Objective: The administration of antidepressant drugs was shown to positively affect the rate of smoking cessation. This study evaluates the efficacy of nortriptyline in an antismoking program.
Methods: A possible randomized double-blind study that included 144 patients who were randomized to receive nortriptyline, 75 mg/d (68 patients), or placebo (76 patients), during 6 consecutive weeks. All patients attended behavioral group orientation for 5 weeks. The rate of success, complications, adherence to the regime, and factors of pretreatment prognosis were evaluated (multivariate analysis).
Results: The groups were balanced in relation to the characteristics of the patients on entering the study. Patients receiving nortriptyline showed significantly higher cessation rate (55.9%) compared to the group receiving placebo (23.3%; p < 0.001). In a univariate analysis on prognosis factors influencing the rate of cessation in our study, the Fagerstrom test results (p = 0.005) and nortriptyline (p < 0.001) were identified. Logistic regression showed that a Fagerstrom test score of < 7 (odds ratio [OR], 3.1; 95% confidence interval [CI], 1.47 to 6.7; p = 0.003) and nortriptyline use (OR, 4.1; 95% CI, 2 to 8.3; p < 0.001) were independent factors impacting the rate of success for smoking cessation. No significant complications were observed in the nortriptyline group.
Conclusion: This study showed that nortriptyline significantly increases the smoking cessation rate in chronic smokers, as compared to the placebo group, without any significant side effects.
Key words: nortriptyline; smoking cessation; tobacco
**********
Cigarette smoking remains the most important cause of preventable morbidity and mortality in developed countries. It is estimated that in the year 2001, smoking-related diseases will account for > 400,000 deaths just in the United States. (1,2)
In Brazil, every year 200,000 people die of tobacco-related illnesses. The prevalence of smoking in Brazil is approximately 35% of the population. (1)
Ceasing to smoke clearly lowers the risk of death from cardiovascular and cerebrovascular diseases, COPD, and cancer. In comparison with those patients who continued to smoke, those ceasing to smoke before the age of 50 years show a 50% reduction in the risk of all causes of death in the following 16 years. (1) Stopping smoking can increase life expectancy, even for those ceasing to smoke after the age of 65 years. (1)
Despite the fact that the use of tobacco constitutes the most serious common medical problem, access to effective treatment remains limited for the majority of Brazilians. The difficulty in stopping smoking is highlighted by the fact that only 2.5% of all smokers actually succeed in remaining abstinent for a year. (2) One of the main problems for those attempting to stop smoking is the syndrome of withdrawal from nicotine.
The association between abstinence from nicotine and the presence of depressive symptoms has been widely reported in the literature. (3-13) Studies showed that the association between smoking and depression is specific for nicotine-dependent individuals, being directly proportional to the degree of dependence on nicotine as evaluated by specific dependence tests. (6,8,10,14)
Several studies have evaluated the effect of the administration of antidepressants on abstinence from nicotine. Initial trials with doxepin, a tricyclic antidepressant, showed positive results in aiding abstinence from nicotine. (15) A form of therapy with sustained-release bupropion, a unicyclic antidepressant, also appeared to be effective in the treatment of abstinence from nicotine. (16)
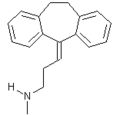
Few studies in the literature have assessed the effectiveness of nortriptyline, which is a tricyclic antidepressant with broad previous clinical experience in therapy for depression. (17,18) This double-blind randomized study evaluated the safety and effectiveness of nortriptyline administered to smokers enrolled in an antismoking program.
MATERIALS AND METHODS
From May 1999 to June 2000, 236 patients were registered by the Smokers' Support Group at the A.C. Camargo Cancer Hospital in Sao Paulo, Brazil. Smokers enrolled in the group spontaneously. At the initial interview with the psychiatrist, the Beck and Fagerstrom test questionnaires were applied.
The Beck questionnaire (19) includes 21 questions that screen for depression symptoms. The scoring of this evaluation ranges from 0 to 63 points. Patients scoring [greater than or equal to] 20 points were excluded from the study. At the initial interview, the Fagerstrom questionnaire also was used to determine the degree of dependence on nicotine. Individuals who scored [greater than or equal to] 7 points were considered to be highly dependent on nicotine. (20)
The inclusion criteria were as follows:
1. Age range from 18 to 65 years;
2. Smoking habit of an average of [greater than or equal to] 15 cigarettes per day in the last year;
3. Score of [less than or equal to] 20 on the Beck questionnaire;
4. Good general health, as evaluated by a clinician;
5. Had not taken antidepressants at least for the last month;
6. Had not taken benzodiazepine derivatives, except in cases in which the patient had been receiving the drug over a long period (ie, for > 6 months); and
7. Had not taken antipsychotic medication for at least 1 month.
The exclusion criteria were as follows:
1. Patient had mental deficiency or demential syndromes;
2. Personal history of arrhythmias and a recent myocardial infraction;
3. Was pregnant or breast feeding;
4. History of glaucoma or urinary retention;
5. History of thyroid disease;
6. History of epilepsy or chronic convulsive syndromes; and
7. Currently receiving therapy for nicotine replacement.
Following the first interview for assessment, 182 patients meeting the criteria for inclusion were accepted into the study and then submitted to further clinical evaluation with a thorough medical history, physical examination, chest radiograph, and ECG. Thirty patients were excluded at this point due to ECG alterations, including arrhythmias and evidence of ischemic heart disease, and 8 patients showed a low performance status. The remaining 144 patients began the study.
Following clinical evaluation, all patients received full information on the protocol and signed an informed consent form. They were then randomized to receive nortriptyline (Pamelor; Novartis; Sao Paulo, Brazil; 76 patients) or placebo (68 patients). Each patient chose a blind number from a box, with each number corresponding to a "medication kit" that was externally undistinguishable. Patients and professionals participating in this study were blindfolded for this distribution. All patients were instructed to take their medication daily, and to note and report on any side effects.
Following the randomizing, subgroups of 15 patients were formed. These subgroups returned weekly for behavioral orientation related to stopping smoking (ie, sessions in support therapy in groups coordinated by the psychiatrist, based on cognitive-behavioral theory). These sessions were conducted by the same psychiatrist for all patients. The patients began receiving medication 1 week before the beginning of the group sessions. The dose was increased weekly from one tablet (25 mg), reaching a dose of three tablets (75 mg) until the end of the study (42 days). The same progression of daily tablets was given to the placebo group.
At the end of the program, the success of the treatment was registered individually. It was considered to be successful for those individuals who stopped smoking for at least I week at the end of the treatment period. At the end of the study, after 3 months, we established phone contact with participants to determine the rate of abstinence from nicotine after that follow-up period.
Statistical Analysis
The groups were compared for all variables using the Student t test to compare means and the [chi square] test to compare category variables.
Variables determined at the first interview (ie, marital status, education, race, age when the patient had begun to smoke, the average number of cigarettes smoked per day, the motivation to stop, family history of depression, personal history of depression, Fagerstom test score, age on admission to the study, and sex) were evaluated for their impact on the cessation of smoking in the two groups.
The cessation rates were evaluated using univariate and multivariate analyses that were carried out to identify the prognostic factors that could affect the success rate. Multiple logistic regression, with a forward stepwise selection was used. The significance of the final model was assessed using the Hosmer-Lemeshow test. (21) Statistical analyses were performed with a computer software package (SPSS for Windows, version 8.0; SPSS; Chicago, IL). The differences were considered to be significant at the p < 0.05 level.
RESULTS
The study was completed by 144 patients. The group completing the treatment was composed predominantly of women, and 71% of the group were married.
Ten patients abandoned the study before reaching the daily three-tablet dose (one patient reported impotence with a dose of 25 mg nortriptyline), and 5 patients abandoned the study at follow-up (placebo group, 3 patients; and nortriptyline group, 2 patients). Three patients complained of diarrhea, sore throat, and unspecific muscular pain. Of these patients, two were receiving placebo and one was receiving nortriptyline. One patient receiving nortriptyline referred to commuting difficulties. Patients beginning to smoke again and then stopping were considered as not having stopped smoking (ie, failure).
Ten patients abandoned the treatment after reaching a dosage of three tablets per day (equivalent to 75 mg nortriptyline). Five patients referred to intolerance to the drug as the cause for abandoning treatment. Of these patients, three were receiving nortriptyline and two were receiving placebo. There were complaints of intense dryness in the mouth, Four patients receiving placebo and one patient receiving nortriptyline said that they abandoned treatment because the treatment did not work.
Table 1 shows the results of the univariate analysis for prognostic factors. The use of nortriptyline (p < 0.001) and the score on the Fagerstrom test (p = 0.005) were statistically significant in relation to success in ceasing to smoke.
The results of the multiple logic regression are shown in Table 2. All the variables with p < 0.20 in the univariate analysis were tested. The Fagerstrom test variable score, age, and the use of nortriptyline were significant independent factors impacting on smoking cessation.
In Table 3, we analyzed the population studied, according to the final status on smoking (ie, ceasing or not ceasing to smoke). The Fagerstrom score was the only significant predictor of success (p = 0.001).
In Table 4, we separately analyzed those patients admitted to the study with Fagerstrom scores of [greater than or equal to] 7. The impact of nortriptyline or placebo on ceasing to smoke was assessed. In this highly dependent population, patients who received nortriptyline showed a significantly higher rate of smoking cessation (60.4%) compared to the group that received placebo (7%). There was a statistically significant difference in the results between the groups (p < 0.001).
There were no statistically significant differences between nortriptyline and placebo in ceasing to smoke for the group with the low Fagerstrom scores (ie, < 7; p = 0.135), as shown in Table 5.
Table 6 shows the adverse reactions and symptoms of abstinence in both groups. There were no significant differences between the groups.
After 3 months of follow-up after the end of the treatment period, 26.5% of the patients who received nortriptyline and 5.3% patients who received placebo had ceased to smoke (p = 0.0006). Fourteen patients receiving placebo and 20 patients receiving nortriptyline began to smoke again during this follow-up period. Seven patients receiving placebo referred to the presence of depressive symptoms, and 10 patients referred to anxiety symptoms as the cause. All patients receiving nortriptyline referred to anxiety symptoms as the cause.
After 6 months' follow-up from the end of the treatment period, 20.6% of patients who had received nortriptyline and 5.3% of patients who had received placebo had ceased to smoke (p = 0.012). Two patients who had received nortriptyline began to smoke again at this follow-up period. These patients referred to anxiety symptoms as the cause.
DISCUSSION
Nicotine replacement, in the form of patches, chewing gum, and aerosols, has been widely used to diminish nicotine deprivation symptoms in individuals trying to stop smoking. (22) Antidepressant drugs administered for this purpose also have been evaluated. (23,24)
Bupropion is the only antidepressant drug approved by the US Food and Drug Administration for the treatment of tobacco addiction. In the United States, there has been wide experience with the use of this drug, which has potential side effects in patients predisposed to seizures. (25,26) The risk of seizures is related to the patients' predisposition, to the clinical situation (eg, head injury, brain tumor, alcohol abuse, or cocaine addiction), and to the concomitant medications used (eg, insulin, antipsychotic medication, antidepressant medication, or theophylline). Approximately 35% of patients receiving 300 mg/d bupropion have insomnia, and there have been no clinical trials establishing the safety of bupropion in patients with cardiovascular disease. (27)
On the other hand, nortriptyline has been shown to be an effective treatment. (17,18) The drug is well-known, having been widely used in several countries since the decade of the 1960s. In comparison to other tricyclic antidepressants, nortriptyline has several therapeutic advantages as follows: minimal night stimulation; low incidence of anticholinergic side effects; low incidence of orthostatic hypotension; and low risk of seizures. Nortriptyline should be used with caution in patients having cardiovascular diseases. The clinical experience in relation to this factor is large, and the risks have been established. (28,29) Among tricyclic antidepressants, nortriptyline has the lowest rates of side effects, with acceptance in the elderly population. The most common side effects are a dry mouth and constipation.
In the present prospective, randomized, double-blind study with 144 smokers, 23.7% of the patients receiving placebo stopped smoking, compared to 55.9% of the patients receiving nortriptyline (p < 0.001). Individuals were considered to have stopped smoking if they claimed total abstinence from cigarette smoking for at least 1 week. Our results were comparable to those of another randomized study by Hurt et al, (16) which included 615 patients who had been treated with bupropion. In the sixth week of the study, the abstinence rate was 19% for the group receiving placebo and 44.2% for the group receiving bupropion (p < 0.001).
Prochazka et al (18) in a randomized, double blind, placebo-controlled study with 214 patients, evaluated the effects of nortriptyline on the rate of ceasing to smoke. The success rate for the group that received the active drug was 50%, compared to 32% for the group receiving placebo. Only 12% of the patients had a history of depression, compared to 48% in the population of our study. Despite the difference between the two studies in the methodologies used to obtain this information (in our study, the report on psychiatric treatment for the diagnosis of depression was considered as previous history of depression, while in the study by Prochazka et al, (18) a structured questionnaire was applied [ie, the diagnostic interview schedule]), the difference between the two populations could explain the different in the rate of success in ceasing to smoke.
The study by Hall et al, (17) which was another placebo-controlled, double blind, randomized study of 199 patients receiving nortriptyline, resulted in an initial abstinence rate at 10 weeks of 40% for patients receiving placebo and 70% for patients receiving nortriptyline. The methodology used in our study permitted adjustment in the doses according to the serum levels of the patients. This may explain the higher success rates in that study compared to those in our study. Hall et al (17) separately analyzed the rates of smoking cessation in patients with and without previous histories of major depression, receiving or not receiving behavioral or educational intervention, and the association with the administration of placebo or nortriptyline. The best results were obtained with educational intervention, in those patients having no personal history of depression, who received the active drug. A negative history of depression was, however, the most important factor for the success of the treatment.
Jorenby et al, (30) in a study of the use of bupropion, placebo, the nicotine patch, or the nicotine patch plus bupropion in 893 individuals, excluded patients having a previous history of several psychiatric pathologies (eg, panic, psychoses, bipolar disorder, alimentary disorder, dependence on psychoactive drugs, and alcohol). A significant difference in the rate of smoking cessation was observed, as follows: nicotine patch, 48.0%; bupropion, 60.2%; nicotine patch plus bupropion, 66.5%; placebo, 33.8%. The exclusion of a large portion of the psychiatric population could account for the effectiveness of the medications used in this study, compared to the study by Hurt et al (16) with bupropion.
There were no references in the previous studies to the use of the Fagerstrom test. Our study suggests that the use of this test is an important forecaster of smoking cessation success, showing that the success of the medication in relation to placebo was only significant for patients with Fagerstrom scores of [greater than or equal to] 7, possibly identifying a subgroup of smokers that would benefit from treatment with nortriptyline.
CONCLUSION
We concluded that nortriptyline is an effective and well-tolerated drug for the treatment of addiction to smoking, with success rates that are comparable to those using bupropion as treatment. Nortriptyline was especially effective in smokers having a high dependence on nicotine (Fagerstrom score, [greater than or equal to] 7), but Fagerstrom scores can only indicate that a trend may be present. Further studies may be needed to solidify this relationship.
REFERENCES
(1) World Health Organization. Framework Convention on Tobacco Control [monograph on line]. Available at: http:// www5.who.int/tobacco. Accessed July 12, 2002
(2) Giovino GA, Henningfield JE, Tomar SL, et al. Epidemiology of tobacco uses and dependence. Epidemiol Rev 1995; 17:48- 65
(3) Breslau N, Kilbey MM, Andreski P. Nicotine dependence, major depression, and anxiety in young adults. Arch Gen Psychiatry 1991; 48:1069-1074
(4) Breslau N, Kilbey MM, Andreski P. Nicotine withdrawal symptoms and psychiatric disorders: findings from an epidemiologic study of young adults. Am J Psychiatry 1992; 149: 464-469
(5) Breslau N, Kilbey M, Andreski P. Nicotine dependence and major depression: new evidence from a prospective investigation. Arch Gen Psychiatry 1993; 50:31-35
(6) Breslau N, Kilbey MM, Andreski P. DSM-III-R: nicotine dependence in young adults; prevalence, correlate and associated psychiatric disorders. Addiction 1994; 89:743-754
(7) Covey SL, Glasman AH, Stetner F. Depression and depressive symptoms in smoking cessation. Compr Psychiatry 1990; 31:350-354
(8) Escobedo LG, Kirch DG, Anda RF. Depression and smoking initiation among US Latinos. Addiction 1996; 91:113-119
(9) Glassman AH, Helzer JE, Covey LS, et al. Smoking, smoking cessation, and major depression. JAMA 1990; 264:1546-1549
(10) Glassman AH, Covey LS, Dalack GW, et al. Smoking cessation, clonidine, and vulnerability to nicotine among dependent smokers. Clin Pharmacol Ther 1993; 54:670-679
(11) Hemenway D, Solnick SJ, Colditz GA. Smoking and suicide among nurses. Am J Public Health 1993; 83:249-251
(12) Hughes JR. Genetics of smoking: brief review. Behav Ther 1986; 17:335-345
(13) Kendler KS, Neale MC, Maclean CJ, et al. Smoking and major depression. Arch Gen Psychiatry 1993; 50:36-43
(14) D' Mello DA, Flanagan C. Seasons and depression: the influence of cigarette smoking. Addict Behav 1996; 21:671-674
(15) Edwards NB, Murphy JK, Downs AD, et al. Doxepin as an adjunct to smoking cessation: a double-blind pilot study. Am J Psychiatry 1989; 146:373-376
(16) Hurt RD, Sachs DPL, Glover ED, et al. A comparison of substained-release bupropion and placebo for smoking cessation. N Engl J Med 1997; 337:1195-1202
(17) Hall SM, Reus VI, Munoz RF, et al. Nortriptyline and cognitive-behavioral therapy in the treatment of cigarette smoking. Arch Gen Psychiatry 1998; 55:683-693
(18) Prochazka AV, Weaver MJ, Keller RT, et al. Randomized trial of nortriptyline for smoking cessation. Arch Intern Med 1998; 158:2035-2039
(19) Gorenstein C, Andrade L. Validation of Portuguese version of the Beck Depression Inventory in Brazilian subjects. Braz J Med Biol Res 1996; 29:453-457
(20) Fagerstrom KO, Schneider NG. Measuring nicotine dependence: a review of the FagerstrOm tolerance questionnaire. J Behav Med 1989; 12:159-181
(21) Horner DW, Lemeshow S. Applied logistic regression. New York, NY: John Wiley and Sons, 1989
(22) Thompson GH, Hunter DA. Nicotine replacement therapy. Ann Pharmacother 1998; 32:1067-1075
(23) Ferey LH. Non-nicotine pharmacotherapy for smoking cessation. Prim Care 1999; 26:653-669
(24) Covey SL, Sullivan MA, Johnston JA, et al. Advances in non-nicotine pharmacotherapy for smoking cessation. Drugs 2000; 59:17-31
(25) Ascher JA, Cole JO, Colin J-N, et al. Bupropion: a review of its mechanisms of antidepressant activity. J Clin Psychiatry 1995; 56:395-401
(26) Johnston JA, Lineberry CG, Ascher JA, et al. A 102-center prospective study of seizure in association with bupropion. J Clin Psychiatry 1991; 52:450-456
(27) Roose SP, Dalack GW, Glassman AH, et al. Cardiovascular effects of bupropion in depressed patients with heart disease. Am J Psychiatry 1991; 148:512-516
(28) Burrows GD, Maguire KP, Scoggins BA, et al. Plasma nortriptyline and clinical response: a study using changing plasma levels. Psychol Med 1977; 7:87-91
(29) Cooper TB, Simpson GM. Prediction of individual dosage of nortriptyline. Am J Psychiatry 1978; 135:333-335
(30) Jorenby DE, Leischow SJ, Nides MA, et al. A controlled trial of substained-release bupropion, a nicotine patch or both for smoking cessation. N Engl J Med 1999; 340:685-691
* From the Departments of Psychiatry (Drs. da Costa and Lourenco) and Thoracic Surgery (Dr. Younes), A.C. Camargo Cancer Hospital, Sao Paulo, Brazil.
Received March 8, 2001; revision accepted February 14, 2002. Correspondence to: Celia Lidia da Costa, MD, Department of Psychiatry, A.C. Camargo Cancer Hospital, Rua Prof. Antonio Prudente, No. 211, 01509-010 Sao Paulo, S.P., Brazil
COPYRIGHT 2002 American College of Chest Physicians
COPYRIGHT 2002 Gale Group