We tested the hypothesis that collapsed alveoli opened by a recruitment maneuver would be unstable or recollapse without adequate positive end-expiratory pressure (PEEP) after recruitment. Surfactant deactivation was induced in pigs by Tween instillation. An in vivo microscope was placed on a lung area with significant atelectasis and the following parameters measured: (1) the number of alveoli per field and (2) alveolar stability (i.e., the change in alveolar size from peak inspiration to end expiration). We previously demonstrated that unstable alveoli cause lung injury. A recruitment maneuver (peak pressure = 45 cm H2O, PEEP = 35 cm H2O for 1 minute) was applied and alveolar number and stability were measured. Pigs were then separated into two groups with standard ventilation plus (1) 5 PEEP or (2) 10 PEEP and alveolar number and stability were again measured. The recruitment maneuver opened a significant number of alveoli, which were stable during the recruitment maneuver. Although both 5 PEEP and 10 PEEP after recruitment demonstrated improved oxygenation, alveoli ventilated with 10 PEEP were stable, whereas alveoli ventilated with 5 PEEP showed significant instability. This suggests recruitment followed by inadequate PEEP permits unstable alveoli and may result in ventilator-induced lung injury despite improved oxygenation.
Keywords: acute respiratory distress syndrome; alveolar mechanics; in vivo microscopy; recruitment maneuver; ventilator-induced lung injury
Although the lung recruitment maneuver (RM) has been the subject of much investigation over the last two decades, its use has become much more prevalent of late for treatment of patients with acute lung injury (ALI) and acute respiratory distress syndrome (ARDS) (1-4). Among the pathologic features of ARDS/ALI is the loss and dysfunction of surfactant, subjecting alveoli to increased surface tension and alveolar collapse with resulting hypoxcmia (5, 6). One current ventilator strategy for patients with ARDS/ALI includes an "open lung" approach. This approach consists of an RM with high sustained airway pressures to open atelectatic alveoli followed by application of positive end-expiratory pressure (PEEP) to maintain alveolar patency. This approach was among the interventions performed in a study that showed an improvement in oxygenation and reduced mortality in patients with ARDS (7). Although the postulated mechanism responsible for an RM-induced improvement in oxygenation is recruitment and stabilization of collapsed lung regions (8, 9), this has never been demonstrated at the alveolar level. At present, the effect of an RM on alveolar size, number, and stability is unknown.
Using a unique in vivo microscopic technique developed in our laboratory, we are able to view alveoli in the living animal in real time during mechanical ventilation. We previously described a continuum of alveolar mechanics in the healthy and injured lung, and demonstrated that normal sub-pleural alveoli in healthy lungs do not change area appreciably during tidal ventilation (10). We refer to these as "stable" alveoli (see in vivo microscopic footage demonstrating normal alveoli in the online supplement; video clip E1). However, alveoli in an acutely injured lung develop a complex, heterogeneous inflation pattern, with some alveoli becoming hyperinflated, some remaining totally atelectatic and not participating in ventilation, and some developing instability with partial or total recruitment and derecruitment with tidal ventilation. We have termed this abnormal alveolar behavior repetitive alveolar collapse and expansion, or RACE (10). RACE has been a suspected mechanism of lung injury in infants with respiratory distress syndrome (11), has been shown to produce histologic evidence of ventilator-induced lung injury (VILI) (12), and inhibits hypoxic pulmonary vasoconstriction (HPV) (13). Further, the addition of PEEP in the presence of these abnormal mechanics (RACE) has been shown to stabilize and protect these alveoli from VILI (14).
In this study, we hypothesized that collapsed alveoli in a surfactant deactivation model of acute lung injury could be recruited with a clinically applicable RM, but that these newly recruited alveoli would be unstable (RACE). We further postulate that the addition of sufficient PEEP will stabilize alveoli and prevent RACE. Using in vivo microscopy in a surfactant deactivation model of ARDS, we measured alveolar number and stability before, during, and after RM with ventilation after the RM with either lower (5 cm H2O) or elevated (10 cm H2O) PEEP.
METHODS
Yorkshire pigs (25-35 kg; n = 8) were pretreated with glycopyrrolate (0.01 mg/kg, intramuscular), Telazol (tiletamine hydrochloride and zolazepam hydrochloride [5 mg/kl, intramuscular]), and xylazine (2 mg/kg, intramuscular). Pentobarbital (6 mg/kg per hour) was delivered intravenously by Harvard infusion pump (model 907; Harvard Apparatus, Holliston, MA) for anesthesia. Animals were ventilated with a Galileo ventilator (Hamilton Medical, Reno, NV) with 100% oxygen. Baseline ventilator settings were as follows: tidal volume, 12 cm^sup 3^/kg; PEEP, 5 cm H2O; inspiration-to-expiration ratio, 1:2; and respiratory rate, 15 breaths/minute. Tidal volume and inspiration-to-expiration ratio were unchanged throughout the protocol, and respiratory rate was adjusted to maintain arterial carbon dioxide (Pa^sub CO^sub 2^^) between 35 and 45 cm H2O. Left carotid artery and right internal jugular vein catheters were placed for hemodynamic monitoring and blood sampling, and a right femoral vein Swan-Ganz catheter was placed for cardiac output and filling pressures. ECG monitoring was measured with a pacemaker/defibrillator (Zoll Medical, Burlington, MA).
Surfactant Deactivation
Surfactant deactivation by endotracheal lavage with Tween 20 has been described previously (10, 14), and additional details arc provided in the online supplement.
In Vivo Microscopy
A right thoracotomy was performed with removal of Ribs 5-7 to expose the lung for in vivo microscope placement. Our technique for in vivo microscopy has been described in detail elsewhere (15). Briefly, the in vivo microscope was placed on the visceral pleura of the right lung diaphragmatic lobe. The microscopic images were viewed with a video camera (CCD SSC-S20; Sony, Tokyo, Japan), recorded with a Super VHS video recorder (SVO-9500 MD; Sony), and analyzed with a computerized image analysis system (Image-Pro; Media Cybernetics, Carlsbad, CA).
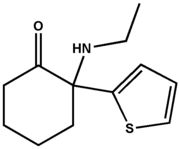
Still images of alveoli were extracted from video at peak inspiration and end expiration and alveolar areas at both peak inspiration and end expiration were measured by computer image analysis (Figure 1). Alveolar stability was expressed as the dynamic change in alveolar area between inspiration and expiration (I-E[Delta]; with higher values for I-E[Delta] representative of worse alveolar instability and lower values for I-E[Delta] representative of more stable alveoli) and was calculated on a standard data spread sheet (Excel; Microsoft, Redmond, WA). The numbers of alveoli were also counted per microscopic field as an index of atelectasis.
Protocol
After surgical preparation and Tween instillation, the in vivo microscope was positioned on the pleural surface and video of subpleural alveoli was recorded during baseline ventilation before RM. RM was then performed, consisting of a peak pressure of 45 cm H2O with a PEEP of 35 cm H2O sustained for 1 minute with continuous video recorded. After RM, animals were divided into two groups, PEEP 5 After RM (5 cm H2O; n = 4) and PEEP 10 After RM (10 cm H2O; n = 4), and ventilation was resumed. Video was again recorded during tidal ventilation tor both groups, with images captured to assess I-E[Delta] and number of alveoli per microscopic field. Additional methods and samples of the in vivo microscopic video are available in the online supplement (see video clips E1-E4).
Statistics
All values are reported as means + or - SEM. Significant differences between groups were determined by one-way analysis of variance and within groups by repeat analysis of variance. Whenever the F ratio indicated significance, a Newman-Keul test was used to identify individual differences. Significance was assumed if the probability of the null hypothesis is less than 5% (p
RESULTS
Before RM in the surfactant-deactivated lung, significant atelectasis is present as indicated by the low number of alveoli per microscopic field (Figure 2A and Table 1). However, the few patent alveoli before RM are stable during tidal ventilation as indicated by the minimal change in area between peak inspiration and end expiration (low I-E[Delta]; see Figure 3 [Before RM] and Table 1). As anticipated, the number of alveoli per microscopic field increased significantly with the recruitment maneuver (Before RM = 2.5 + or - 1.5 alveoli per field versus During RM = 16.5 + or - 1.6 alveoli per field; p
Hemodynamic and pulmonary data are reported in Table 2. RM successfully improved oxygenation regardless of PEEP level after RM (Before RM = 91.4 + or - 1.5% saturation versus PEEP 5 After RM = 98.7 + or - 0.1% saturation; Before RM = 91.4 + or - 1.5% saturation versus PEEP 10 After RM = 97.9 + or - 1.2% saturation; p
DISCUSSION
The most important findings in this study are that alveoli opened with an RM may collapse without adequate PEEP, and many recruited alveoli that do not collapse are unstable (RACE). These unstable alveoli are therefore vulnerable to the shear stress-induced damage believed to be a major cause of ventilator-induced lung injury (VILI) (14, 16, 17). Therefore, although it may improve arterial oxygenation, an RM followed by inadequate PEEP could potentially exacerbate VILI.
Relationship among Alveolar Recruitment, Stability, and Po^sub 2^
There is a current debate as to whether a recruitment maneuver actually opens atelectatic alveoli, or merely distends already patent airspaces (18). Investigations using computerized tomography (CT scan) have equated "successful" recruitment with a decrease in lung tissue density (8, 19), but the resolution of a clinical CT scan is unable to show recruitment at the alveolar level, nor can it image the dynamic behavior of these recruited alveoli (i.e., stable or unstable) during ventilation. Other methods for assessing lung volumes and recruitment, such as plethysmography, are at a similar disadvantage and have been criticized as unable to differentiate true lung volume improvements from pressure-dependent blood shift from the thoracic cavity to the periphery due to elevations in PEEP (20). To our knowledge, the present study is the first to (1) provide direct evidence that alveoli open after an RM, (2) visualize the dynamic behavior of newly recruited alveoli during ventilation, and (3) highlight the fact that, despite "successful" recruitment of alveoli with an RM, without adequate PEEP after RM, alveoli are unstable and therefore susceptible to recruitment-/ derecruitment-induced injury.
Without the benefit of in vivo microscopic observations, "successful" recruitment is currently assessed by several different bedside parameters. Improvement in oxygen saturation is routinely used as a measure of "successful" recruitment (7, 21-26). Reduction in intrapulmonary shunt is also typically used to evaluate improvement after RM (23, 26). Using oxygenation and shunt as a yardstick, both the lower PEEP (PEEP 5 After RM) and higher PEEP (PEEP 10 After RM) groups demonstrated "successful" recruitment. The fact that oxygen saturation and intrapulmonary shunt improved in both groups after RM does not allow differentiation between these two PEEP levels at the bedside on the basis of these physiologic parameters. However, as the data regarding instability suggest, there is marked protection in terms of stabilizing alveoli during ventilation in the high-PEEP group. This highlights the disturbing fact that, although the oxygenation may be transiently improved, suggestive of "successful" recruitment, the risk of VILI is increased without adequate alveolar stabilization with PEEP.
In addition, improvements in oxygenation after an RM appear transient, with repeated RMs necessary to maintain oxygen saturation (27). It appears that insufficient levels of PEEP after RM allow collapse of recruited alveoli (28, 29). In a saline lavage model of acute lung injury, Rimensberger and coworkers demonstrated that elevated PEEP after an RM maintained improvements in Pa^sub O^sup 2^^ (30). This is consistent with the findings in the present study, and suggests that the transient nature of oxygenation improvement after RM may be remedied at least in part by increased PEEP after RM in an effort to reduce RACE or alveolar collapse.
Negative Impact of RM and PEEP on Alveoli
One of the foremost concerns voiced with elevation of airway pressure (RM and/or PEEP) is the potential for alveolar injury by overdistension. One of the hallmarks of ARDS is the heterogeneous nature of the injury, with injured areas directly adjacent to areas of healthy lung (5, 31, 32). Theoretically, ventilation would be delivered preferentially to unaffected normal lung regions with higher compliance, resulting in alveolar overdistension and possible injury (33, 34). High inspiratory plateau pressures have been shown to produce lung injury (35-38), and noninvasive assessments of alveolar overdistension by CT scan (39-41) and pressure-volume curve analysis (42) have been used to direct mechanical ventilation in an attempt to limit overdistension-induced alveolar injury. In the present study, elevated PEEP (PEEP 10 After RM) caused a significant increase in peak inspiratory and end-expiratory alveolar areas as compared with before RM and low PEEP (PEEP 5 After RM) (Table 1). Thus, this study confirmed that increasing PEEP in the acutely injured lung causes a significant increase in peak inspiratory alveolar size in the living animal. It remains to be seen whether this increase in size is pathologic (i.e., alveolar overdistension). In contrast, we have previously demonstrated that alveolar overdistension is not seen in the normal lung (14). This study was not designed to determine what increase in peak inspiratory area represents pathologic overdistension, which may ultimately result in VILI. Furthermore, we are unable to comment on alveolar dimensions in the regions of the lung we are unable to visualize with our in vivo microscope, which may be undergoing even more dramatic distension at peak inspiration. Further investigation is necessary to determine the relationship among the increase in alveolar size at both peak and end ventilation and alveolar instability (RACE) to alveolar injury and VILI.
Recruitment Maneuver Pros and Cons
Previous studies using open lung techniques have shown efficacy in both animal (43) and clinical studies (21, 23). In a clinical study of 15 patients with ARDS, Richard and coworkers (28) demonstrated upward shifts of successive pressure-volume curves performed before and after RM, suggesting recruitment of new lung regions, and correlated this with improvements in oxygen saturation. They went on to show that addition of PEEP further augmented recruitment with corresponding improvements in oxygenation (28). To this end, the recommendations of the American-European Consensus Conference on ARDS include volume recruitment with increased PEEP followed by elevated PEEP to maintain alveolar patency and oxygenation (44).
It has been suggested, but as yet unsupported, that ateleclasis in the presence of ARDS is a self-imposed protective mechanism that limits alveolar damage due to continued recruitment/derecruitment (45). This led to the ventilatory strategy of "lung rest" with low airway pressures to prevent recruitment/derecruitment. The "lung rest" strategy, utilizing lower set tidal volumes, has been employed in several different techniques. "Biologically variable" ventilation, in which tidal volume and rate are varied by computer in the region of a set low mean tidal volume, has shown improvement in Pa^sub O^^sub 2^ at lower peak airway pressures, reduced inflammatory cytokines, and pulmonary edema (46-49). However, it remains to be seen whether this application of variable low tidal volume ventilation truly "rests" atelectatic regions or rather intermittently reopens these regions, subjecting them to possible repetitive recruitment/derecruitment. In patients with severe ARDS, low-volume pressure-limited ventilation with minimal sedation to allow spontaneous breathing has shown improvement in mortality with substantial permissive hypercapnia (50). Although "lung rest" with low airway pressures and atelectasis tolerance appears to be at the opposite end of the ventilation spectrum from "open lung" with higher sustained airway pressures and atelectasis avoidance, the intention of both strategies is the prevention of repetitive opening and closing of alveoli, or RACE. The fact that both of these disparate strategies have resulted in clinically measurable improvements suggests that RACE plays a significant role in the development of VILI. It remains to be established whether lung pathology and outcomes are improved more by tolerance (lung rest) or avoidance (open lung) of atelectasis, and results of this comparison in prospective studies will undoubtedly have tremendous clinical value.
Critique of Methods
Detailed critiques of this methodology have been published previously in several articles (10, 15, 51). Briefly, the suction used to stabilize the microscopic field has been shown to contribute only a slight underestimation of alveolar area change during tidal ventilation (51). Also, subpleural structures have been identified as true alveoli by electron microscopy (51) and alveoli are morphologically distinct from the visceral pleura such that pleural expansion/contraction does not impact the change in alveolar size (15). This in vivo microscopic technique allows measurements of alveoli only in two dimensions, producing an alveolar cross-sectional area on which all calculations of inspiratory and expiratory area changes are calculated (that is, I-E[Delta]). Changes in alveolar depth during ventilation cannot be determined because of the shallow depth of field of the microscope. Although we are unable to comment on the change in alveolar depth and thus cannot identify an absolute volume change for an individual alveolus during tidal ventilation, we can identify and quantify normal and abnormal alveolar mechanics in two dimensions. Certainly, even in two dimensions, the behavior of alveoli in normal and surfactant-deactivated lung is profoundly different, and so the concept of RACE as injurious to the lung appears valid despite our inability to measure change in alveolar size along the z axis. In addition, this in vivo microscopic technique does not provide us with a global measure of alveolar recruitment and mechanics, but rather we are restricted to our microscopic field. Lung injury in clinical ARDS as well as the surfactant deactivation model of ARDS, is heterogeneous in nature, with areas of normal alveolar behavior adjacent to areas of abnormal alveolar mechanics. The intent of the present study was to examine the effects of RM and PEEP on lung areas demonstrating abnormal alveolar mechanics, as it has been previously demonstrated that alveoli with normal mechanics do not change size appreciably with mechanical ventilation (10).
The use of the in vivo microscope to observe alveolar mechanics requires an open chest. Although this is a departure from the clinical scenario of a patient with ARDS undergoing mechanical ventilation, several clinical studies have shown that chest wall compliance does not influence the shape of the pressure-volume curve (52-54), suggesting the open chest wall may be of negligible consequence in the "recruitability" of the lung in the present study. Furthermore, the present study was performed on the non-dependent lung. It has been demonstrated that nondependent lung regions recruit at lower peak pressures than those required to recruit the dependent lung regions (8, 55). With this in mind, the incremental increase in PEEP after RM in the high-PEEP group in the present study (PEEP 10 After RM) may not provide the same degree of stabilization of RACE in the dependent lung. We are currently imaging dependent portions of lung, and the behavior of alveoli under these conditions is being investigated.
CONCLUSION
As the recruitment maneuver and the "open lung" approach become more prevalent in the care of patients with ARDS/ALI, further investigation is required to identify the "optimal" PEEP after recruitment. Reopening of collapsed lung regions for the sake of improved oxygenation in patients with ARDS presents obvious clinical value; however, it is not without potential negative consequences. Failure to maintain patency with adequate PEEP may transiently improve oxygenation at the cost of exacerbated lung injury caused by alveolar recruitment/derecruitment. In addition, elevated levels of PEEP to stabilize alveoli with the resultant potential to produce lung injury by overdistension require further investigation.
Acknowledgment: The authors thank Kathy Snyder and Andrew Paskanik for expert technical assistance.
References
1. Corbridge TC, Wood LD, Crawford GP, Chudoba MJ, Yanos J, Sznajder JI. Adverse effects of large tidal volume and low PEEP in canine acid aspiration. Am Rev Respir Dis 1990;142:311-315.
2. Smith JC, Stamenovic D. Surface forces in lungs: I. Alveolar surface tension-lung volume relationships. J Appl Physiol 1986;60:1341-1350.
3. Stamenovic D, Smith JC. Surface forces in lungs: III. Alveolar surface tension and elastic properties of lung parenchyma. J Appl Physiol 1986;60:1358-1362.
4. Stamenovic D, Smith JC. Surface forces in lungs: II. Microstructural mechanics and lung stability. J Appl Physiol 1986;60:1351-1357.
5. Ashbaugh DG, Bigelow DB, Petty TL, Levine BE. Acute respiratory distress in adults. Lancet 1967;2:319-323.
6. Rinaldo JE, Christman JW. Mechanisms and mediators of the adult respiratory distress syndrome. Clin Chest Med 1990;11:621-632.
7. Amato MB, Barbas CS, Medeiros DM, Magaldi RB, Schettino GP, Lorenzi-Filho G, Kairalla RA, Deheinzelin D, Munoz C, Oliveira R, Takagaki TY, Carvalho CR. Effect of a protective-ventilation strategy on mortality in the acute respiratory distress syndrome. N Engl J Med 1998;338:347-354.
8. Crotti S, Mascheroni D, Caironi P, Pelosi P, Ronzoni G, Mondino M, Marini JJ, Gattinoni L. Recruitment and derecruitment during acute respiratory failure: a clinical study. Am J Respir Crit Care Med 2001;164:131-140.
9. Pelosi P, Goldner M, McKibben A, Adams A, Eccher G, Caironi P, Losappio S, Gattinoni L, Marini JJ. Recruitment and derecruitment during acute respiratory failure: an experimental study. Am J Respir Crit Care Med 2001;164:122-130.
10. Schiller HJ, McCann UG II, Carney DE, Gatto LA, Steinberg JM, Nieman GF. Altered alveolar mechanics in the acutely injured lung. Crit Care Med 2001;29:1049-1055.
11. Robertson B, Van Golde L, Batenburg JJ. Pulmonary surfactant. Amsterdam: Elsevier; 1984.
12. Muscedere JG, Mullen JB, Gan K, Slutsky AS. Tidal ventilation at low airway pressures can augment lung injury. Am J Respir Crit Care Med 1994;149:1327-1334.
13. McCann UG II, Schiller HJ, Gatto LA, Steinberg JM, Carney DE, Nieman GF. Alveolar mechanics alter hypoxic pulmonary vasonconstriction. Crit Care Med 2002;30:1394-1395.
14. McCann UG II, Schiller HJ, Carney DE, Galto LA, Steinberg JM, Nieman GF. Visual validation of the mechanical stabilizing effects of positive end-expiratory pressure at the alveolar level. J Surg Res 2001;99:335-342.
15. Carney DE, Bredenberg CE, Schiller HJ, Picone AL, McCann UG, Gatto LA, Bailey G, Fillinger M, Nieman GF. The mechanism of lung volume change during mechanical ventilation. Am J Respir Crit Care Med 1999;160:1697-1702.
16. Marini JJ. Evolving concepts in the ventilatory management of acute respiratory distress syndrome. Clin Chest Med 1996;17:555-575.
17. Dreyfuss D, Saumon G. Ventilator-induced lung injury: lessons from experimental studies. Am J Respir Crit Care Med 1998;157:294-323.
18. Suter PM. Let us recruit the lung and keep an open mind. Intensive Care Med 2000;26:491-492.
19. Puybasset L, Cluzel P, Gusman P, Grenier P, Preteux F, Rouby JJ. Regional distribution of gas and tissue in acute respiratory distress syndrome: I. Consequences for lung morphology. CT Scan ARDS Study Group. Intensive Care Med 2000;26:857-869.
20. Aliverti A, Dellaca R, Pelosi P, Chiumello D, Pedotti A, Gattinoni L. Optoelectronic plethysmography in intensive care patients. Am J Respir Crit Care Med 2000;161:1546-1552.
21. Amato MB, Barbas CS, Medeiros DM, Schettino Gde P, Lorenzi Filho G, Kairalla RA, Deheinzelin D, Morais C, Fernandes Ede O, Takagaki TY, et al. Beneficial effects of the "open lung approach" with low distending pressures in acute respiratory distress syndrome. A prospective randomized study on mechanical ventilation. Am J Respir Crit Care Med 1995;152:1835-1846.
22. Brunet F, Jeanbourquin D, Monchi M, Mira JP, Fierobe L, Armaganidis A, Renaud B, Belghith M, Nouira S, Dhainaut JF, et al. Should mechanical ventilation be optimized to blood gases, lung mechanics, or thoracic CT scan? Am J Respir Crit Care Med 1995;152:524-530.
23. Foti G, Cereda M, Sparacino ME, De Marchi L, Villa F, Pesenti A. Effects of periodic lung recruitment maneuvers on gas exchange and respiratory mechanics in mechanically ventilated acute respiratory distress syndrome (ARDS) patients. Intensive Care Med 2000;26:501-507.
24. Cakar N, der Kloot TV, Youngblood M, Adams A, Nahum A. Oxygenation response to a recruitment maneuver during supine and prone positions in an oleic acid-induced lung injury model. Am J Respir Crit Care Med 2000;161:1949-1956.
25. Lapinsky SE, Aubin M, Mehta S, Boiteau P, Slutsky AS. Safety and efficacy of a sustained inflation for alveolar recruitment in adults with respiratory failure. Intensive Care Med 1999;25:1297-1301.
26. Pelosi P, Cadringher P, Bottino N, Panigada M, Carrieri F, Riva E, Lissoni A, Gattinoni L. Sigh in acute respiratory distress syndrome. Am J Respir Crit Care Med 1999;159:872-880.
27. Fujino Y, Goddon S, Dolhnikoff M, Hess D, Amato MB, Kacmarek RM. Repetitive high-pressure recruitment maneuvers required to maximally recruit lung in a sheep model of acute respiratory distress syndrome. Crit Care Med 2001;29:1579-1586.
28. Richard JC, Maggiore SM, Jonson B, Mancebo J, Lemaire F, Brochard L. Influence of tidal volume on alveolar recruitment: respective role of PEEP and a recruitment maneuver. Am J Respir Crit Care Med 2001;163:1609-1613.
29. Mancini M, Zavala E, Mancebo J, Fernandez C, Barbera JA, Rossi A, Roca J, Rodriguez-Roisin R. Mechanisms of pulmonary gas exchange improvement during a protective venlilatory strategy in acute respiratory distress syndrome. Am J Respir Crit Care Med 2001;164:1448-1453.
30. Rimensberger PC, Cox PN, Frndova H, Bryan AC. The open lung during small tidal volume ventilation: concepts of recruitment and "optimal" positive end-expiratory pressure. Crit Care Med 1999;27:1946-1952.
31. Rinaldo JE, Rogers RM. Adult respiratory-distress syndrome: changing concepts of lung injury and repair. N Engl J Med 1982;306:900-909.
32. Bernard GR, Artigas A, Brigham KL, Carlet J, Falke K, Hudson L, Lamy M, Legall JR, Morris A, Spragg R. The American-European Consensus Conference on ARDS: definitions, mechanisms, relevant outcomes, and clinical trial coordination. Am J Respir Crit Care Med 1994;149:818-824.
33. Gattinoni L, Pesenti A, Avalli L, Rossi F, Bombino M. Pressure-volume curve of total respiratory system in acute respiratory failure: computed tomographic scan study. Am Rev Respir Dis 1987;136:730-736.
34. Gattinoni L, D'Andrea L, Pelosi P, Vitale G, Pesenti A, Fumagalli R. Regional effects and mechanism of positive end-expiratory pressure in early adult respiratory distress syndrome. JAMA 1993;269:2122-2127.
35. Webb HH, Tierney DF. Experimental pulmonary edema due to intermittent positive pressure ventilation with high inflation pressures: protection by positive end-expiratory pressure. Am Rev Respir Dis 1974;110:556-565.
36. Kolobow T, Moretti MP, Fumagalli R, Mascheroni D, Prato P, Chen V, Joris M. Severe impairment in lung function induced by high peak airway pressure during mechanical ventilation: an experimental study. Am Rev Respir Dis 1987;135:312-315.
37. Dreyfuss D, Soler P, Saumon G. Mechanical ventilation-induced pulmonary edema: interaction with previous lung alterations. Am J Respir Crit Care Med 1995;151:1568-1575.
38. Dreyfuss D, Saumon G. Role of tidal volume, FRC, and end-inspiratory volume in the development of pulmonary edema following mechanical ventilation. Am Rev Respir Dis 1993;148:1194-1203.
39. Puybasset L, Gusman P, Muller JC, Cluzel P, Coriat P, Rouby JJ. Regional distribution of gas and tissue in acute respiratory distress syndrome: III. Consequences for the effects of positive end-expiratory pressure. CT Scan ARDS Study Group. Intensive Care Med 2000;26:1215-1227.
40. Dambrosio M, Roupie E, Mollet JJ, Anglade MC, Vasile N, Lemaire F, Brochard L. Effects of positive end-expiratory pressure and different tidal volumes on alveolar recruitment and hyperinflation. Anesthesiology 1997;87:495-503.
41. Vieira SR, Puybasset L, Richecoeur J, Lu Q, Cluzel P, Gusman PB, Coriat P, Rouby JJ. A lung computed tomographic assessment of positive end-expiratory pressure-induced lung overdistension. Am J Respir Crit Care Med 1998;158:1571-1577.
42. Ranieri VM, Eissa NT, Corbeil C, Chasse M, Braidy J, Matar N, Milic-Emili J. Effects of positive end-expiratory pressure on alveolar recruitment and gas exchange in patients with the adult respiratory distress syndrome. Am Rev Respir Dis 1991;144:544-551.
43. Hartog A, Vazquez de Anda GF, Gommers D, Kaisers U, Lachmann B. At surfactant deficiency, application of "the open lung concept" prevents protein leakage and attenuates changes in lung mechanics. Crit Care Med 2000;28:1450-1454.
44. Artigas A, Bernard GR, Carlet J, Dreyfuss D, Gattinoni L, Hudson L, Lamy M, Marini JJ, Matthay MA, Pinsky MR, et al. The American-European Consensus Conference on ARDS. 2. Ventilatory, pharmacologic, supportive therapy, study design strategies and issues related to recovery and remodeling. Intensive Care Med 1998;24:378-398.
45. Marini JJ. Recruitment maneuvers to achieve an "open lung"-whether and how? Crit Care Med 2001;29:1647-1648.
46. Arold SP, Mora R, Lutchen KR, Ingenito EP, Suki B. Variable tidal volume ventilation improves lung mechanics and gas exchange in a rodent model of acute lung injury. Am J Respir Crit Care Med 2002;165:366-371.
47. Lefevre GR, Kowalski SE, Girling LG, Thiessen DB, Mutch WA. Improved arterial oxygenation after oleic acid lung injury in the pig using a computer-controlled mechanical ventilator. Am J Respir Crit Care Med 1996;154:1567-1572.
48. Suki B, Barabasi AL, Hantos Z, Petak F, Stanley HE. Avalanches and power-law behaviour in lung inflation. Nature 1994;368:615-618.
49. Boker A, Graham MR, Walley KR, McManus BM, Girling LG, Walker E, Lefevre GR, Mutch WA. Improved arterial oxygenation with biologically variable or fractal ventilation using low tidal volumes in a porcine model of acute respiratory distress syndrome. Am J Respir Crit Care Med 2002;165:456-462.
50. Hickling KG, Henderson SJ, Jackson R. Low mortality associated with low volume pressure limited ventilation with permissive hypercapnia in severe adult respiratory distress syndrome. Intensive Care Med 1990;16:372-377.
51. Nieman GF, Bredenberg CE, Clark WR, West NR. Alveolar function following surfactant deactivation. J Appl Physiol 1981;51:895-904.
52. Ranieri VM, Brienza N, Santostasi S, Puntillo F, Mascia L, Vitale N, Giuliani R, Memeo V, Bruno F, Fiore T, Brienza A, Slutsky AS, et al. Impairment of lung and chest wall mechanics in patients with acute respiratory distress syndrome: role of abdominal distension. Am J Respir Crit Care Med 1997; 156:1082-1091.
53. Roupie E, Dambrosio M, Servillo G, Mentec H, el Atrous S, Beydon L, Brun-Buisson C, Lemaire F, Brochard L. Titration of tidal volume and induced hypercapnia in acute respiratory distress syndrome. Am J Respir Crit Care Med 1995;152:121-128.
54. Suter PM, Fairley HB, Isenberg MD. Effect of tidal volume and positive end-expiratory pressure on compliance during mechanical ventilation. Chest 1978;73:158-162.
55. Malbouisson LM, Muller JC, Constantin JM, Lu Q, Puybasset L, Rouby JJ. Computed tomography assessment of positive end-expiratory pressure-induced alveolar recruitment in patients with acute respiratory distress syndrome. Am J Respir Crit Care Med 2001;163:1444-1450.
Jeffrey M. Halter, Jay M. Steinberg, Henry J. Schiller, Monica DaSilva, Louis A. Gatto, Steve Landas, and Gary F. Nieman
Departments of Surgery and Pathology, State University of New York Upstate Medical University, Syracuse, New York; and Department of Biological Sciences, State University of New York College at Cortland, Cortland, New York
(Received in original form May 16, 2002; accepted in final form February 20, 2003)
Supported in part by a grant from Hamilton Medical, Inc.
Correspondence and requests for reprints should be addressed to Dr. Jeffrey M. Halter, M.D., SUNY Upstate Medical University, Department of Surgery, 750 E. Adams Street, Syracuse, NY 13210. E-mail: halterj@upstate.edu
Copyright American Thoracic Society Jun 15, 2003
Provided by ProQuest Information and Learning Company. All rights Reserved