Phenothiazine-induced hepatotoxicity,(1,2) including cirrhosis,(3) has been known for many years and has been primarily associated with the use of chlorpromazine. Thioridazine has been reported to cause hepatic injury in six cases.(4-7) Elevations of liver enzymes and jaundice have been the usual presentations of this hepatitis. This paper reports a clinically obvious hepatic dysfunction associated with thioridazine use, which presented with normal bilirubin and liver enzyme levels. CASE REPORT The patient was a 34-year-old schizophrenic male resident of an adult foster care home. He was sent to the clinic by the director of the home with the complaint that he was repeatedly falling asleep while smoking. The patient could not give a reliable history, and no records were available except those from the adult foster care home.
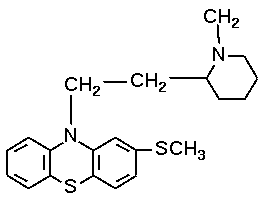
The patient reported having been treated with chlorpromazine in the past, but was switched to thioridazine about 2 years ago because chlorpromazine was too sedating. He currently was taking 200 mg of thioridazine twice daily.
The patient reported that he has had the problem of falling asleep for about 1 year. He also reported a weight gain of approximately 100 lb during the last year. The patient denied any history of hepatitis or other serious illness. The patient denied alcohol abuse. No other history was available.
Physical examination revealed an obese man with a protruberant abdomen who was in no apparent distress. He was cooperative and pleasant during the examination. His blood pressure was 110/80 mm Hg, temperature 37.0'C 98.4'F), and weight 292 lb.
Examination of the chest was within normal limits. The examination of the abdomen revealed tense ascites with a liver span of 20 cm by percussion. The liver margin was smooth, firm, and nontender. There was minimal pitting edema of the ankles.
Laboratory results at the first visit included hemoglobin 172 g/L (17.2 g/dL), hematocrit 0.52, white cell count 8.8 x 109/L (8.8 x 10 .sub.3/(micro)L) with a normal differential, albumin 39 g/L (3.9 g/dL), alkaline phosphatase 1.6 (micro)kat/L (94 IU/L) normal 0. 8 to 2.3 (micro)kat/L, 50 to 136 IU/L), asparate aminotransferase (AST) 0.57 (micro)kat/L (34 IU/L) normal 0.20 to 0.75 (micro)kat/L, 12 to 45 IU/L), alanine aminotransferase (ALT) 0.78 (micro)kat/L (47 IU/L) (normal 0. 12 to 0.66 (micro)kat/L, 7 to 40 IU/L), creatinine 88.40 (micro)mol/L (1.0 mg/ dL), sodium 140 mmoUL (mEq/L), and potassium 4.5 mmot/L mEq/L). Screening tests for hepatitis A and B were negative.
The diagnosis of hepatic failure was made on clinical grounds before the laboratory results were available. The thioridazine was discontinued, and haloperidol, 10 mg three times a day, was substituted because of its low hepatotoxicity." A low dose of spironolactone, 25 mg twice a day, was given for the ascites.
The patient was seen I week later. At that time the supervisor of the adult foster care home reported that the problem of falling asleep while smoking had resolved. The patient's weight had decreased 12 lb (to 280 lb). The pedal edema had disappeared, and the ascites, while still present, was no longer tense. At that visit, the liver span was again found to be 20 cm by percussion.
The patient was seen again after I more week. At that time the patient weighed 281 lb. Percussion of the liver revealed that it had decreased in size to 16 cm. Ascites was not apparent. The patient was continued on the spironolactone at 25 mg twice a day, and the haloperidol dose was decreased to 10 mg twice a day. An ultrasound of the liver was then ordered, which revealed "complete loss of the normal internal echo architecture of the liver. No ascites was seen on ultrasound.
On follow-up 1 month after the first visit, the patient weighed 280 lb, and no ascites was apparent on examination. The spironolactone was discontinued, and the haloperidol continued at the dose of 10 mg twice a day. Two months later he remained asymptomatic with no recurrence of the signs of liver failure. DISCUSSION This case appears to represent thiofidazine-induced hepatotoxicity. Hepatomegally, ascites, and peripheral edema were seen, which resolved when the thioridazine was discontinued. Significant changes in liver architecture were also noted on ultrasound. Significantly, bilirubin, alkaline phosphatase, and AST levels were all normal, and ALT was only slightly elevated. Symptomatic liver failure with normal liver function studies has not been previously reported with thioridazine use.
Hepatic injury associated with thioridazine use has been reported in six previous cases in the literature; three had clinically significant hepatitis and three had only biochemical evidence of hepatic involvement. Weiden and Bruckner(4) reported a case of severe hepatitis associated with thioridazine use that progressed to hepatic encephalopathy. Block5 reported a case of an elderly woman who developed hyperbilirubinemia and elevated liver enzymes after thioridazine administration. Brunold(6) reported a case of jaundice. Reinhart et al(7) reported three cases of patients with biochemical evidence of hepatitis, but no clinical evidence of hepatic disease: the first had hyperbilirubinemia and increases in liver enzymes; the second patient had increases in liver enzymes but normal bilirubin levels; the third patient experienced only elevations in the level of ALT. In each of the reported cases, withdrawal of the medication was associated with resolution of the clinical symptoms and return of normal liver function studies. No pathological studies of the effects of thioridazine on the liver have been published.
Chlorpromazine is well known to cause cholestatic jaundice and hepatocellular injury. (1-3) Thioridazine, on the other hand, appears to cause liver damage only rarely, with only three clinically significant cases previously reported in the literature. Withdrawal of the medication led to resolution of the clinical findings, and no long-term sequelae have been reported. The reputation of thioridazine as a relatively safe antipsychotic medication appears to be justified, based on this review of the literature and the present case. Physicians who care for schizophrenic patients should be aware, however, that hepatotoxicity is a known complication of treatment with any phenothiazine, and they should include a careful physical examination of the liver in their routine care of these patients. References 1, Ishak KG, Irey NS: Hepatic injury associated with the phenothiazines.
Arch Pathol 1972; 93:283-304 2. Dickes R, Schenker V, Deutsch L: Serial liver-function and blood
studies in patients receiving chlorpromazine. N Engl J Med 1957;
256:1-7 3. Walker CO, Combes B: Biliary cirrhosis induced by chlorpromazine.
Gastroenterology 1966; 51:631-640 4. Weiden PL, Bruckner CD: Thioridazine toxicity, agranulocytosis and
hepatitis with encephalopathy. JAMA 1973; 224:518-520 5. Block SL: Jaundice following thioridazine administration. Am J Psychol
1962; 119:77 6. Brunold H: [Experiences with a new phenothiazine derivative, Mel - laril, Sandoz]. Ther Umsch 1959; 16:90-92 7. Reinhad MJ, Benson RM, Kwass SK, Storey WF: Suggestive evidence
of hepatotoxicity concomitant with thioridazine hydrochloride
use. JAMA 1967; 197:767-769 8. Munyon WH, Salo R, Briones DF: Cytotoxic effects of neuroleptic
drugs. Psychopharmacology 1987; 91:182-188
COPYRIGHT 1990 Dowden Health Media, Inc.
COPYRIGHT 2004 Gale Group