 mg/ dL vs 31.2
0.6 mg/dL). PGI^sub 2^ formation, as well as that of its radioimmunologically determined stable derivative 6-oxoPGF^sub 1^6-oxo-PGF^sub a^, was generally increased in the animals receiving etoposide (Table 3), a trend which was highest in the endothelialized areas.
To summarize, there was a reduced uptake of LDL in the arterial wall in the animals receiving etoposide and consequently a reduction in the size of experimentally induced fatty streaks, as shown in sudanophilic areas. Breakdown of LDL in the liver was not significantly enhanced. Plasma decay of ^sup 125^I-LDL was faster and serum cholesterol was lower than in the controls. Both a significantly enhanced formation of PGI^sub 2^ and a trend toward an increase in high-density lipoprotein under etoposide administration were observed.
COMMENT
Since the introduction of cisplatin in chemotherapy regimens in the 1970s, a high proportion of testicular cancer patients with advanced disease have achieved long-lasting, complete remissions, and most are even cured by chemotherapy.1 Compared with the combined modality treatment for Hodgkin's disease, the only malignant solid tumor with comparable cure rates, the threat of secondary malignancies in these long-term testicular cancer survivors is vanishing and is limited to rare acute leukemias secondary to etoposide27 and radiation therapy.28 More concern is raised by reports in the literature about the vascular toxicity of chemotherapy, ranging from Raynaud's phenomen5 to myocardial infarction.3,4 Acute cardiovascular events are more likely related to vasospasms based on cisplatin-induced hypomagnesemia7,8 or bleomycin-induced endothelial damage6 than to atherosclerotic origin. Retrospective studies did not discover a higher incidence of cardiovascular events compared with a control population.14,27 However, elevated serum cholesterol levels have been found in patients with testicular cancer after chemotherapy,13 and this finding has raised new concerns. Furthermore, the late vascular toxicity of germ cell therapy is likely to be subtle, and even careful epidemiologic studies will have problems excluding a negative effect of the chemotherapeutic agents. To our knowledge, no experimental studies on the influence of these chemotherapeutic drugs on lipid mechanism exist so far.
Because of its quite unexpected beneficial influence on LDL entry into the arterial wall (one of the key events of atherogenesis), etoposide can be ruled out as a causative agent for a negative influence on lipid metabolism and consequent development of coronary artery disease. As a consequence, we noted a reduction in the size of experimentally induced atheromatous plaques. The pathogenesis of this effect is not clear. Etoposide induces leukopenia and could therefore result in damage to the monocyte/ macrophage system, inhibiting the adhesion and migration of monocytes or macrophages and resulting in a deprivation of tissue macrophages and consecutively in a smaller uptake of modified LDL by scavenger receptors.29 However, plasma decay of LDL was significantly faster in the animals receiving etoposide, and a higher uptake of radiolabeled LDL was found in the liver, although not at a significant level. This could be induced by an upregulation of LDL receptors in the liver, resulting in a higher breakdown of LDL to high-density lipoprotein. At least part of the reduced LDL uptake seems to be mediated by an increase of PG^sub 2^ in the arterial wall.
More important than the mechanisms already noted is the fact that etoposide can be excluded as a drug which harms the arterial wall and leads to atherogenesis in this experimental model. The elevated serum cholesterol levels observed in patients with testicular cancer could be mediated by the reduction of tumor burden, since tumors do express LDL receptors and show a high rate of LDL uptake. A number of tumor cell lines and tumor tissues present higher LDL-receptor activities than normal cells, and there is evidence from studies in leukemic patients that hypocholesterolemia in malignancy due to elevated LDL-- receptor activity in tumor cells may occur.30 As the majority of our patients had pretreatment cholesterol levels that were lower than their posttherapeutic level, this assumption is unlikely to be the cause. However, 2 other drugs, cisplatin and bleomycin, which are under study at the moment, or the combination of any of these drugs, could be responsible for the raise in cholesterol levels and supposed vascular damage.
References
1. Einhorn LH. Testicular cancer as a model for a curable neoplasm: the Richard and Hinda Rosenthal Foundation Award Lecture. Cancer Res. 1981;41: 3275-3280.
2. Peckham MJ, Barrett A, Husband JE, Hendry WF. Orchidectomy alone in testicular stage I nonseminomatous germ cell tumors. Lancet. 1982;2:678-680.
3. Doll DC, List AF, Grecco A, Hairsworth JD, Handle KR, Johnson DFI. Acute vascular ischemic events after cisplatin-based combination chemotherapy for germ cell tumors of the testis. Ann Intern Med. 1986;78:861-869.
4. Samuels BL, Vogelzang NJ, Kennedy BI. Severe vascular toxicity associated with vinblastine, bleomycin and cisplatin chemotherapy. Cancer Chemother PharmacoL 1987;19:253-256.
5. Vogelzang NJ, Bosl GJ, Johnson K, Kennedy BI. Raynaud's phenomenon: a common toxicity after combination therapy for testicular cancer. Ann Int Med. 1981;95:288-292.
6. Burkhardt A, Haltje WJ, Gebbens JO. Vascular lesions following perfusion with bleomycin: electron microscopic observations. Virchows Arch. 1976;372: 227-236.
7. Schilsky RL, Anderson T. Hypomagnesemia and renal magnesium wasting in patients receiving cisplatin. Ann Intern Med. 1979;90:929-931.
8. Turlapaty PD, Altura BM. Magnesium deficiency produces spasms of the coronary arteries: relationship to etiology of sudden death in ischemic heart disease. Science. 1980;208:198-200.
9. Bodensteiner DC. Fatal coronary fibrosis after treatment with bleomycin, vinblastin and cisplatinum. South Med J. 1981;74:898-899.
10. Edwards GS, Lane M, Smith FE. Long-term treatment with cisdichloro-dia
mineplatinum (il)-vinblastine-bleomycin: possible association with severe coronary disease. Cancer Treat Rev. 1979;63:551 552.
11. Vogelzang NJ, Frenning DH, Kennedy BJ. Coronary artery disease after bleomycin and vinblastin. Cancer Treat Rev. 1980;64:1159-1160.
12. Klag MJ, Ford DE, Mead LA. Serum cholesterol in young men and subsequent cardiovascular disease. N Engl J Med. 1993;328:313-318.
13. Rhagavan D, Cox K, Childs A, Grygiel J, Sullivan D. Hypercholesterolemia after chemotherapy for testis cancer. J Clin Oncol. 1992;10:1386-1389.
14. Boyer M, Raghavan D, Harris PI, et al. Lack of late toxicity in patients treated with cisplatin containing combination chemotherapy for metastatic testicular cancer. I Clin Oncol. 1990;8:21-26.
15. Nichols C, Roth B, Williams S. Cardiovascular complications of chemotherapy for testicular cancer. Proc Am Soc Oncol. 1990;9:132-140.
16. Fitzharris BM. VP 16-213 as a single agent in advanced testicular tumours. Eur J Cancer. 1980;17:245-249.
17. Newman HAI, Zilversmit DB. Quantitative aspects of cholesterol flux in rabbit atheromatous lesions. J Biol Chem. 1962;237:2078-2085.
18. St. Clair RW. Metabolism of the arterial wall and atherosclerosis. In: Paoletti R, Gotto AM, eds. Atherosclerosis Review New York, NY: Raven Press; 1976:61-117.
19. Axen R, Porath J, Ernbhack S. Chemical coupling of peptides and proteins to polysaccharides by means of cyanogen halides. Nature.1967;214:1302-1305.
20. McFarlane AS. Efficient radiolabelling of proteins with iodine. Nature. 1958;182:53-55.
21. Langer T, Stober W, Levy R. The metabolism of low density lipoproteins in familial type II hyperlipoproteinemia. J Clin Invest. 1972;51:1528-1536.
22. Folch J, Lees M, Stanley HS. A simple method for the isolation and purification of total lipids from animal tissues. Biol Chem. 1957;226:497-509.
23. Lowry OH, Rosebrough NJ, Farr AL, Randall RJ. Protein measurements with the Folin phenol reagent. J Biol Chem. 1951;193:265-275.
24. Moncada S, Gryglewski JR, Bunting S, Vane JR. An enzyme isolated from arteries transforms prostaglandin endoperoxides to an unstable substance that inhibits platelet aggregation. Nature. 1976;263:663-665.
25. Sinzinger H, Firbas W, Cromwell M. Radiation induced alterations in rabbit aortic prostacyclin formation. Prostaglandins.1982;24:323-329.
26. Born GVR, Cross MJ. The aggregation of blood platelets. I Physiol. 1963;168:178-195.
27. Nichols CR, Breeden ES, Loehrer PJ, Williams SD, Einhorn LH. Secondary leukemia associated with a conventional dose of etoposide: review of serial germ cell tumor protocols. I Natl Cancer Inst. 1993;85:36-40.
28. Van Leeuwen FE, Stiggel Bout AM, Van Den Bely D, et al. Second cancer risk following testicular cancer: a follow-up study of 1909 patients. J Clin Oncol. 1993;11:415-424.
29. Goldstein JL, Ho YK, Basu SK, Brown MS. Binding site on macrophages that mediates uptake and degradation of acetylated low density lipoprotein, producing massive cholesterol deposition. Proc Natl Acad Sci U SA. 1979;76:333337.
30. Vitols S, Garthon G, Bjor Kholm M, Petterson C. Hypocholesterolemia in malignancy due to elevated LDL receptor activity in tumor cells: evidence from studies in leukemic patients. Lancet. 1985;2:1150-1154.
Accepted for publication January 18, 1999.
From the Department of Internal Medicine, Division of Oncology (Drs Krainer and Zielinski), the Department of Nuclear Medicine (Drs Rodrigues and Sinzinger), and Ludwig Boltzmann Institute for Nuclear Medicine (Dr Sinzinger), University Hospital, Vienna, Austria.
Reprints: Margarida Rodrigues, Department of Nuclear Medicine, University Hospital, Wahringer Gurtel 18-20, A-1090 Vienna, Austria.
Copyright College of American Pathologists Jun 1999
Provided by ProQuest Information and Learning Company. All rights Reserved