Johnson BA, Ait-Daoud N, Bowden CL, et al. Oral topiramate for treatment of alcohol dependence: a randomized controlled trial. Lancet 2003; 361:1677-1685.
* PRACTICE RECOMMENDATIONS
Oral topiramate is effective in the treatment of alcohol dependence. Patients taking topiramate consumed less alcohol, had fewer heavy drinking days, and had more days abstinent within a 12-week period. This medication adds a significant adjunct to our current treatment of alcoholism and can be considered for use in treating those alcoholics who desire sobriety.
* BACKGROUND
Alcohol dependence is a fairly common problem seen in family practice. To date, there have been few, if any, effective medications that help patients control or reduce their drinking behavior.
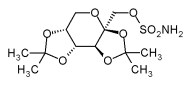
Topiramate is an anticonvulsant that inhibits dopamine release in portions of the brain that may be associated with alcohol's rewarding effects. Carbamazepine, another anticonvulsant, has been shown to decrease drinking among patients in alcohol withdrawal programs. (1) This trial tested the efficacy of treatment with topiramate (in addition to counseling) as a method of reducing alcohol consumption and initiating abstinence.
* POPULATION STUDIED
These researchers enrolled 150 patients with alcohol dependence, as defined by the Diagnostic and Statistical Manual of Mental Disorders, 4th edition (DSM-IV), into the study. They randomly assigned subjects to treatment or placebo groups.
At baseline, the 2 groups did not differ by sex, average number of drinks per day, or age of onset of alcohol abuse. Subjects' average age was 42 years (range, 21-65); 71% were men; 64% white, 32% Hispanic, and 3% African American. Subjects drank an average of 9 drinks per day, with an average 14-year history of alcohol abuse.
Researchers excluded study participants with a positive urine toxicological screen for narcotics, amphetamines, or sedative hypnotics; alcohol withdrawal symptoms; clinically significant physical abnormalities; a history of renal impairment or stones; seizures; or unstable hypertension. They also excluded pregnant or lactating participants and those taking medications affecting alcohol consumption.
Also excluded were study subjects undergoing compulsory treatment for alcohol dependence by an outside agency, subjects treated for alcohol dependence within the 30 days prior to enrollment, or subjects with a current Axis 1 diagnosis other than alcohol or nicotine dependence.
* STUDY DESIGN AND VALIDITY
Patients were randomly assigned to receive escalating doses of either topiramate (maximum of 300 mg/d) or placebo for a period of 12 weeks. Subjects, clinicians, and those assessing treatment outcomes were blind to group assignment; however, it is unclear whether allocation to the groups was concealed.
Patients also underwent brief behavioral counseling administered by trained nurse practitioners. Researchers did not address whether study participants also underwent other behavioral interventions, such as Alcoholics Anonymous meetings. Researchers used an intention-to-treat approach in their statistical analyses.
* OUTCOMES MEASURED
The investigators measured 6 primary outcomes on a weekly basis throughout the 12 weeks of the study. They assessed the number of drinks per day, drinks per drinking day, heavy drinking days (defined as 5 or more drinks for men or 4 or more drinks for women), and number of days abstinent.
They also measured weekly plasma gammaglutamyl transferase (GGT) levels, as an objective measure of alcohol consumption, and a secondary efficacy variable of self-reported craving, which they measured with a 14-item obsessive compulsive drinking scale (validated in a previous study of alcoholism severity). (2)
* RESULTS
Patients taking topiramate had an average of 1 fewer drink per day, both on drinking days and on a daily basis, 15% fewer days of heavy drinking, and approximately 12% more days of abstinence compared with the placebo group. The numbers were even more significant at the end of the study, showing a trend in increasing efficacy over the 12 weeks of follow up. The anticraving effects were also more significant at the end than when averaged over the length of the study. Plasma GGT levels had a statistically significant drop during the study and obsessive-compulsive drinking scale factor scores decreased significantly. All 150 subjects completed the study, and they reported no adverse events.
REFERENCES
(1.) Malcolm R, Myrick H, Roberts J, Wang W, Anton RF, Ballenger JC. The effects of carbamazepine and lorazepam on single versus multiple previous alcohol withdrawals in an outpatient randomized trial. J Gen Intern Med 2002; 17:349-355.
(2.) Moak DH, Anton RF, Latham PK. Further validation of the Obsessive-Compulsive Drinking Scale (OCDS). Relationship to alcoholism severity. Am J Addict 1998; 7:14-23.
Noble Anderson, MD, and M. Norman Oliver, MD, Department of Family Medicine, University of Virginia, Charlottesville. E-mail: nea2p@virginia.edu.
COPYRIGHT 2003 Dowden Health Media, Inc.
COPYRIGHT 2003 Gale Group