The therapeutic range of serum theophylline concentrations (STCs) is narrow.[1] Theophylline is metabolized by the hepatic cytochrome P448 system;[2] many factors alter its pharmacokinetics,[3-5] and inappropriate concentrations frequently result. Cirrhosis of the liver causes prolongation of the elimination half-life of the theophylline and diminishes protein binding.[6-7] Although moderate social alcohol intake has been postulated to induce hepatic enzymes and shorten elimination half-life,[8] to our knowledge, this has not been investigated. In animal experiments, alcohol enhances theophylline absorption,[9] but this has not been demonstrated to occur in man.[10,11]
To determine if intermittent social alcohol consumption influences STC and potentially impairs accurate monitoring, the effect of a nocturnal dose of alcohol on theophylline pharmacokinetics was investigated.
Methods
Eight normal volunteers, seven men and one woman (mean age, 28 years), were entered into an open, randomized, crossover, placebo-controlled study. All subjects had an average alcohol consumption of less than 20 g of alcohol per day, were nonsmokers, and were taking no medications. The study medication consisted of 0.95 g of alcohol per kilogram (3 ml of whiskey per kilogram) together with 600 ml of mineral water or, alternatively, consisted of an equivalent volume (3 ml/kg) of water (as placebo) plus mineral water; this was consumed between 9 pm and 11 pm the evening prior to each study day. After fasting from midnight, fast-release theophylline (Theolair, 3 Riker St Paul; 125-mg tablets) 5 mg/kg, was taken with 250 ml of water at 9 am. Fasting then continued for a further 4 h. Blood was collected for estimation of STC at 0, 0.5, 1.0, 1.5, 2.0, 2.5, 3.0, 4.0, 6.0, 8.0, 12.0, and 24 h. Assessment of hepatic and renal function was also performed. Subjects received the alternate evening treatment one week later. No other alcohol was allowed for 48 h prior to each study day and caffeine consumption was identical in both 48-h periods and was limited to less than four cups of coffee/tea; none was consumed during the blood sampling period.
Serum theophylline concentrations were determined by the enzyme multiplied immunoassay technique method using a centrifugal fast analyzer.[12] In our laboratory, the assay detection limit is 0.5 mg/L, and the intra-assay coefficient of variation for 10 mg/L is 6 percent. The assayist was blind to the allocation of treatment days, and all samples were assayed in duplicate with corresponding samples from the two study days being assayed in the same batch. Simple pharmacokinetic parameters were derived from the STC data, and the bioavailability for placebo and that for alcohol were assumed to be equal to 1, as demonstrated in previous studies.[10,11,13]
The area under the curve (AUC) for STC (0.24) was derived by digitizing the STC curves and applying a computer program (Prime Systems). The AUC (0, [alpha]) was then derived by extrapolating the log concentration time curve to infinity. The elimination half-life, t1/2, was determined by using least-squares linear regression analysis of the terminal linear portion of the log concentration time curves. Systemic clearance, [Cl.sub.s], was determined by dividing the dose of theophylline by the AUC (0, [alpha]). Since absorption of fast-release theophylline is known to be rapid, it was assumed that the elimination half-life as determined was not influenced by absorption and thus the volume of distribution, Vd, was calculated by dividing [Cl.sub.s] by the elimination rate constant [k.sub.e] (0.7/t1/2). A curve-fitting program (Non lin) was used to generate steady-state data for a dose of 10 mg/kg/d ( mg/kg every 6 h) by using the following equation: steady-state concentration = AUC (0, T)/[tau], where [tau] = dosing interval.[14,15 Simple descriptive statistics were used to obtain the mean and SEM while statistical comparisons were made using one-way analysis of variance followed by Student's paired t test using the computer program SPSS. All subjects gave informed consent, and the study was approved by the hospital ethics committee.
Results
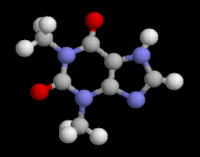
Following alcohol consumption, STCs were greater in each individual at times 6, 8, 12, and 24 h (p<0.01), resulting in a significant difference in the AUC to 24 h and AUC to infinity (Fig 1, Table 1). These differences were primarily attribute to a significant difference in the observed elimination half-life and clearance (Table 1). No significant differences were discernible for maximum serum concentration or time of maximum concentration (Table 1), thereby suggesting that obsorption was rapid and similar on both test days. Following alcohol intake, there was equally no statistically significant difference in volume of distribution (Table 1).
[TABULAR DATA OMITTED]
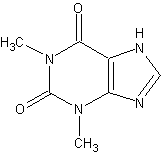
Simulated curves for steady-state fast-release medication are given in Figure 2 and assume a total daily dose of 10 mg/kg/d and 6-h dosing. The simulated mean steady-state data for the placebo day showed a peak-trough difference of 4.2 mg/L, and a similar result was obtained for the alcohol day. However, when comparing the alcohol day with the placebo day, the peak concentration for the simulated mean curve increased by 20 percent. In one individual, the simulated curves showed an increase in peak concentrations of 40 percent (11.0 to 15.4).
There was no significant change in plasma transaminase, alkaline phosphatase, gamma glutamyl transferase (GT), creatinine, or urea values throughout the study. None of the subjects complained of nausea and none experienced any other gastrointestinal symptoms.
Discussion
Alcohol is one of the few "drugs" in our society regularly consumed on an intermittent basis, frequently at night, and rarely in hospital. In this study, following a single episode of moderate nocturnal alcohol consumption, a significant impairment of both elimination half-life and clearance (approximately 33 percent) occurred the next day. Thus, mild-moderate evening alcohol consumption seems likely to cause clinically significant elevations of steady-state serum concentrations; this is supported by the computer-simulated serum concentration time curves and by comparison with drugs such as cimetidine. Cimetidine produces clinically significant elevations of STC by causing an increase in elimination half-life to a degree similar to that seen with alcohol in this study.[16]
The results of this study may have important implications with respect to effective outpatient monitoring of STC. When hospitalized patients return to their normal environments, it is not uncommon for changes to occur in STCs. Previously this has been attributed to changes in diet and improvement in state of health.[17] However, it is feasible in some instances that this may be due to returning to a pattern of intermittent consumption of nocturnal alcohol prior to a daytime assessment of STC. Similarly, some patients monitored in an outpatient setting appear to have considerable variation in plasma concentrations without change in dose; this is usually ascribed to poor compliance, laboratory error, or mistiming of sample collection. In some instances, however, this may also be due to significant alcohol consumption on some evenings but not others.
Serious toxic reactions precipitated by social alcohol consumption seems unlikely to occur unless the patient already has steady-state theophylline concentrations that are almost toxic. However, some of the more distributing side effects of theophylline, such as nausea and vomiting, can occur at very low STCs and interfere with attempts to provide optimal therapy.[18,19] Although patient sensitivity to theophylline toxicity is variable, it is possible some patients may be inadvertently elevating their plasma concentrations by 20 to 40 percent with intermittent alcohol consumption, thereby precipitating side effects.
Other studies have assessed only the effect of alcohol on theophylline absorption and have not shown an effect.[10,11] Similarly in this study, simple inspection of the STC equally suggested that any delayed effect of alcohol ingestion on theophylline absorption is unlikely. Minimization of plasma volume loss from alcohol-induced diuresis and fasting was achieved by giving extra fluid volume during the evening preceding serum theophylline monitoring and presumbly helped to keep the volume of distribution similar on both study days.
Contrary to previous predictions of enhanced hepatic metabolism, it seems likely the increase in half-life detected after even mild-moderate alcohol consumption was predominantly due to impairment of hepatic enzyme systems and seems comparable to the acute effect alcohol has on warfarin metabolism.[20] This effect of alcohol on theophylline metabolism has not been previously reported, and although effects from other components of whiskey cannot be excluded, this would seem unlikely given the known sensitivity of liver function to alcohol exposure. Despite the effects of short-term alcohol intake, it is still likely that regular moderate consumption of alcohol may cause hepatic enzyme induction and neutralize this acute toxic effect. Further studies are required to evaluate this and to determine the duration of the effect of isolated nocturnal alcohol ingestion. The STC at 12 and 24 h appeared to lie on the same linear regression line at the terminal end of the long concentration time curve, indirectly suggesting that the effect may last up to 24 h.
Although further studies are required, the results from this preliminary assessment suggest it may be prudent to advise patients taking regular doses of theophylline either to drink a modest amount of alcohol on a regular basis or not to consume alcohol the night before drug monitoring. Similarly the potential for the combination of alcohol and theophylline to cause increased toxic reactions the following day needs to be considered when evaluating patients with theophylline side effects.
References
[1] Weinberger MM, Bronsky EA. Evaluation of oral bronchodilator therapy in asthmatic children. J Pediatr 1974; 84:421-27 [2] Lohman SM, Miech RP. Theophylline metabolism by the rat liver microsomal system. J Pharmacol Exp Ther 1976; 196:213-25 [3] Riegleman S, Muir K, Upton R. Factors affecting the pharmacokinetics of theophylline. Eur J Respir Dis 1980; 61(suppl 109):67-82 [4] Powell JR, Vozeh S, Hopewell P, Costello J, Sheiner LB, Riegleman S. Theophylline disposition in the acutely ill hospitalized patients: the effect of smoking, heart failure, severe airways obstruction and pneumonia. Am Rev Respir Dis 1978; 118:229-38 [5] Ogilvie RI. Clinical pharmacokinetics of theophylline. Clin Pharmacokinet 1978; 3:267-93 [6] Mangione A, Imhoff TE, Lee RV, Shum LY, Jusko WJ. Pharmacokinetics of theophylline in hepatic disease. Chest 1978; 73:616-22 [7] Piafsky KM, Sitar DS, Rango RE, Ogilvie RI. Theophylline disposition in patients with hepatic cirrhosis. N Engl J Med 1977; 296:1495-97 [8] Jusko WJ, Gardner MJ, Mangione A, Schentag JS, Koup JR, Vance JW. Factors affecting theophylline clearances: age, tobacco, marijuana, cirrhosis, congestive heart failure, obesity, oral contraceptives, benzodiazepines, barbiturates and ethanol. J Pharm Sci 1979; 68: 1358-66 [9] Harrigan DJ, Levy G. Concentration dependence of ethanol effect on intestinal absorption of theophylline in rats. J Pharm Sci 1975; 64:897-88 [10] Powell JR, Voseh S, Hopewell P, Costello J, Sheiner LB. Riegleman S. Theophylline disposition in acutely ill hospitalized patients. The effect of smoking, heart failure, severe airways obstruction and pneumonia. Am Rev Respir Dis 1989; 118:229-38 [11] Sligo JH, Charles BG, Ravenscroft PJ. Oral bioavailability of theophylline from hydroalcoholic and alcohol-free preparations. Med J Aust 1981; 2:410-11 [12] Kampa IS, Dunkoski LK, Jarzabeck JI, Grubesich D. Comparison of three assay procedures for theophylline determination. Their Drug Monit 1979; 1:249-56 [13] Jonkman JHG, Berg WC, Schoenmaker R, Zeeuw RA, Greving JE, Orie NGM. Disposition and clinical pharmacokinetics of microcrystalline theophylline. Eur J Clin Pharmacol 1980: 17:379-84 [14] Rowland M, Tozer TN. Clinical pharmacokinetics: concepts and applications. Philadelphia: Lea & Febiger, 1980 [15] Gibaldi M, Perrier D. Pharmacokinetics. 2nd ed. New York Marcel Decker, 1982 [16] Bauman JH, Kimelblatt BJ, Caraccio TR, Silverman HM, Simon GI, Beck GJ. Cimetidine-theophylline interaction report of four patients. Ann Allergy 1982; 48:100-02 [17] Thompson PJ, Skypala I, Dawson S, McAllister WAC, Turner-Warwick M. The effect of diet upon serum concentrations of theophylline. Br J Clin Pharmacol 1983; 16:267-70 [18] Jacobs MH, Senior RM, Kessler G. Clinical experience with thephylline: relationships between dosage serum concentrations and toxicity. JAMA 1976; 235:1983-86 [19] Svedmyr K. [Beta.sub.2]-Adrenoreceptor stimulants and theophylline in asthma therapy. Eur J Respir Dis 1981; 62(suppl 116):10-1 [20] Breckenridge A, Orme M. Clinical implications of enzyme induction. Ann N Y Acad Sci 1971; 179:421-24
COPYRIGHT 1992 American College of Chest Physicians
COPYRIGHT 2004 Gale Group