The Quality Standards Subcommittee of the American Academy of Neurology (AAN) has released evidence-based recommendations for the initiation of pharmacologic and surgical therapies for patients with essential tremor. The recommendations are based on a systematic literature review and were rated for strength of evidence. The full report was published in the June 28, 2005, issue of Neurology and can be found online at http://www. neurology.org/cgi/content/full/64/12/2008.
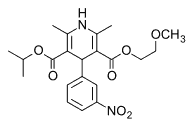
Essential tremor is defined as the presence of postural and kinetic tremor. Classic essential tremor most commonly affects the upper limbs, but it also can affect a head, lower limbs, voice, tongue, face, and trunk. Although essential tremor does not reduce life expectancy, and symptoms are limited to tremors, the condition may cause substantial physical and psychosocial disability (e.g., difficulty with writing, drinking, eating, dressing, speaking, and other fine motor skills). Propranolol (Inderal) is the only drug approved by the U.S. Food and Drug Administration for the management of essential tremor. However, an estimated 30 percent of patients will not respond to this medication. Other drugs may be used, and surgical intervention is an invasive alternative to pharmacologic therapy.
Recommendations
PHARMACOLOGIC THERAPY
Table 1 summarizes the evidence for the pharmacologic management of essential tremor.
Level A. Propranolol was effective in managing limb tremor related to essential tremor. The results of treatment with once-daily, long-acting propranolol (Inderal LA) were similar to those of standard propranolol in managing limb tremors. Physicians might consider the use of propranolol, long-acting propranolol, or primidone (Mysoline) to manage limb tremor in patients with essential tremor, depending on concurrent medical conditions and potential side effects. Primidone and propranolol were equally effective for initial treatment of patients with limb tremor.
Trazodone (Desyrel) did not significantly affect postural or kinetic tremor and is not recommended for managing limb tremor.
Level B. Alprazolam (Xanax), atenolol (Tenormin), gabapentin (Neurontin) mono-therapy, sotalol (Betapace), and topiramate (Topamax) may reduce limb tremor associated with essential tremor. Atenolol, gabap-patient's entin monotherapy, sotalol, and topiramate may be used for limb tremor, although data are limited. Alprazolam should be used with caution because of the potential for abuse. Propranolol should be considered for the management of head tremor.
Acetazolamide (Diamox), isoniazid (INH), and pindolol (Visken) probably do not reduce limb tremor and are not recommended for managing essential tremor.
Level C. Nadolol (Corgard) and nimodipine (Nimotop) may be considered to manage limb tremor associated with essential tremor, but clonazepam (Klonopin) should be used with caution because of its potential for abuse and withdrawal symptoms. Clozapine (Clozaril) is recommended only for refractory cases of essential tremor because of the risk of agranulocytosis.
Methazolamide (Neptazane), mirtazapine (Remeron), nifedipine (Procardia), and verapamil (Calan) probably do not reduce limb tremor and are not recommended for managing essential tremor.
SURGICAL THERAPY
Table 2 summarizes the evidence for the surgical management of essential tremor. Surgical intervention should be considered only for patients who do not respond to pharmacologic therapy.
Level C. Sufficient evidence was available only on the effectiveness of chronic thalamic deep brain stimulation (DBS) and thalamotomy for managing essential tremor. Unilateral thalamotomy may be used to manage limb tremor, but bilateral thalamotomy is not recommended because of adverse effects. Thalamic DBS may be used to treat patients with limb tremor, but insufficient evidence exists to make a recommendation regarding its effectiveness in managing head and voice tremor. Although DBS has fewer adverse effects, physicians should choose between DBS and thalamotomy based on the patient's intraoperative complications compared with the practicality of the procedures.
Level U. gamma knife surgery, chronic thalamic DBS (head), chronic thalamic DBS (voice), and unilateral versus bilateral DBS (hand) should be considered unproven therapies at this time.
Conclusion
The committee concludes that research on the management of essential tremor is limited, and additional prospective, double-blind, placebo-controlled trials are needed to better determine the effectiveness and side effects of pharmacologic and surgical therapy for essential tremor.
COPYRIGHT 2005 American Academy of Family Physicians
COPYRIGHT 2005 Gale Group