* EVIDENCE-BASED ANSWER
Adverse reactions to long-term tetracycline therapy are rare, and most will occur within 2 months of initiating therapy (strength of recommendation [SOR]: B, systematic review of ecological studies). Rare but serious drug reactions include a severe cutaneous reaction, hypersensitivity syndrome reaction, serum sickness-like reaction, and isolated single-organ dysfunction (SOR: B, systematic review).
Duration of antibiotic treatment is strongly associated with increased bacterial resistance (SOR: B, systematic review and 1 outcomes study), but antibiotics for acne do not appear to interfere with oral contraceptive efficacy (SOR: B, case-control study and supporting expert opinion). Laboratory monitoring is not indicated in otherwise healthy patients (SOR: B, consistent cohort studies).
No reports have been published regarding long-term topical tretinoin (Retin A) therapy. Short-term follow-up reports note no systemic effects
(SOR: C, expert opinion), no teratogenicity (SOR: B, single case control study), and negligible systemic absorption (SOR: B, outcome studies). Thus, long-term topical tretinoin is presumed to be safe (SOR: C, expert opinion and extrapolation of pharmacologic data).
* EVIDENCE SUMMARY
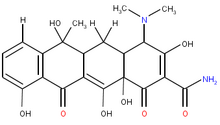
Tetracycline
A study of the safety of tetracycline, (1) which used reports in a drug safety database and a literature review of reported adverse events, concluded that rare but serious events do occur with tetracycline. Severe cutaneous adverse reaction was the most common reported single-organ dysfunction. Other rare events included hypersensitivity syndrome reactions and serum sickness-like reactions.
Since baseline rates of tetracycline use are unknown, it is impossible to ascertain the event rates for these rare reactions. Most of these serious adverse events occur less than 2 months after initiating therapy; they typically include general symptoms such as fever, malaise, and arthralgias, but may also include major organ involvement. The study suggested no clear treatment for these complications, but recommended discontinuing tetracycline and avoiding the entire tetracycline class of drugs. (1) No evidence supports previous concerns that tetracycline causes drug-induced lupus.
A systematic review confirms that treating acne with long-term systemic antibiotics leads to increased antimicrobial resistance. (2,3) A well-designed cohort trial showed that Propioni-bacterium acnes resistance was directly related to duration of antibiotic therapy. (4) This is clinically important because resistance levels correlate with therapeutic failure. (2) Rotating antibiotics on a long-term basis actually increases bacterial resistance patterns and can exacerbate the problems of increasing resistance and poor treatment outcomes. (2)
A relatively large retrospective cohort study of oral contraceptive users in a dermatological practice showed no difference in contraceptive failure rates between those prescribed common antibiotics (including tetracycline) and controls (1.6% vs 0.96%; 95% confidence interval [CI] for the difference, 0.81-2.1). (5)
A systematic review of 8 studies reported on 777 patients taking antibiotics for acne, and examined the need for laboratory monitoring of long-term tetracycline users, including renal, liver, and blood components. The authors found only 1 adverse drug reaction (mild hyperbilirubinemia). They concluded that routine lab monitoring for all patients on long-term antibiotics for acne rarely detects clinically concerning adverse drug reactions and would be cost-prohibitive. (6)
Minor adverse side effects of tetracycline therapy are reported in about 8% of patients. (7) Some of the relatively more common and benign side effects are summarized in Table 1.
Topical tretinoin (Retin A)
Most published studies on topical tretinoin (Retin A) focus on the side effect of minor skin irritation. A multicenter, double-blind parallel study (10) compared the safety and efficacy of 2 formulations of tretinoin gel formulations. Adverse dermatologic side effects commonly reported are in Table 1. These cutaneous irritant side effects, while noted in up to 50% of treated patients, peaked in 7 days and decreased significantly over time.
Topical tretinoin has been in clinical use for more than 25 years. Topical delivery results in a very low systemic exposure; plasma retinoid levels measured after topical use remain at or below endogenous levels, likely due to very limited absorption. (11) Topical tretinoin is not associated with an increased risk for major congenital disorders. A retrospective study of 215 women on tretinoin during the first trimester compared with 430 controls found that the relative risk for a major congenital anomaly was 0.7 (95% CI, 0.2-2.3). The authors concluded that topical tretinoin did not increase congenital anomaly risk. (12)
* RECOMMENDATIONS FROM OTHERS
No clinical guidelines have been published about the long-term use of tetracycline or topical tretinoin. An ad hoc committee of the American Academy of Dermatology concluded "tetracycline is a rational, effective, and relatively safe drug for use in the treatment of acne vulgaris when given in a dosage of 1 gm or less per day for long term therapy." (7) Other experts, more concerned with growing antibiotic resistance, recommend steps to help prevent increasing resistance (Table 2).
* CLINICAL COMMENTARY
Use a judicious approach to topical agents and systemic antibiotics
We should use a judicious approach with appropriate use of topical agents to treat acne. In those cases where acne is not responding, systemic antibiotics can be quite effective and very well tolerated. Regarding antimicrobial resistance of P acnes, we should avoid changing antibiotics unnecessarily, and taper to the lowest effective dose once the acne is well controlled. I think the dictum to avoid treating with systemic antibiotics for longer than 6 months is not widely followed. Often, much longer courses of treatment are necessary. For an individual patient, the risk of developing resistant P acnes is often preferable to the alternatives of inadequate acne control or systemic isotretinoin. Periodic attempts should be made to discontinue antibiotics when acne is well controlled, with resumption of the same antibiotic if one continues to be needed.
Marsha Mertens, MD, Mercy Family Medicine Residency, St. Louis, Mo
REFERENCES
(1.) Shapiro LE, Knowles SR, Shear NH. Comparative safety of tetracycline, minocycline, and doxycycline. Arch Derm 1997; 133:1224-1230.
(2.) Cooper AJ. Systematic review of P acnes resistance to system antibiotics. Med J Australia 1998; 169:259-261.
(3.) Cunliffe WJ. Propionibacterium acnes resistance and its clinical relevance. J Dermatol Treatment 1995; 6:S3-S4.
(4.) Tan HH, Goh CL, Yeo MCG, Tan ML. Antibiotic sensitivity of Propionibacterium acnes isolates from patients with acne vulgaris in a tertiary dermatological referral centre in Singapore. Ann Acad Med Singapore 2001; 30:22-25.
(5.) Helms SE, Bredel DL, Zajic J, Jarjoura D, Brodell RT, Krishnarao I. Oral contraceptive failure rates and oral antibiotics. J Am Acad Dermatol 1997; 36:705-710.
(6.) Driscoll MS, Rothe MJ, Abrahamian L, Grant-Kels JM. Long-term oral antibiotics for acne: is laboratory monitoring necessary? J Am Acad Dermatol 1993; 28:595-602.
(7.) Ad Hoc Committee Report. Systemic antibiotics for treatment of acne vulgaris: efficacy and safety. Arch Dermatol 1975; 111:1630-1636.
(8.) Gilgor RS. Complications of tetracycline therapy for acne. NC Med J 1972; 33:331-333.
(9.) Leyden JJ, Marples RP, Mills Jr OH, Kligman AM. Gram negative folliculitis--a complication of antibiotic therapy in acne vulgaris. Br J Derm 1973; 88:533-538.
(10.) Lucky AW, Cullen SI, Jarratt MT, Quigley JW. Comparative efficacy and safety of two 0.025% tretinoin gels: results from a multicenter, double-blind, parallel study. J Am Acad Dermatol 1998; 38:S17-S23.
(11.) Bershad S, Bersen D, Brodell R, et al. Topical retinoids in the treatment of acne vulgaris. Proceedings of a Roundtable Meeting. Cuds 1999; 64(2S):1-19.
(12.) Jick SS, Terris BZ, Jick H. First trimester topical tretinoin and congenital disorders. Lancet 1993; 341:1181-1182.
Barbara F. Kelly, MD, Martha Burroughs, MS, AHIP, University of Colorado Health Sciences Center, Denver
COPYRIGHT 2004 Dowden Health Media, Inc.
COPYRIGHT 2004 Gale Group