To the editor:
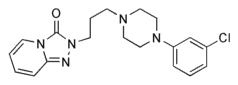
The only thing missing from the well-intentioned tramadol piece in JFP (McDiarmid T, Mackler L, Schneider DM, "Clinical inquiries. What is the addiction risk associated with tramadol?" J Fam Pract 2005; 54[1]:72-73) was a little common sense. The low numbers they quoted on tramadol addiction and detoxification seem paltry in comparison with illicit opiates (such as heroin) and diverted opiates (such as OxyContin), but the numbers can be deceptive--reporting agencies rarely know what's going on in the real world. In the treatment arena we see staggering amounts of Ultracet and tramadol addiction, with patients popping up to 30 or 40 pills daily to fill an ever-expanding mureceptor void. Many of these fall into the addiction innocently because, and I quote, "My doctor told me that these were safe!" Far from it. The tramadol mu activity is considerable in the opiate-naive patient, and even more so in the recovering opiate addict. The phenomenon of "reinstatement," where any activity at the receptor level triggers old drug-seeking behavior, is well documented, and should be avoided at all costs, especially given the broad nonopiate choices available to our patients in need, including the highly effective neural modulators (such as Neurontin, Depakote, and Trazodone) and NSAID/ COX-2 families. While any primary doc can step into the waters of addiction medicine, some formal training may help avoid potential disasters.
If a patient merits relief from pain that is not handled by current nonsteroidal and adjunctive modality therapy (lets not forget TENS units, massage therapy, and acupuncture), then certainly consider tramadol--but let's also consider the risks and warn the patient accordingly. Monitor their usage periodically, and don't give refills unless the patient is traveling out of the area. And finally, if your patient is one of the millions of opiate addicts seeking relief from bone-fide pain, do him and yourself a favor--don't use an opiate unless absolutely necessary, having exhausted all other measures. The risk of relapse is too great. Lest we forget, "Above all, do no harm."
Stephen Patt, MD, Family Practice, Santa Monica, Calif
Dr McDiarmid responds:
I regret that Dr Patt did not appreciate the emphasis I hoped to convey of the limitations on validity and generalizability of the manufacturer-sponsored surveillance program's estimated rates of tramadol abuse in a tramadol-exposed population. The limitations mentioned in the Clinical inquiry included nonrandom and nonrepresentative sampling methods, tramadol abuse likely suppressed by presence of more potent euphoriant in the studied addiction communities, and the low return rates of surveys from substance abuse experts. Each of these biases could significantly alter any attempts at estimating tramadol abuse rates in the general tramadolexposed populations.
I appreciate Dr Patt sharing his experience with patients who abuse large quantities of tramadol. There are case reports in the literature describing similar patient behaviors. I would encourage him to report such case experiences to the FDA's MedWatch program so that what is a personal clinical experience can contribute to the evidence of out collective knowledge.
FAST TRACK In the treatment arena we see staggering amounts of Ultracet and tramadol addiction
Todd McDiarmid, MD, Moses Cone Health System, Department of Family Medicine, University of North Carolina School of Medicine, Greensboro
COPYRIGHT 2005 Dowden Health Media, Inc.
COPYRIGHT 2005 Gale Group