YOUR PATIENT can use patient-controlled analgesia (PCA) to administer opioid medication to control postoperative or chronic pain. The LV. route is the most common option.
DO
* Teach your patient and his family why and how to use PCA.
Assess his ability to push the button and warn the family not to push it unless he clearly tells them he needs and wants a dose and can't push it himself.
* Determine his baseline pain level, vital signs, level of consciousness, mental status, and level of sedation. Also assess current or prior opioid use and medication allergies.
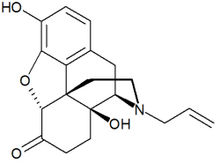
* Make sure that the opioid antagonist naloxone (Narcan) is readily available.
* Establish IN. access. Connect the PCA tubing to the drug reservoir, prime and clamp it, and connect it to the IN. line at the Y connector nearest the insertion site.
With another RN, verify the PCA pump settings against the order. Check the patients name; the drug, route, and concentration; dose volume limits; lockout interval and frequency; and 4-hour limit. Settings should be rechecked every time the syringe, parameters, or caregiver changes.
* Lock the machine. Look for digital cues that it isn't properly set and make corrections, if necessary.
* Administer the prescribed loading dose to control your patients pain. Encourage him to press the button as soon as he begins to feel pain. Reassure him that he won't get too much medication.
* Monitor the insertion site for swelling, pain, tenderness, redness, and coolness (which may indicate catheter displacement or phlebitis).
* According to facility policy, monitor your patient periodically for pain, excessive sedation, changes in mental and respiratory status, and hypotension.
* At least every 4 hours, document the pump settings, number of bolus doses given, number of attempts, total amount of drug given, patient education, and response to treatment. Document the amount of any wasted opioid.
DON'T
* Don't start PCA until two nurses independently calculate the pump settings.
* Don't let anyone administer doses unless the patient can't push the button himself and clearly communicates that he needs and wants a dose.
* Don't give meperidine (Demerol) via PCA because it could be neurotoxic.
SELECTED REFERENCES
Berman, A., et al. (eds): Kozier fr Erb's Techniques in Clinical Nursing, 5th edition. Upper Saddle River, NJ., Pearson Education, Inc., 2002.
Smeltzer, S., and Bare, B.(eds): Brunner and Suddarth's Textbook of Medical-Surgical Nursing, 9th edition. Philadelphia, Pa., Lippincott Williams a Wilkins. 2000.
Richard L. Pullen, Jr, is a professor of nursing at Amarillo (Tex.) College. Each month, this department illustrates key clinical points for a common nursing procedure. Because of space constraints, it's not comprehensive.
Copyright Springhouse Corporation Jul 2003
Provided by ProQuest Information and Learning Company. All rights Reserved