In patients without established cardiac disease, the occurrence of premature ventricular complexes without sustained ventricular tachycardia is more an annoyance than a medical risk, and treatment is not required. In contrast, patients with established heart disease and premature ventricular complexes have a higher likelihood of developing ventricular tachycardia or fibrillation. These patients should be treated with a beta blocker or class I antiarrhythmic drug. Treatment of arrhythmias in pregnant women is rarely needed. When treatment is required, amiodarone should be avoided, and beta blockers should be used with caution, because these agents have been associated with fetal growth retardation. The most important rhythm abnormality in athletes is ventricular tachycardia associated with hypertrophic cardiomyopathy. If the presence of the disease is confirmed by echocardiography, beta-blocker therapy is necessary, and these patients should be limited to participation in nonstrenuous sports. Acute arrhythmias in children with Wolff-Parkinson-White syndrome can be treated with adenosine. Radiofrequency ablation of the accessory pathway can provide long-term control. (Am Fam Physician 2002;65:2491-6. Copyright[C] 2002 American Academy of Family Physicians.)
Atrial fibrillation, supraventricular tachycardias, and sinus nodal arrhythmias are the rhythm abnormalities most commonly encountered by family physicians. Ventricular ectopy is also common. The management of ventricular ectopy can be troublesome, because some treatments may actually worsen outcomes rather than improve them. Part II of this two-part article reviews the management of ventricular arrhythmias and approaches to rhythm disturbances in selected populations.
Premature Ventricular Complexes
A premature ventricular complex is characterized by the premature occurrence of a QRS complex that is bizarre in shape and lasts longer than 120 msec. The T wave is large and usually of opposite polarity to the QRS complex. A premature ventricular complex is usually followed by a full compensatory pause.
The term "ventricular bigeminy" refers to alternating normal sinus and premature ventricular complexes. Three or more successive premature ventricular complexes are arbitrarily defined as ventricular tachycardia.
Premature ventricular complexes become more prevalent with increasing age and occur in association with a variety of stimuli (Table 1). It is important to determine whether underlying structural heart disease is present and left ventricular function is impaired. Other common causes include electrolyte abnormalities, stimulants, and some medications.
Attempts have been made to estimate the risk of chronic premature ventricular complexes based on their frequency and waveforms. Several studies(1,2) have demonstrated an increased risk for life-threatening arrhythmias with 10 or more ectopic impulses per hour or the presence of impulse salvos (i.e., three to five consecutive impulses). However, structural heart disease and poor left ventricular function are the key factors in determining whether treatment is warranted and what the prognosis may be.
MANAGEMENT
Patients Without Heart Disease. In the absence of heart disease, premature ventricular complexes are associated with little or no increased risk of developing a dangerous arrhythmia. In this situation, the risk-to-benefit ratio of antiarrhythmic drug therapy does not support routine treatment.(3) It is important to review medications, determine if stimulants are being used, and correct electrolyte abnormalities. If no underlying cause is found, the optimal approach is patient reassurance.
Patients should be made aware of the potential dangers of antiarrhythmic drug therapy as determined in the Cardiac Arrhythmia Suppression Trials (CAST and CAST II).(4,5) CAST showed that the risk of dying increased, rather than decreased, with successful long-term suppression of premature ventricular complexes after myocardial infarction in older patients. At best, CAST II showed no impact on long-term survival from drug treatment that successfully suppressed premature ventricular complexes.
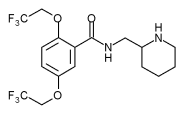
If patients with multiple premature ventricular complexes have severe, disabling symptoms, beta blockers are the safest initial choice. Referral to a cardiologist is indicated if beta-blocker therapy is not effective. In this situation, the next agents to be tried would be class I antiarrhythmic drugs, such as flecainide (Tambocor) and amiodarone (Cordarone), although radiofrequency ablation of an ectopic focus may also be an appropriate treatment.
Patients with Structural Heart Disease. The occurrence of premature ventricular complexes in patients with structural heart disease has been shown to significantly increase the risk of subsequent morbidity and mortality. Coronary heart disease, cardiomyopathy, and congestive heart failure are the major cardiac diseases associated with unfavorable outcomes in patients with premature ventricular complexes.
Ventricular Tachycardia
Ventricular tachycardia refers to a rhythm originating from a ventricular ectopic focus at a rate greater than 100 beats per minute. The electrocardiogram shows a wide-complex tachycardia with no associated P waves.
In patients with bundle branch block, Wolff-Parkinson-White syndrome, or aberrant conduction, supraventricular tachycardia can resemble ventricular tachycardia. Because of the morbidity and mortality associated with untreated ventricular tachycardia, any wide-complex tachycardia should be assumed to be ventricular tachycardia until proved otherwise. Physicians should keep in mind that patients with ventricular tachycardia can have minimal symptoms.
MANAGEMENT
The mortality rate within two years is reported to be higher than 30 percent in patients with nonsustained ventricular tachycardia on Holter monitoring and impaired left ventricular function.(6) Two large multicenter trials(7,8) showed a clear advantage for automatic cardioverter-defibrillator implantation over drug therapy in patients who had a malignant ventricular arrhythmia or who had been resuscitated from sudden cardiac death.
The selection of high-risk patients for defibrillator implantation should be based on left ventricular function and the findings of electrophysiologic studies. Implantable defibrillators appear to be most beneficial in patients with a low ejection fraction who are noted to have frequent premature ventricular complexes, nonsustained ventricular tachycardia on Holter monitoring, and a history of syncope or near-syncope. It is critical to rule out coronary heart disease and to optimize the treatment of congestive heart failure in these patients.
When ventricular tachycardia is diagnosed in relatively asymptomatic patients, medical treatment should be attempted. New recommendations from the American Heart Association(9) emphasize the initial use of 300 mg of intravenously administered amiodarone, followed by repeated 150-mg intravenous doses every eight to 10 minutes, in patients with pulseless ventricular tachycardia. Patients with stable ventricular tachycardia should be given 150 mg of amiodarone intravenously over 10 minutes, followed by an infusion at 1 mg per minute for six hours and then at 0.5 mg per minute until the ventricular tachycardia converts to sinus rhythm or another less dangerous rhythm. The alternative treatment is intravenously administered lidocaine (Xylocaine), given first in a 100-mg bolus (or 1 mg per kg) and then in an infusion at 1 to 4 mg per minute.
In hemodynamically unstable patients, electrical cardioversion should be attempted in accordance with the recently revised advanced cardiac life support (ACLS) protocols.(9)
Automatic implantable cardioverter-defibrillators are considered the most effective treatment for patients with life-threatening ventricular tachycardia or fibrillation. According to expert recommendations, implantation of an automatic cardioverter-defibrillator should be considered in these situations(10): (1) cardiac arrest resulting from ventricular fibrillation or tachycardia not caused by a transient or reversible cause; (2) spontaneous, sustained ventricular tachycardia; (3) syncope of undetermined origin and sustained ventricular tachycardia or fibrillation induced during electrophysiologic studies; and (4) nonsustained ventricular tachycardia with coronary artery disease and left ventricular dysfunction if ventricular tachycardia or fibrillation is induced during electrophysiologic studies.
Treatment of Arrhythmias in Special Populations
PREGNANT WOMEN
The incidence and severity of atrial and ventricular ectopy are reported to increase during pregnancy.(11,12) The reasons remain unclear, although it may be that more frequent contact with health care providers allows greater opportunity for cardiac disturbances to be recognized.
Isolated atrial and ventricular ectopic beats in pregnant women without existing heart disease are usually benign.(13) Increases in atrial extra beats and sustained atrial arrhythmias may be associated with the use of sympathomimetic drugs such as pseudoephedrine.(13) Thus, it is important to inquire about the use of over-the-counter medication in pregnant women who complain about palpitations or extra heartbeats.
Most medications that are safe in nonpregnant patients are safe in pregnant women. Amiodarone is the only antiarrhythmic drug that has been associated with significant fetal abnormalities. In addition to cardiac disturbances, amiodarone can cause fetal goiter, neonatal hypothyroidism, and fetal growth retardation.(14) Based on these observations, amiodarone should not be given to pregnant women. When used for hypertension management during pregnancy, propranolol (Inderal) and atenolol (Tenormin) have been associated with intrauterine growth restriction. These beta blockers can also cause hypoglycemia in the newborn.(15,16)
Most antiarrhythmic drugs are safe for use in lactating women. The exceptions are amiodarone and acebutolol (Sectral). Amiodarone should not be used because it is secreted in breast milk. Acebutolol becomes concentrated in breast milk; therefore, breastfed infants receive a much larger dose than they would with other beta blockers. As a result, these infants may develop neonatal bradycardia or hypoglycemia. If lactating women need a beta blocker, an agent other than acebutolol should be used.(14)
ATHLETES
Well-trained athletes usually have a slow heart rate, with occasional sinus pauses and, frequently, multiple benign escape beats. If no symptoms are present and the sinus pauses last three seconds or less, no further evaluation is necessary.(17) The rhythm changes are caused by increased vagal tone. During exercise, vagal tone is reduced, and appropriate heart rate acceleration occurs. The maximal heart rate is unchanged, although more physical exertion may be required to achieve it.
Malignant ventricular tachycardia, the arrhythmia of most concern in athletes, is usually associated with idiopathic hypertrophic cardiomyopathy. In one series,(18) 48 of 131 athletes who experienced sudden cardiac death were found to have this disease, and another 14 probably had it. Symptoms of syncope or near-syncope with exercise or a family history of sudden cardiac death in a close relative are red flags for the presence of idiopathic hypertrophic cardiomyopathy. Athletes who have an aortic murmur that increases with Valsalva's maneuver should also be evaluated for hypertrophic cardiomyopathy before they are allowed to participate in sports.
When hypertrophic cardiomyopathy is identified, treatment with a beta blocker or calcium channel blocker can reduce cardiac contractility and limit heart rate during exertion. An alternative to pharmacologic management is the insertion of an implantable cardioverter-defibrillator.
Expert panels have recommended that athletes with identified hypertrophic cardiomyopathy be barred from participation in strenuous sports.(19) These persons may participate in low-intensity sports such as bowling, golf, billiards, and cricket.(20) High-performance athletes who have attempted to engage in their sport while taking medications frequently complain of fatigue or diminished performance. Consequently, they may not comply with treatment and thereby increase their risk of sudden cardiac death.
CHILDREN
Supraventricular tachycardias are the most common sustained pathologic arrhythmias in children younger than 12. These arrhythmias are usually caused by an accessory atrioventricular pathway or Wolff-Parkinson-White syndrome.(21)
The same medications are used to treat supraventricular tachycardias in children and adults. Adenosine (Adenocard) in a dose of 100 mcg per kg administered intravenously can usually disrupt the arrhythmia. If the initial dose is not successful, it may be doubled and repeated. For long-term control, radiofrequency ablation is the recommended definitive treatment, with a success rate of 85 to 95 percent when performed by experienced pediatric cardiologists.(22)
Atrial and ventricular extra beats are also common in children. These extra beats are not cause for concern if they resolve with exercise in otherwise healthy children. However, ventricular extra beats are associated with a higher risk of death in children who have existing structural heart disease or cardiomyopathies.(21) These children should be referred for additional evaluation.
PATIENTS WITH ACUTE MYOCARDIAL INFARCTION
Some form of rhythm abnormality is present in 90 percent of patients with acute myocardial infarction.(23) Serious arrhythmias, such as ventricular fibrillation, occur early in the acute phase of myocardial infarction, with the risk declining rapidly after 24 hours. The most common arrhythmias are sinus tachycardia and premature ventricular complexes. Sinus bradycardia often develops in patients with acute inferior infarction. Common arrhythmias in patients with acute myocardial infarction are summarized in Table 2.(24)
Accelerated idioventricular rhythm is defined as a ventricular rhythm with a rate of 60 to 125 beats per minute. This arrhythmia is sometimes called "slow ventricular tachycardia." Accelerated idioventricular rhythm is present in up to 20 percent of patients after an acute myocardial infarction.(25) It occurs with equal frequency in anterior and inferior infarctions and does not usually have a negative impact on hemodynamic status. Accelerated idioventricular rhythm is also common after successful reperfusion with thrombolytics, but it is not considered a reliable indicator of reperfusion. Most episodes are self-limited and do not require treatment.
Premature ventricular complexes do not usually require treatment. However, if premature ventricular complexes and sinus tachycardia are both present, they may be controlled with orally administered beta blockers. Early intravenous administration of these drugs can reduce the incidence of ventricular fibrillation in patients with evolving acute myocardial infarction.(24)
Nonsustained ventricular tachycardia in the immediate peri-infarction period does not appear to be associated with an increased risk of death, and antiarrhythmics have not been shown to have a beneficial effect on morbidity and mortality rates.(26) However, nonsustained ventricular tachycardia occurring after 48 hours in patients with left ventricular dysfunction is a marker for sudden cardiac death. These patients should be observed closely and referred for electrophysiologic studies. Sustained ventricular tachycardia (lasting longer than 30 seconds) is a medical emergency and should be managed in accordance with ACLS protocols.
Atrial fibrillation occurs in 10 to 15 percent of patients with acute myocardial infarction.(24) It is most often associated with larger anterior infarcts and signals an increased risk for stroke, as well as increased mortality.(27)
Sinus bradycardia is particularly common in patients with acute inferior and posterior infarction. If symptoms are present, atropine should be given. First-degree atrioventricular block occurs in 15 percent of patients with acute myocardial infarction and is sometimes exacerbated by medications.(24) No therapeutic measures are necessary in these patients, but monitoring should be continued.
Mobitz type I block (Wenckebach block) occurs when there is ischemia to the atrioventricular node. This arrhythmia is commonly associated with inferior myocardial infarction. It rarely progresses to complete atrioventricular block, and temporary pacing is almost never required. Temporary pacing support is required in most patients with Mobitz type II block or third-degree heart block.
The authors indicate that they do not have any conflicts of interest. Sources of funding: none reported.
Members of various family practice departments develop articles for "Practical Therapeutics." This article is one in a series coordinated by the Department of Family Medicine at the Medical University of South Carolina, Charleston. Guest editor of the series is William J. Hueston, M.D.
This is part 2 of a two-part article on common arrhythmias. Part I, "Supraventricular Arrhythmias," appears on page 2479 in this issue.
A. KESH HEBBAR, M.D., and WILLIAM J. HUESTON, M.D., Medical University of South Carolina, Charleston, South Carolina
REFERENCES
(1.) Schulze RA Jr, Strauss HW, Pitt B. Sudden death in the year following myocardial infarction. Am J Med 1977;62:192-9.
(2.) Bigger JT Jr, Fleiss JL, Kleiger R, Miller JP, Rolnitzky LM. The relationships among ventricular arrhythmias, left ventricular dysfunction, and mortality in the 2 years after myocardial infarction. Circulation 1984;69:250-8.
(3.) Kennedy HL, Whitlock JA, Sprague MK, Kennedy LJ, Buckingham TA, Goldberg RJ. Long-term follow-up of asymptomatic healthy subjects with frequent and complex ventricular ectopy. N Engl J Med 1985;312:193-7.
(4.) Echt DS, Liebson PR, Mitchell LB, Peters RW, Obias-Manno D, Barker AH, et al. Mortality and morbidity in patients receiving encainide, flecainide, or placebo. The Cardiac Arrhythmia Suppression Trial. N Engl J Med 1991;324:781-8.
(5.) Effect of the antiarrhythmic agent moricizine on survival after myocardial infarction. The Cardiac Arrhythmia Suppression Trial II Investigators. N Engl J Med 1992;327:227-33.
(6.) Wilber DJ, Garan H, Finkelstein D, Kelly E, Newell J, McGovern B, et al. Out-of-hospital cardiac arrest. Use of electrophysiologic testing in the prediction of long-term outcome. N Engl J Med 1988;318:19-24.
(7.) Moss AJ, Hall WJ, Cannom DS, Daubert JP, Higgins SL, Klein H, et al. Improved survival with an implanted defibrillator in patients with coronary disease at high risk for ventricular arrhythmia. Multicenter Automatic Defibrillator Implantation Trial Investigators. N Engl J Med 1996;335:1933-40.
(8.) A comparison of antiarrhythmic-drug therapy with implantable defibrillators in patients resuscitated from near-fatal ventricular arrhythmias. The Antiarrhythmics versus Implantable Defibrillators (AVID) Investigators. N Engl J Med 1997;337:1576-83.
(9.) Guidelines 2000 for cardiopulmonary resuscitation and emergency cardiovascular care. An international consensus on science. The American Heart Association in collaboration with the International Liaison Committee on Resuscitation (ILCOR). Circulation 2000;102(8 suppl):I1-370.
(10.) Gregoratos G, Cheitlin MD, Conill A, Epstein AE, Fellows C, Ferguson TB Jr, et al. ACC/AHA guidelines for implantation of cardiac pacemakers and antiarrhythmia devices: executive summary--a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee on Pacemaker Implantation). Circulation 1998;97:1325-35.
(11.) Tawam M, Levine J, Mendelson M, Goldberger J, Dyer A, Kadish A. Effect of pregnancy on paroxysmal supraventricular tachycardia. Am J Cardiol 1993;72:838-40.
(12.) Brodsky M, Doria R, Allen B, Sato D, Thomas G, Sada M. New-onset ventricular tachycardia during pregnancy. Am Heart J 1992; 123(4 pt 1):933-41.
(13.) Chow T, Galvin J, McGovern B. Antiarrhythmic drug therapy in pregnancy and lactation. Am J Cardiol 1998;82(4A):58I-62I.
(14.) Onuigbo M, Alikhan M. Over-the-counter sympathomimetics: a risk factor for cardiac arrhythmias in pregnancy. South Med J 1998;91:1153-5.
(15.) Eliahou HE, Silverberg DS, Reisin E, Romem I, Mashiach S, Serr DM. Propranolol for the treatment of hypertension in pregnancy. Br J Obstet Gynaecol 1978;85:431-6.
(16.) Lydakis C, Lip GY, Beevers M, Beevers DG. Atenolol and fetal growth in pregnancies complicated by hypertension. Am J Hypertens 1999;12:541-7.
(17.) Link MS, Olshansky B, Estes NA 3d. Cardiac arrhythmias and the athlete. Curr Opin Cardiol 1999;14:24-9.
(18.) Maron BJ, Shirani J, Poliac LC, Mathenge R, Roberts WC, Mueller FO. Sudden death in young competitive athletes. Clinical, demographic, and pathological profiles. JAMA 1996;276: 199-204.
(19.) Maron BJ, Isner JM, McKenna WJ. 26th Bethesda conference: recommendations for determining eligibility for competition in athletes with cardiovascular abnormalities. Task Force 3: hypertrophic cardiomyopathy, myocarditis and other myopericardial diseases and mitral valve prolapse. J Am Coll Cardiol 1994;24:880-5.
(20.) Mitchell JH, Haskell WL, Raven PB. Classification of sports. J Am Coll Cardiol 1994;24:864-6.
(21.) Case CL. Diagnosis and treatment of pediatric arrhythmias. Pediatr Clin North Am 1999;46:347-54.
(22.) Danford DA, Kugler JD, Deal B, Case C, Friedman RA, Saul JP, et al. The learning curve for radiofrequency ablation of tachyarrhythmias in pediatric patients. Participating members of the Pediatric Electrophysiology Society. Am J Cardiol 1995;75:587-90.
(23.) Aufderheide TP. Arrhythmias associated with acute myocardial infarction and thrombolysis. Emerg Med Clin North Am 1998; 16:583-600.
(24.) Antman EM, Braunwald E. Acute myocardial infarction. In: Braunwald E, ed. Heart disease: a textbook of cardiovascular medicine. 6th ed. Philadelphia: Saunders, 2001:1114-28.
(25.) Ryan TJ, Anderson JL, Antman EM, Braniff BA, Brooks NH, Califf RM, et al. AHA/ACC guidelines for the management of patients with acute myocardial infarction: executive summary. A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee on Management of Acute Myocardial Infarction). Circulation 1996;94: 2341-50.
(26.) Eldar M, Sievner Z, Goldbourt U, Reicher-Reiss H, Kaplinsky E, Behar S. Primary ventricular tachycardia in acute myocardial infarction: clinical characteristics and mortality. The SPRINT Study Group. Ann Intern Med 1992;117:31-6.
(27.) Goldberg RJ, Seeley D, Becker RC, Brady P, Chen ZY, Osganian V, et al. Impact of atrial fibrillation on the in-hospital and long-term survival of patients with acute myocardial infarction: a community-wide perspective. Am Heart J 1990;119:996-1001.
COPYRIGHT 2002 American Academy of Family Physicians
COPYRIGHT 2002 Gale Group