Objective: To determine the applicability and safety of an ifosfamide, cisplatin, and etoposide (VIP) regimen as a neoadjuvant chemotherapy to a concomitant thoracic radiotherapy and cisplatin continuous infusion in locally advanced non-small cell lung cancer (NSCLC).
Patients and methods: Forty-four patients (stage IIIb in 43 and stage IIIa in 1) entered a study of VIP, followed by concomitant thoracic radiotherapy and cisplatin continuous infusion. Chemotherapy consisted of three courses of cisplatin 25 mg/[m.sup.2], ifosfamide 1.5 g/[m.sup.2] (with uroprotection), and etoposide 100 mg/[m.sup.2] given on days 1 to 4 of a 21-day cycle with hematopoictic support using recombinant human methionyl granulocyte colony stimulating factor. Patients who achieved a response or a stabilization were planned to receive a split-course normofractionated thoracic radiotherapy (first course: 30 Gy/10; 4-week rest period; second course: 25 Gy/10). A continuous cisplatin infusion of 6 mg/[m.sup.2] daily was administered using an autonomous chemotherapy delivery device. Total plasma platinum titration was performed daffy during the two courses in five of the patients. Analyses were done on an intent-to-treat basis.
Results: Thirty-nine of the 44 patients received the three-cycle chemotherapy program. Received dose intensity was 82%. Thirty-eight patients received the radiotherapy and, among them, 35 received the complete concomitant continuous cisplatin infusion. Objective (complete) response rates were 48% (7%) at the end of chemotherapy and increased up to 61% (16%) by the end of radiotherapy. At the end of the first radiotherapy cycle, the mean total plasma platinum concentration was twice as high as that of the residual postinduction chemotherapy concentration. During induction chemotherapy, myelosuppression was the limiting toxicity requiring hospital readmission in 23 patients. During radiotherapy, the main toxicity was acute esophagitis. A relatively high rate of pulmonary fibrosis was observed using the subjective objective management analytic--late effects of normal tissue score without life-threatening pulmonary function impairment. None of the patients died from toxic reactions. Probability of survival at 1, 2, and 3 years was 49%, 19%, and 5%, respectively. Primary cause of failure was a local relapse in 63% of the patients, brain metastases in 24%, and hematogeneous metastases to other sites in 13%.
Conclusion: Neoadjuvant VIP followed by concomitant radiotherapy-chemotherapy is feasible, but the split-course radiotherapy did not prevent a high rate of local recurrences. The high rate of toxic reactions requiring hospital readmission limits further development of such an aggressive regimen in NSCLC. (CHEST 1999; 115:144-150)
Key words: concomitant radiochemotherapy; continuous cisplatin infusion; induction chemotherapy; non-small cell lung cancer
Abbreviations: CAP = cisplatin, doxorubicin (Adriamycin), cyclophosphamide; CI = confidence interval; MVP = mitomycin C, vinblastine or vindesine, cisplatin; NSCLC = non-small cell lung cancer; r-metHuG-CSF = recombinant human methionyl granulocyte colony stimulating factor; SOMA-LENT = subjective objective management analytic--late effects of normal tissues; VIP = cisplatin, etoposide, ifosfamide combination., WHO = World Health Organization
Patients with non-small cell lung cancer (NSCLC) at stage IIIb of Mountain's classification are generally not considered for surgery. Radical radiotherapy has long been proposed as the sole therapy, and it is mainly used in an attempt to limit symptoms related to locally advanced NSCLC.[1] The main underlying problem is that the local and regional extension in NSCLC makes the existence of a microscopic metastatic disease predictable. This is the explanation for the frequent metastatic relapses following radiotherapy alone in stage IIIb NSCLC. This clinical observation is the rationale for the evaluation of the case of chemotherapy in the treatment of this disease. Several randomized studies comparing radiotherapy vs radiotherapy and chemotherapy have reported a survival advantage for patients assigned to the combined modality treatment. However, some other studies failed to demonstrate such an advantage. A recent meta-analysis confirms the putative role of chemotherapy in this setting and highlights the pivotal case of cisplatin.[2] However, the above-mentioned survival advantage remains extremely weak as only a 10% reduction in the risk of death is offered to patients receiving chemotherapy corresponding to an absolute benefit of 3% at 2 years, Search for new combinations and schedules of chemotherapy is therefore needed.
Among the different schedules of radiotherapy-chemotherapy association, one can consider the case of induction chemotherapy as it has been investigated in marginally resectable NSCLC.[3,4] For this modality, the early delivery of systemic chemotherapy could efficiently treat the microscopic metastatic disease. Afterwards, a local treatment (radiotherapy in our setting) might eradicate the chemoresistant tumor remainder.
A second possible schedule of radio-chemotherapy combination is the concomitant delivery of the two modalities. The chemotherapy dosage used in this setting is usually low in order to circumvent the putative increase in toxic effects. Cisplatin given at a 6 mg/[m.sup.2] daily dosage allows a radiosensitization of the disease and increases the survival by reducing the local recurrence rate.[5] The timing of chemotherapy delivery in relation to each radiotherapy fraction remains to be established. As DNA repair following radiotherapy occurs as a continuous process, a continuous infusion of cisplatin might be proposed.
We recently published the feasability of recombinant human methionyl granulocyte colony stimulating factor (r-metHuG-CSF) as an adjunct to etoposide, ifosfamide, cisplatin (VIP) regimen in 20 patients with locally advanced or metastatic NSCLC.[6] In the present study, we investigated the applicability and safety of this regimen as a neoadjuvant chemotherapy to a concomitant thoracic radiotherapy and cisplatin continuous infusion.
MATERIALS AND METHODS
Patients
Patients with newly diagnosed, histologically proven NSCLC took part in this open nonrandomized bicentric, phase II study. Staging procedure was done according to the fourth edition of the International Union Against Cancer, tumor-nod-metastases staging classification,[8] the American Thoracic map of regional lymph nodes? and the Mountain's stage grouping (the 1986 edition was in use at time when this study began but as the new classification does not alter the IIIb subgroup; the 1997 stage-grouping is therefore applicable to this study).[9] Staging procedure consisted of CT scan of the chest, upper abdomen, and brain, fiberoptic bronchoscopy, and bone nuclear scanning; cervical mediastinoscopy was not done routinely but only for patients with no evidence of bulky mediastinal lesions on CT. Eligibility consisted of age [is less than] 75 years old, performance status [is less than] 3 (Eastern Cooperative Oncology Group), stage IIIb, normal baseline neutrophils and platelets, normal hepatic and renal functions, and measurable disease. Patients who had received previous treatment, patients suffering from active infection, and patients who had had a previous malignant disease were excluded from the study.
Chemotherapy
Induction chemotherapy consisted of daily administration of the following treatment: etoposide, 100 mg/[m.sup.2] in a 30-min IV infusion; cisplatin, 25 mg/[m.sup.2] in a 100-min IV infusion; ifosfamide, 1.5 g/[m.sup.2] in a 180-min IV infusion; and mesna, 1.8 g/[m.sup.2] in a 14-h IV infusion. Patients were hospitalized during the chemotherapy delivery. This treatment was associated with hyperhydratation and was repeated days 1 to 4. Selective serotonin receptor antagonists were given as a prophylaxis of chemotherapy-induced emesis, r-metHuG-CSF (Filgrastim; Amgen Inc; Thousand Oaks, CA), 5 [micro]g/kg, was administered subcutaneously from day 5 to day 14. This adjuvant therapy was discontinued before clay 14 if the absolute neutrophil count was [is greater than] 5,000/[micro]L. A cycle was scheduled every 21 days and a total of three cycles was planned as induction therapy.
Chemotherapy toxicity was assessed for each cycle according to the World Health Organization (WHO) scale.[10] Hematologic status of the patients was screened every other day once the patient entered the nadir period. A 25% dose reduction was applied for patients who experienced a grade 3 thrombocytopenia or a grade 3 neutropenia lasting longer than 7 days or a febrile neutropenia during the preceding cycle. In addition, when the blood count on day 1 of a planned cycle indicated neutropenia and/or thrombocytopenia, the course was delayed for 8 days. Full projected doses of cisplatin were administered to patients with a creatinine clearance [is greater than] 60 mL/min. Patients with creatinine clearance between 40 and 60 mL/min received 50% of the projected doses, whereas no cisplatin was administered to patients with a [is less than] 40 mL/min creatinine clearance.
Radiotherapy
After a 3-week rest period following the third chemotherapy cycle, patients who achieved a response and those with stable disease received a split-course normofractionated thoracic radiotherapy using megavoltage equipment. During the first course, a dose of 30 Gy was delivered in 10 fractions. Following a 4-week rest period, radiation therapy was restarted for 2 weeks, 9,5 Gy in 10 fractions. CT scan dosimetry was used for each patient. During the first course, radiation was given to the primary tumor with a 1- to 2-cm normal lung margin, the ipsilateral and contralateral hilar, mediastinal, and supraclavicular lymph nodes, subcarinal node, by anterior and posterior fields. The second course was administered using lateral or oblique fields excluding the spinal cord and the normal lung. Cisplatin was concomitantly delivered during both radiotherapy courses. A continuous infusion of 6 mg/[m.sup.2] daily was administered using an autonomous chemotherapy delivery device (Deltec; Paris, France). Creatinine clearance was calculated every week during concomitant chemotherapy-radiotherapy and cisplatin delivery was stopped when clearance was equal to 60 mL/min or below this value.
Postprogram Therapy
At any time during chemotherapy or radiotherapy, patients who experienced a progressive disease discontinued the program and alternative treatment or best supportive care was offered to them. At the end of the radiotherapy, patients who achieved a complete response were followed up without treatment and patients who achieved a partial response were proposed to receive a maintenance chemotherapy consisting of vinorelbine, 30 mg/[m.sup.2] weekly for 10 weeks. Seventeen patients received this maintenance therapy.
Toxicity and Response Evaluation
Toxicity was analyzed by the frequency distribution of each grade of toxic events. Patients were reassessed for response at the end of the third chemotherapy cycle and 4 weeks after the completion of the second radiotherapy cycle. Pulmonary fibrosis was assessed at the third and sixth months of posttherapy follow-up using the subjective objective management analytic--late effects of normal tissues (SOMA-LENT) scale. This scale has been proposed by the European Organization for Research and Treatment of Cancer and the Radiation Therapy Ontology Group to characterize radiotherapy late effect of normal tissue.[11] For radiographic abnormalities, this scale described five classes; 0: normal radiographic lung appearance; 1: minimal infiltrates limited to the lobe of the primary disease; 2: dense and irregular pulmonary opacities; 3: confluent and dense pulmonary opacities but limited to the fields of radiotherapy; and 4: severe bilateral infiltrates outside the fields of radiotherapy with pulmonary retraction. The SOMA-LENT scale was also used to classify the subjective symptoms, in particular dyspnea. Pulmonary function and diffusing capacity for carbon monoxide were not systematically measured but were recorded in patients with dyspnea on exercise. Tumor response evaluation was done using the WHO recommendations[10] at the end of chemotherapy and at the end of radiotherapy. CT documents were used to define and measure indicator lesions. A complete response was defined as the complete disappearance of all lesions with normal histology on repeated bronchofiberoptic biopsy specimens. A partial response was defined as [is greater than or equal to] 50% reduction in the product of the two longest perpendicular diameters of the indicator lesions. Stable disease was defined as [is less than] 50% reduction or [is less than] 25% increase in this product. Finally, progressive disease was defined as [is greater than or equal to] 25% increase in this product or appearance of new lesions.
Platinum Assay
Platinum was determined in plasma by means of flameless atomic absorption spectrophotometry[12] with a spectrophotometer (Varian 1275-AA; Varian SA; Walnut Creek, CA). Sample size was 10 [micro]L and an auto sampler was used. Determinations were based on at least three injections of each sample. Samples of plasma were stored at 4 [degrees] C until platinum determination. Briefly, adjustment of the dosage was assessed by a standard curve achieved with five concentrations of platinum from 25 to 250 mg/mL plotted every third dosage. The lower limit of quantitation was 0.025 [micro]g platinum/mL and the coefficient of variation on triplicate samples was [is less than] 1%, The reproducibility of the assay gave a variation of [is less than] 2%.
Five patients were tested for the total plasma platinum concentration by sampling at time TO (before the radiotherapy fraction) and time T60 and T120, respectively: 60 and 120 min after the radiotherapy fraction.
Statistics
All analyses were done on an intent-to-treat basis. Response rates were calculated at the end of chemotherapy and at the end of radiation therapy. Quantitative variables (such as absolute neutrophil count at nadir) were expressed in median and interquartile range. Real dose-intensity was calculated taking into account the real on-treatment participation for each patient according to the method described by Hryniuk and Goodyear.[13] Survival was defined as the time from the first day of treatment to the date of death (all causes of death have been taken into account as events). Time to progression was defined as the time from the observation of response or stabilization to the date of progression. Probability of survival was estimated by the Kaplan-Meier method.[14] A software package was used (SAS; Cary, NC).
RESULTS
Patients' Characteristics
From April 1993 to October 1995, 44 patients were enrolled by two institutions (University Hospital and Cancer institute of Montpellier). Patient characteristics are shown in Table 1. One patient was retrospectively found to be ineligible due to a stage IIIa disease. Forty percent of the patients had a histologic demonstration of stage IIIb, whereas the diagnostic method of staging remained radiographic for the other patients. For these patients, mediastinal extent was characterized by a gross mediastinal involvement: ipsilateral and contralateral nodal stations in 5 patients (N3 nodal status) and/or nodal involvement [is greater than] 20 mm in diameter in 12 patients. Nine additional patients had radiographic evidence of main pulmonary artery involvement.
Compliance With Therapy
Thirty-nine of the 44 patients received the three-cycle chemotherapy program. Three patients discontinued after the first chemotherapy cycle: one of them experienced a reversible fever probably related to ifosfamide and its concomitant uroprotection (she then received another chemotherapy combination); two patients died early after cycle 1 delivery: one experienced a massive hemoptysis (that occurred before the onset of thrombocytopenia) and the other had a fatal cardiac failure related to a myocardial invasion by a left lower lobe large cell carcinoma. Both early deaths were reported as consequences of the disease and not related to the protocol. Median real dose-intensity was 82 to 83%. Compliance with therapy was also evaluated taking into account the median value of the ratio of received dose to the planned dose, for each cycle and each drug. This median value remained high for the second cycle (97%) but then decreased during the third cycle (77%) due to the dose reductions. Six patients did not receive the planned radiotherapy: the two above mentioned patients who died during cycle 1, the patient who did not receive the protocol regimen chemotherapy due to an ifosfamide-mesna-related fever, two patients who experienced a progression of the disease, and finally, one patient who refused to receive radiotherapy. Among the 38 patients who received the radiotherapy, 35 had the complete concomitant continuous cisplatin infusion. This treatment was stopped during the second course of radiotherapy for the remaining three patients owing to thrombocytopenia.
Tumor Response
Among the 44 patients, 41 received a minimum of two cycles and were therefore evaluable for response to chemotherapy. The three remaining patients were taken into account in this intent-to-treat analysis as nonresponders. Twenty-one patients achieved a tumor response (3 complete responses and 18 partial responses) giving an objective response rate of 48% (95% confidence interval [CI], 33 to 66%).
Thirty-eight patients underwent the complete concomitant chemotherapy-radiotherapy program and were evaluable for the response. The remaining patients were classified in the nonresponder group. There were 7 complete and 20 partial responses at time of the postradiotherapy tumor measurement. Thus the objective response rate was increased to 61% (95% CI, 47 to 75%).
Survival
Survival data were updated in October 1997. At that time, median follow-up was 38 months (range, 24 to 54 months). None of the patients was unavailable for follow-up. Median survival was 12 months (95% CI, 6 to 15 months). Probability of survival at 1, 2, and 3 years was 49%, 19%, and 5%, respectively (Fig 1). Median time to progression was 7 months (95% CI, 6 to 10 months). Locality of relapses was local in 63% of the patients, brain metastases in 24%, and hematogenous metastases to other sites in 13%. At time of reporting, five patients are still alive. They had achieved a complete or partial but nearly complete response at the end of the chemotherapy and radiotherapy program. Three of them are free of disease. Two experienced a single brain metastasis 1 year after the study entrance. Both patients underwent a concomitant high-dose ifosfamide and brain radiotherapy; they are still alive and free of disease, 30 and 41 months after they entered the study.
[Figure 1 ILLUSTRATION OMITTED]
Treatment Toxicity
During induction chemotherapy, myelosuppression was the limiting toxicity. However, this hematologic toxicity was mild to moderate and manageable (Table 2). During the first cycle, grade 3 to 4 neutropenia was the main toxicity whereas grade 3 to 4 thrombocytopenia was rare. During the following two cycles, the incidence and duration of neutropenia decreased slightly whereas the incidence of thrombocytopenia became limiting in both dose and timing of treatment. During the whole chemotherapy program, RBC transfusions were administered to 13 patients and platelet transfusions to 9 (2 of them received both transfusions). Twenty-three patients were readmitted to the hospital for a grade 2 or 3 infection requiring antibiotics infusions. No cisplatin dose reduction was imposed by renal toxicity inasmuch as none of the patients experienced a significant renal function impairment.
(*) Toxicities were assessed in the whole population. All patients had grade 3 alopecia.
([dagger]) For each patient, the worst nadir was taken into account whatever the cell line concerned.
([double dagger]) Percentages are calculated taking into account the 38 patients who underwent thoracic radiotherapy. Fifteen percent of the patients were nonevaluable for chronic pulmonary fibrosis due to progression of the disease that shortened follow-up.
During radiotherapy, the main toxic reaction was acute esophagitis. Afterwards, during follow-up, a relatively high rate of pulmonary fibrosis was observed using the radiographic score. Transient dyspnea was observed in those patients but only three suffered from long-term dyspnea on exercise. Four patients experienced a definite reduction of vital capacity ([is less than or equal to] 70% of predictive values) but fortunately, none of them suffered from a life-threatening pulmonary function impairment requiring long-term oxygen prescription.
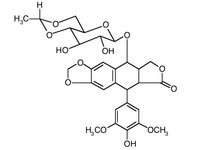
Total Plasma Platinum Concentration
The mean [+ or -] SD total platinum concentration before starting concomitant radiotherapy-chemotherapy was 0.26 [+ or -] 0.1 Pt [micro]g/mL. This concentration reflected the residual concentration of plasma platinum and resulted from the induction therapy. This mean concentration increased to 0.48 [+ or -] 0.16 [micro]g Pt/mL at the end of the first course of radiotherapy. The respective mean [+ or -] SD total plasma platinum concentrations before and after the second course of radiotherapy were 0.15 [+ or -] 0.09 and 0.32 [+ or -] 0.2 [micro]g platinum/mL. A typical pharmacokinetic pattern is shown in Figure 2.
[Figure 2 ILLUSTRATION OMITTED]
DISCUSSION
Multiple three-drug regimens have been tested in patients with advanced stage NSCLC. Two of the most extensively evaluated ones are CAP (cisplatin, doxorubicin [Adriamycin], cyclophosphamide) and MVP (mitomycin C, vinblastine or vindesine, cisplatin). Studies comparing MVP to a cisplatin plus vinblastine or etoposide regimen failed to demonstrate a difference in survival,[15,16] even though MVP might induce a higher response rate.[16] However, vindesine-cisplatin combination provided a higher response rate and longer survival than the CAP regimen as reported in the study by the Canadian National Cancer Institute,[17] but this difference might be explained by the lower cisplatin dose intensity in the CAP regimen. There is, hitherto, no proof of a putative benefit of three-drug chemotherapies in NSCLC but this lack of demonstration may be explained by the difficulties in maintaining the projected chemotherapy. As myelosuppression is the limiting toxic reaction, hematopoietic growth factors might offer an opportunity to deliver three-drug regimens safely and optimally.[18]
The cisplatin-etoposide-ifosfamide combination (VIP) is a putative therapy for unresectable NSCLC. Two recent phase II trials of VIP regimen exemplified its high hematologic toxicity as a limiting factor.[19,20] We have previously published two phase II studies using the present dosage and schedule of VIP combination in NSCLC.[6,19] Taken as a whole, the three studies (including the one presented herein) consisted of 97 NSCLC patients. This population was selected owing to its relatively good prognosis among other subgroups with unresectable NSCLC inasmuch as locally advanced stages were predominant (stage IIIa: 37%; stage IIIb: 54%; and stage IV: 9%). In addition, the performance status of this population was 0 or 1 in 78% of the population and 2 in the remaining patients. Squamous cell carcinoma was the predominant histologic subtype (63%). Adenocarcinomas and large cell carcinomas had a 24% and 13% frequency, respectively. In this population, we observed 55 objective responses giving a 57% objective response rate with a 95% CI comprised between 47% and 66%. Among these patients, nine achieved a complete response, five of them having been confirmed by surgery (complete response rate: 9%; 95% CI: 3.5 to 15%). During the first study, performed without hematopoietic growth factor,[19] one toxic-related death occurred whereas none was observed during the two others, including the present one. However, we must stress the fact that, despite r-metHuG-CSF support, hematologic toxic events requiring transfusions and/or antibiotics were responsible for unplanned hospitalizations. Optimal delivery of chemotherapy is still limited by other toxic reactions, mainly thrombocytopenia, but the successful close intensity observed herein deserves further studies designed to test the hypothesis of a dose intensity-survival relationship in NSCLC. The activity of this regimen in NSCLC seems promising and it fits the criteria of neoadjuvant chemotherapy that requires short duration and high activity.[21]
Concomitant chemotherapy and radiotherapy has been proposed in the setting of locally advanced NSCLC.[5] Although this approach could enhance the local control of the disease, it does not seem, to avoid distant metastasis.[5,22,23] This is the rationale for the combination of the two approaches described herein, ie, induction chemotherapy followed by a radical radiotherapy with combined cisplatin infusion.
In our study, we used a 24-h infusion modality of administration of 6 mg/d/[m.sup.2] of cisplatin using an autonomous chemotherapy delivery device. Although studied in a small subgroup of patients, the pharmacokinetics of the total platinum concentration suggested that this method allows a stable concentration of cisplatin. Whether this modality is able to enhance the radiosensitization effect of cisplatin by limiting DNA repair between two radiotherapy fractions remains to be established. It is noteworthy that, despite the combined treatment, the local control of the disease remains insufficient, an observation also made in the study by Blanke et al.[22] In addition, the high rate of radiographic lung fibrosis suggests that other modalities of fractionation such as continuous 6-week delivery of lower radiotherapy dosage by fraction must be investigated to reduce the late effects of normal lung tissue.
Our study suggests that neoadjuvant VIP followed by concomitant radiotherapy-chemotherapy is feasible in patients suffering from stage IIIb NSCLC.
REFERENCES
[1] Gregor A. Controversies in the treatment of non-small cell lung cancer. Eur J Cancer 1991; 27:362-366
[2] Non-small cell lung cancer collaborative group. Chemotherapy in non-small cell lung cancer: a meta-analysis using updated data on individual patients from 52 randomized clinical trials. BMJ 1995; 311:899-909
[3] Rosell R, Gomez-codina J, Camps c, et al. A randomized trial comparing preoperative chemotherapy plus surgery with surgery alone in patients with non-small cell lung cancer. N Engl J Med 1994; 330:153-158
[4] Roth JA, Fossella F, Komaki R, et al. A randomized trial comparing perioperative chemotherapy and surgery, with surgery alone in resectable stage III non-small cell lung cancer. J Natl Cancer Inst 1994; 86:673-680
[5] Schaake Koning C, Van Der Bogaert W, Dalesio O, et al. Effects of concomitant cisplatin and radiotherapy on inoperable non-small cell lung cancer. N Engl J Med 1992; 326: 524-530
[6] Gautier V, Pujol JL, Zinai A, et al. r-metHuG-CSF support to ifosfamide, cisplatin, etoposide chemotherapy in non-small cell lung cancer. Lung Cancer 1996; 14:343-351
[7] Sobin LH, Hermanek P, Hutter BVP. TNM classification of malignant tumours. 4th ed. Geneva, Switzerland: UICC, 1987
[8] Tisi GM, Friedman PJ, Peters RM, et al. American Thoracic Society: clinical staging of primary lung cancer. Am Rev Respir Dis 1982; 125:659-664
[9] Mountain CF. Revisions in the international item for staging lung cancer. Chest 1997; 111:1710-1717
[10] World Health Organization. WHO handbook for reporting the results of cancer treatment. Geneva, Switzerland: WHO Offset Publication No. 48, 1979
[11] Rubin P, Constine S, Fajardo LF, et al. RTOG late effects working group: overview: late effects of normal tissues (LENT) scoring system. Int J Radiat Oncol Biol Phys 1995; 31:1041-1042
[12] Pujol JL, Cupissol D, Gestin-Boyer C, et al. Tumor tissue and plasma concentrations of platinum during chemotherapy of non-small cell lung cancer patients. Cancer Chemother Pharmacol 1990; 27:72-75
[13] Hryniuk W, Goodyear M. The calculation of received dose intensity. J Clin Oncol 1990; 8:1935-1937
[14] Kaplan EL, Meier P. Nonparametric estimation from incomplete observations, J Am Stat Assoc 1958; 53:457-481
[15] Crino L, Tonato M, Darvish S, et al. A randomized trial of 3 cisplatin-containing regimens in advanced non-small cell lung cancer: a study of the Umbrian lung cancer group. Cancer Chemother Pharmacol 1990; 26:52-,56
[16] Gralla RJ, Kris MG, Burke MT, et al. The influence of addition of mitomycin to vindesine and cisplatin in a random assignment trial in 120 patients with non-small cell lung cancer [abstract]. Proc Am Soc Clin Oncol 1986; 5:182
[17] Rapp E, Pater JL, Willan A, et al. Chemotherapy can prolong survival in patients with advanced non-small cell lung cancer--report of a Canadian multicenter randomized trial. J Clin Oncol 1988; 6:633-641
[18] Groopman JE, Molina JM, Scadden DT. Hematopoietic growth factors: biology and clinical applications. N Engl J Med 1989; 321:1449-1459
[19] Pujol JL, Rossi JF, Le Chevalier T, et al. Pilot study of neoadjuvant ifosfamide, cisplatin, and etoposide in locally advanced non-small cell lung cancer. Eur J Cancer 1990; 26:798-801
[20] Shepherd FA, Goss PE, Latreille J, et al. A phase II study of ifosfamide, cisplatin, etoposide in patients with advanced non-small cell lung cancer: a preliminary report. Semin Oncol 1990; 17:19-23
[21] Shepherd FA. Induction chemotherapy for locally advanced non-small cell lung cancer. Ann Thorac Surg 1993; 55:1585-1592
[22] Blanke C, Ansari R, Mantravadi R, et al. Phase III trial of thoracic irradiation with or without cisplatin for locally advanced unresectable non-small cell lung cancer: a Hoosier Oncology Group Protocol. J Clin Oncol 1995; 13:1425-1429
[23] Shaw E, McGinnis W, Jett J, et al. Pilot study of accelerated hyperfractionated thoracic radiation therapy plus concomitant chemotherapy in patients with unresectable stage III non-small cell carcinoma of the lung. J Natl Cancer Inst 1993; 85:321-323
(*) From the Department of Respiratory Diseases (Drs. Pujol, Lafontaine, Quantin, Khial, and Michel), Hopital Arnaud de Villeneuve, and the Cancer Institute (Drs. Lafontaine, Reme-Saumon, and Cupissol), Centre Val d'Aurelle, Montpellier, France.
This study has been supported by grants from the French League Against Cancer (Herault and Aude committees) and the "Groupement des Entreprises Francaises dans la Lutte contre le Cancer." Manuscript received May 6, 1998; revision accepted July 29, 1998. Correspondence to: Jean-Louis Pujol, MD, Hopital Arnaud de Villeuve, Avenue du doyen Giraud, 34295 Montpellier Cedex 5, France
COPYRIGHT 1999 American College of Chest Physicians
COPYRIGHT 2000 Gale Group