Historically, topical antifungal agents have had nonspecific actions with minimal efficacy. Astringents formulated with zinc and aluminum create a dry environment that limits fungal cell growth.[1] Sodium bicarbonate was used to treat vaginitis after an increase in local pH was noted to provide symptomatic relief for women with this condition.[1] Keratolytic agents have fungistatic activity in that they cause epidermal desquamation.
It was not until 1951 that nystatin was extracted from an Actinomyces species in the soil and then developed into an antifungal agent.[2] Since that time, multiple topical antifungal agents with several different mechanisms of action have been developed. Topical agents, formulated alone or with substances that enhance their activity, continue to be developed.
As new agents emerge, product selection has become increasingly difficult. However, the most effective antifungal agent for a given situation can be chosen by considering the mechanisms, efficacies, side-effect profiles and costs of the various agents.
Topical antifungal formulations have a spectrum of activity against superficial infections, including those caused by dermatophytes (Trichophyton and Microsporum species), Candida organisms and Malassezia furfur (also called Pityrosporum orbiculare), the lipophilic yeast that causes tinea versicolor and, possibly, seborrheic dermatitis.[3]
Systemic therapy should be considered when a fungal infection involves the scalp, the nails or large areas of the skin, when patients have altered immunity or when an infection persists beyond the appropriate treatment period.[4] In patients with onychomycosis or tinea capitis, topical medications may be used as supplements to systemic antifungal treatment to decrease the risk of the spread of infection.
Single-dose systemic medications are used to treat uncomplicated vulvovaginitis, with cure rates comparable to those for topical regimens.[5] However, single-dose regimens offer only limited relief within the first 24 hours for extensive local symptoms, and adjunctive topical medications may be needed.[5]
Shortened therapeutic courses for vulvovaginitis and other mycotic infections are now popular. The efficacy is similar to that of more traditional regimens, with the prolonged tissue levels of the newer agents being used to advantage in shortened courses.
Pharmacology
Antifungal drugs target different stages in the growth and reproduction of a fungal cell. The specificity of a drug's action on the fungal cell or its products determines its ability to limit host cell toxicity.[1] The drug may be fungicidal or fungistatic. It is not necessary for a drug to have fungicidal activity unless the host has altered immunity.[1] Most antifungal drugs have a concentration and a time-dependent action which result in a minimal inhibitory concentration (MIC) that is usually lower than the level required to kill the organism.[6] However, newer agents, such as terbinafine (Lamisil), kill organisms at the level of the MIC.[6]
Pharmacokinetics
Most topical antifungal drugs use the epidermis as a depot. Their greatest concentration is in the stratum corneum, with subsequent distribution through all epidermal layers. Drug concentration in the dermis remains low, and systemic absorption is limited. Absorption may be somewhat greater through the hair follicles, sweat glands and sebaceous glands.[7] Epidermal hydration can increase the absorption rate, especially when an occlusive dressing is used.[7]
The increased lipophilicity of certain drugs and their bases also promotes their bioavailability. Absorption is greater with the water-in-oil cream bases and ointments. However, these antifungal agents are often less well tolerated than other formulations, which may affect patient compliance.
Treatment Options
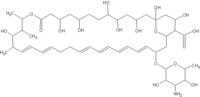
Many antifungal agents are available, with or without a prescription (Table 1),[8] The polyenes, including nystatin (Mycostatin, Mycolog II, Nystex) and amphotericin B (Fungizone), act to increase cell membrane permeability by binding to membrane sterol.[9] Nystatin is both fungicidal and fungistatic. The usual therapeutic target is candidiasis. Vaginitis, which at one time was treated with nystatin, is now treated with the more efficacious azoles.[10] However, nystatin continues to play an important role in the treatment of oral thrush. This agent has limited systemic absorption, and it only occasionally causes nausea, vomiting or diarrhea.[2] Topical formulations, especially the cream, are associated with allergic dermatitis.[2] Amphotericin B, more commonly used as a systemic agent, is also available in topical formulations that are active against Candida organisms and, to a lesser extent, the dermatophytes.[2]
[TABULAR DATA 1 OMITTED]
The imidazoles, including miconazole (Micatin, Monistat. Derm) and clotrimazole (Lotrimin, Mycelex), have similar spectrums of activity and efficacy.[1] They block the synthesis of ergosterol, which is important in cell membrane structure and function. Imidazoles delay cell growth at lower concentrations and inhibit it at the MIC. These agents are fungicidal at five to 10 times the MIC.[1]
Compared with older agents, terconazole (Terazol) has increased potency and a widened spectrum of activity. This triazole also has a decreased side-effect profile.[1]
The newer azoles, including oxiconazole (Oxistat) and sulconazole (Exelderm), remain in the tissues for an extended period. Thus, they may be given in a single daily dose. However, superior results have not been documented for these newer agents.
The allylamines inhibit ergosterol synthesis, specifically squalene epoxidase, thereby altering the structure of the fungal cell wall.[9] Terbinafine and naftifine (Naftin) have an increased lipophilicity that allows them to bind to the stratum corneum layer.[10] Since topical terbinafine persists in tissues for seven days after treatment is stopped, a shortened course may be used.[4] As a primary fungicidal agent, terbinafine has a broad range of activity at lower concentrations.[6] Naftifine has fungicidal action against dermatophytes and Candida species. Its potency is similar to that of tolnaftate (Aftate, NP-27, Tinactin) and clotrimazole.[4] Naftifine also demonstrates an anti-inflammatory effect.[10] The side-effect profiles of both terbinafine and naftifine include about a 2 percent incidence of local burning, pruritus, dryness and erythema.[4]
While tolnaftate has fungicidal activity against dermatophytes, it is not quite as effective as other agents in treating dry Trichophyton rubrum infections and candidiasis. Supplemental nail activity has been documented for the 20 percent urea formulation used in combination with an occlusive dressing. Possible side effects of tolnaftate include contact dermatitis, urticaria, pruritus and erythema. In addition, there have been isolated reports of Stevens-Johnson syndrome and toxic epidermal necrolysis in patients treated with tolnaftate.[2]
Ciclopirox (Loprox) interferes with the uptake and availability of products required for membrane synthesis.[9] This agent also has direct anti-inflammatory actions.[2] The actions of ciclopirox are both fungicidal and fungistatic. A broad range of activity has been demonstrated against dermatophytes, yeast, certain bacteria, and Actinomyces and Eumycetes species.[2] An 8 percent lacquer base penetrates the nails, enhancing the oral treatment of onychomycoses.[2]
Haloprogin (Halotex) is active against dermatophyte infections, candidiasis, pityriasis versicolor and erythrasma.[9] The efficacy of the 1 percent cream resembles that of 2 percent miconazole cream.[2] With haloprogin therapy, local irritation, pruritus and contact dermatitis may occur.[2]
Clioquinol (Vioform) preparations have increased lipid solubility and were once used regularly to treat diaper dermatitis. Since repeated applications may lead to systemic neurotoxic syndromes, however, these preparations should not be used in infants.[2]
Nonspecific Topical Antifungals
Whitfield's ointment, a 12 percent benzoic acid and 6 percent salicylic acid preparation, is fungistatic. Its nonspecific action is keratolytic, producing desquamation. The ointment can be irritating to the skin when it is applied to large surface areas.[2]
Castellani paint, produced from carbolfuchsin, has been used to treat seborrheic eczema and tinea pedis. Its action is antifungal and antibacterial. Gentian violet also has antifungal and antibacterial actions. However, this agent can irritate the skin and stains clothing.[2]
Potassium permanganate has nonspecific activity against Candida species. The compound of undecylenic acid with zinc, calcium and sodium has fungistatic activity.[2] Selenium sulfide has a cytostatic effect on cells. This compound increases fungal shedding by decreasing corneocyte production.
The addition of topical steroids to treatment with an antifungal agent has become popular, but it is controversial. Most studies have included nonspecific diagnoses and have used only one combination product.[11] Other studies involving limited numbers of patients have documented similar results with antifungal agents alone and with the addition of a steroid.[12] Letters and editorials continue to document concern about adverse reactions related to the added topical steroid.[13] The efficacy is questionable, and any clinical benefit appears to be outweighed by the increased risk of side effects.
Choice of Therapy
With the continued introduction of new products, the selection of topical antifungal therapy has become increasingly challenging. Most of the published data provide only limited guidance for product selection. Several studies have compared the use of various antifungal agents in vitro or in animals, and it is difficult to extrapolate the results to patient-care situations. Reports on clinical trials have often noted equivalent results with the newer agents and with miconazole or clotrimazole. To date, no large multicenter study has compared the efficacy of the available antifungal agents.
The newer agent terbinafine has been shown to have a primary fungicidal effect, with lower concentrations required to eradicate an infection. Because this agent remains in tissues for an extended period, a shorter therapeutic course may be used. However, topical superiority for this agent has yet to be demonstrated in a large clinical trial.
A recent article highlighted miconazole as the efficacious, cost-effective agent for most topical mycoses.[14] The cost advantages of the newer antifungal agents have also been recognized, since these agents may be given in a single daily dose or in a shortened therapeutic course.[12] However, the costs of the shortened regimens for vulvovaginitis are similar to the costs of treatment with older agents[5] (Table 2). Studies are needed to evaluate the clinical efficacies and the cost advantages of both alternative and traditional modalities. The dosing regimens and costs (by weight) for currently available prescription and over-the-counter products are provided in Table 3.
[TABULAR DATA 2 & 3 OMITTED]
The author thanks Daniel DePietropaolo, M.D., Judith Fisher, M.D., and James Gill, M.D., of the
Department of Family Medicine at the Medical Center of Delaware, Wilmington, for assistance in the preparation of the manuscript.
REFERENCES
[1.] Ernest JM. Topical antifungal agents. Obstet Gynecol Clin North Am 1992;19:587-607. [2.] Gupta AK, Sauder DN, Shear NH. Antifungal agents: an overview. Part 1. J Am Acad Dermatol 1994;30(5 Pt 1):677-98. [3.] Cohn MS. Superficial fungal infections. Topical and oral treatment of common types. Postgrad Med 1992;91(2):239 44,249-52. [4.] Gupta AK, Sauder DN, Shear NH. Antifungal agents: an overview. Part II. J Am Acad Dermatol 1994;30:911-33. [5.] Sobel JD. Controversial aspects in the management of vulvovaginal candidiasis. J Am Acad Dermatol 1994;31(3 Pt 2):10-3. [6.] Clayton YM. Relevance of broad-spectrum and fungicidal activity of antifungals in the treatment of dermatomycoses. Br J Dermatol 1994;130(Suppl 43):7-8. [7.] Craig CR, Stitzel RE, eds. Modern pharmacology. 2d ed. Boston: Little, Brown, 1986. [8.] American Academy of Family Physicians. Superficial fungal infections/cosmetic dermatology. Home study audio 201. Kansas City, Mo.: American Academy of Family Physicians, 1996:6-7. [9.] Rezabek GH, Friedman AD. Superficial fungal infections of the skin. Diagnosis and current treatment recommendation. Drugs 1992;43:674-82. [10.] Torres-Rodriguez JM. New topical antifungal drugs. Arch Med Res 1993;24:371-5. [11.] Lassus A, Nolting KS, Savopoulos C. Comparison of ciclopirox olamine 1% cream with cidopirox 1%-hydrocortisone acetate 1% cream in the treatment of inflamed superficial mycoses. Clin Ther 1988; 10:594-9 [12.] Reynolds RD, Boiko S, Lucky AW. Exacerbation of hnea corporis during treatment with 1% clotrimazole/0.05% betamethasone diproprionate (Lotrisone) [Letter]. Am J Dis Child 1991;145:1224-5. [13.] Barkey WF. Striae and persistent tinea corporis related to prolonged use of betamethasone dipropionate 0.05% cream/clotrimazole 1% cream (Lotrisone cream) [Letter] J Am Acad Dermatol 1987;11: 518-9. [14.] Chren MM. Costs of therapy for dermatophyte infections. J Am Acad Dermatol 1994;31(3 Pt 2):103-6.
RICHARD W. SLOAN, M.D., R.PH., coordinator of this series, is chairman and residency program director of the Department of Family Medicine at York (Pa.) Hospital and clinical associate professor in family and community medicine at the Milton S. Hershey Medical Center, Pennsylvania State University, Hershey, Pa.
The Authors KRISTINE BURNS DIEHL, M.D., R.PH. is currently in private family practice in Wilmington, Del. She received her pharmacy degree from West Virginia University, Morgantown, where she also earned her medical degree. Dr. Diehl completed a family practice residency at the Medical Center of Delaware, Wilmington.
Address correspondence to Kristine Burns Diehl, M.D., R.Ph., Delaware Family Care Associates, 2700 Silverside Rd., Wilmington, DE 19810.
COPYRIGHT 1996 American Academy of Family Physicians
COPYRIGHT 2004 Gale Group