Although strongly discouraged by many authorities, a significant number of women continue to use prescription medications during pregnancy, placing themselves and their fetuses at risk for adverse outcomes. Studies in Europe have shown that a significant number of pregnant women receive prescription medications that are labeled as potentially harmful to the fetus and a small percentage receive prescriptions for medications that are absolutely contraindicated during pregnancy. Andrade and colleagues performed a retrospective evaluation to determine the use of prescription drugs in pregnant women in the United States.
Researchers studied automated databases from eight health maintenance organizations. Women who delivered an infant in a hospital from January 1, 1996, through December 31, 2000, were identified. To be included in the study, the women had to have participated in a prescription drug plan for at least one year before their delivery date. The gestational period was assumed to begin 270 days before the delivery date with an additional 90-day period before pregnancy included in the analysis. The date that the pregnancy was established in the database was given as the earliest prenatal care visit within 270 days of delivery. Data were excluded if there was no evidence of prenatal care in this period. Information obtained from the database included prescription drugs dispensed and inpatient and outpatient diagnoses and procedures. All medications prescribed during the study were labeled according to the U.S. Food and Drug Administration (FDA) risk classification (A, B, C, D, and X).
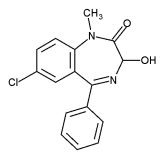
A total of 152,531 deliveries were identified and included in the study. For 64 percent of these deliveries, a drug other than vitamin or mineral supplements was prescribed within the 270 days before delivery; a breakdown by FDA class is given in the accompanying table. After the first prenatal visit, 59 percent of the participants received a drug other than vitamin or mineral supplements, with 3.4 percent receiving a category D medication and 1.1 percent receiving a category X medication. The most common category D medications used, excluding female hormones and ovulation stimulants, included atenolol, secobarbital, doxycycline, lorazepam, and clonazepam. The most common category X medications prescribed, other than female hormones and ovulation stimulants, included temazepam, flurazepam, testosterone, misoprostol, and triazolam. Misoprostol was dispensed in the third trimester and used for cervical ripening exclusively in 12 of 13 women prescribed the drug.
The authors conclude that almost one half of the women in this study received medications that have no evidence of safety during pregnancy or for which evidence shows a risk to the fetus in animals or humans. They add that these results indicate the need to develop and implement systems that eliminate the exposure of pregnant women to these medications.
Andrade SE, et al. Prescription drug use in pregnancy. Am J Obstet Gynecol August 2004;191:398-407.
COPYRIGHT 2005 American Academy of Family Physicians
COPYRIGHT 2005 Gale Group