Abstract
Basal cell carcinomas (BCCs) that arise in sun-protected sites are quite uncommon. We report a case of BCC of the areola, which is extremely rare. Mohs micrographic surgery was used for the treatment. The etiologic factors of BCCs in sun-protected areas are discussed, and previous studies regarding the treatment modalities are reviewed.
**********
Introduction
Basal cell carcinoma (BCC) is the most common human malignancy with at least 900,000 new cases diagnosed annually in the United States. (1) It accounts for 75% of all non-melanoma skin cancers diagnosed in the United States each year. (2) BCCs usually occur in elderly patients on the sun-exposed skin of the head and neck, (3) and occur infrequently on sun-protected skin such as the breast, genital, and perianal regions. (4) While BCC may occur on the breast, a BCC entirely or partially located on the areola-nipple complex is a rare phenomenon, and only 20 patients with areola and nipple BCCs have been described in the literature. We report a case of a BCC on the areola in a 61-year-old man treated with Mohs micrographic surgery.
Case Report
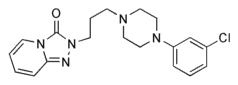
A 61-year-old light-skinned male was referred to the University of Miami Mohs and Laser Surgery Clinic. Initially, he was evaluated at the Miami Veteran Affairs Medical Center and was diagnosed with a biopsy-proven basal cell carcinoma. His relevant past medical history included two previous BCCs removed in 2001: one on the and one on the left anterior abdomen. In 1967, during his military service, a barracks fire caused burns involving his face and chest wall. His current medications include aspirin, Plavix[R], sertraline, trazodone, gemfibrozil, and omeprazole.
On physical examination, there was a 0.6 X 0.5 cm pink, pearly papule located on the inferomedial aspect of his left areola. The lesion had ill-defined borders; no ulceration, discharge, or exudate was noted. No other abnormalities of the nipple were noted. A scar was seen on the left anterior abdomen from a previous BCC removal. There was no axillary lymphadenopathy. The examination failed to demonstrate any further suspicious lesions on the upper half of his body.
Mohs micrographic surgery, with its tissue-sparing properties, was performed due to the tumor's location. The skin cancer was initially curetted 3 times (Figure 1). After the first stage of Mohs surgery, the defect size was 1.2 X 1.8 cm (Figure 2). Hemostasis was obtained using electrocautery. After microscopic examination of the tissue specimen, the margins were clear after stage 1; no further surgery was required. The surgical defect was closed with deep 4-0 polyglactin 910 (Vicryl[TM]; Ethicon, Summerville, NJ) sutures and standard running sutures using 5-0 nylon monofilament (Ethilon[TM], Ethicon, Summerville, NJ) sutures (Figure 3).
Discussion
Basal cell carcinomas that arise in sun-protected sites are quite uncommon, with an estimated annual incidence of 10% to 15% of all diagnosed BCCs. (5) Although ultraviolet radiation (UVR) may be an important factor for BCCs on sun-exposed areas, their occurrence on sun-protected areas raises the possibility of other etiologic agents. These include exposure to ionizing radiation or arsenic, immunosuppression, history of skin cancer, prior injury such as trauma and burns, light skin color, nevus sebaceous, or genodermatoses such as basal cell nevus syndrome and xeroderma pigmentosum. (1,2) Depressed immune surveillance caused by ultraviolet radiation at distant sites may also be involved in the pathogenesis of BCCs at non-sun-exposed sites. (6) Our patient was light-skinned and had a history of non-melanoma skin cancer. Both BCC and squamous cell carcinoma (SCC) correlate with chronic, cumulative UVR exposure. However, it is more common for BCCs than SCCs to occur in sun-protected areas. (1) Heckmann et al said that areas with a high incidence of BCCs despite low UVR exposure, such as the medial quadrant of the orbit, are characterized by a concave shape, reduced skin tension, and the presence of marked skin folds. (7) They hypothesized that the disturbed cell matrix interactions found at these sites could be a cofactor for developing BCCs. The areola-nipple area may share these same characteristics.
[FIGURE 1 OMITTED]
[FIGURE 2 OMITTED]
[FIGURE 3 OMITTED]
BCC has been estimated to metastasize at a rate of less than 0.025%. (8) However, metastases to the axillary lymph nodes were reported in 3 of the previous 20 cases of BCCs involving the areola-nipple area. It may reflect the possibility that BCCs of the areola-nipple area are more aggressive. However, these reported tumors were large and ulcerated, and hence at higher risk for metastasis occurrence. Since our patient's tumor was a relatively small primary lesion, and we did not find any evidence of axillary lymph node involvement, the risk of metastasis is low. Nonetheless, he was advised of the need for post-operative follow-up to monitor for signs of recurrence or metastasis.
Mohs surgery was used for the treatment of our patient due to the location of the tumor. Tissue-sparing is very important with lesions involving the areola. It has been used in the treatment of three of the previously reported cases of BCCs of this area. (8-10) Mohs micrographic surgery may offer the best chance of cure, especially when the tumor is large, the histology is more aggressive, and when maximum uninvolved tissue preservation is desired. (2) Most of the other BCCs of this area were treated by simple excision, and some of them received post-operative radiation therapy. (8)
References
1. LeSueur BW, DiCaudo DJ, Connolly SM. Axillary basal cell carcinoma. Dermatol Surg. 2003; Nov;29(11):1105-8.
2. Gibson GE, Ahmed I. Perianal and genital basal cell carcinoma: a clinicopathologic review of 51 cases. J Am Acad Dermatol. 2001; Jul;45(1):68-71.
3. Gloster HM, Brodland DG. The epidemiology of skin cancer. Dermatol Surg. 1996;22:217-22.
4. Betti R, Bruscagin C, Inselvini E, Crosti C. Basal cell carcinomas of covered and unusual sites of the body. Int J Dermatol. 1997;36:503-5.
5. Gardner ES, Goldberg LH. Axillary basal cell carcinoma: literature survey and case report. Dermatol Surg. 2001;Nov;27(11):966-8.
6. Strickland PT, Creasia D, Kripke ML. Enhancement of two-stage skin carcinogenesis by exposure of distant skin to UV radiation. J Natl Cancer Inst. 1985;74:1129-34.
7. Heckmann M, Zogelmeier F, Konz B. Frequency of facial basal cell carcinoma does not correlate with site-specific UV exposure. Arch Dermatol. 2002;138:1494-7.
8. Zhu YI, Ratner D. Basal cell carcinoma of the nipple: a case report and review of the literature. Dermatol Surg. 2001; Nov;27(11):971-4.
9. Sanchez-Carpintero I, Redondo P, Solano T. Basal cell carcinoma affecting the areola-nipple complex [letter]. Plast Reconstr Surg. 2000;105:1573.
10. Weber PJ, Moody BR, Foster JA. Series spiral advancement flap: an alternative to the ellipse. Dermatol Surg. 2001;27:64-6.
Keyvan Nouri MD, (a) Christopher J. Ballard BS, (b) Navid Bouzari MD, (b) Sogol Saghari MD (c)
a. Associate Professor of Dermatology and Otolaryngology, Director of Mohs, Dermatologic, and Laser Surgery, Director of Surgical Training
b. Research Fellow
c. Resident Department of Dermatology and Cutaneous Surgery
University of Miami School of Medicine, Miami, FL
Address for Correspondence
Keyvan Nouri MD
1475 NW 12th Ave, Suite 2175
Miami, FL 33131
e-mail: knouri@med.miami.edu
Phone: 305-243-9446
Fax: 305-243-4184
COPYRIGHT 2005 Journal of Drugs in Dermatology, Inc.
COPYRIGHT 2005 Gale Group