Inhaled glucocorticosteroids (ICS) are commonly prescribed for chronic obstructive pulmonary disease. No adverse effect on bone mineral density (BMD) has been proven. In a randomized double-blind, placebo-controlled trial at seven centers in North America, we recruited 412 current smokers or recent quitters with mild to moderate chronic obstructive pulmonary disease. They used inhaled triamcinolone acetonide, 600 meg, or placebo, twice daily. We measured femoral neck and lumbar spine BMD at baseline and after 1 and 3 years, and serum osteocalcin at baseline, 3 months, 1 year, and 3 years. After 3 years, BMD at the femoral neck decreased 1.78% more with ICS than with placebo (p
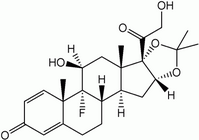
Keywords: bone density; obstructive lung diseases; osteoporosis; randomized controlled trials; triamcinolone acetonide
Inhaled glucocorticosteroids (ICS) are commonly used for the treatment of chronic obstructive pulmonary disease (COPD), although their effectiveness has not been established. Several recent large multicenter randomized trials investigated the efficacy of ICS in COPD (1-5). None found a difference between ICS and placebo in the rate of decline of FEV^sub 1^ over 2 to 3.5 years. Several studies have found a reduction in exacerbations and symptoms associated with ICS (1, 2, 4, 6-8). A subsequent nonrandomized study of patients dismissed from hospital after exacerbation of COPD showed lower rates of rehospitalization and death among those prescribed ICS (9).
The adverse effects of long-term use of systemic glucocorticosteroids include loss of bone mineral density (BMD) (10,11), fractures (12), adrenal suppression, glaucoma and cataracts, diabetes, myopathy, hypertension, and loss of skin integrity (12). Reported but unproven effects of ICS include cataracts (13-15), glaucoma (16, 17), adrenal suppression (18), and skin bruising (2, 15, 18-20).
Studies of the effect of ICS on bone metabolism in adults with asthma show mixed results (18, 21-25, 56). One uncontrolled longitudinal study over 3 years showed a dose-related decline in bone density at the hip in premenopausal women with asthma using ICS (26). In the only long-term controlled study of patients with COPD treated with budesonide, no adverse effect on BMD was found (2). Two systematic reviews have concluded that the long-term use of ICS is not proven to cause significant changes in BMD (27, 28). This issue remains controversial, however, and several recent studies address the evidence of nonvertebral fracture risk (29-32).
Many patients with COPD have risk factors for osteoporosis, including older age, female sex, impaired nutritional status, low exercise levels, and tobacco smoking (33-35). The Lung Health Study II (LHS II) was designed to study the efficacy of inhaled triamcinolone (1,200 µg/day Azmacort) in slowing the decline of FEV^sub 1^ in current smokers and recent quitters with mild to moderate COPD. This trial afforded the opportunity to examine the effect of the long-term use of ICS on bone metabolism in COPD. We performed serial measurements of BMD and serum osteocalcin over 3 years in a subgroup of 412 participants (1).
METHODS
Participants
LHS II recruited 1,116 participants with COPD (ages 40-69 years). Based on a sample size estimate for this ancillary study, we recruited 412 participants from the LHS II for measurements of BMD and osteocalcin. Willing participants were recruited sequentially until the recruitment goal was met. Women were recruited in equal numbers to men. Of the potential LHS II recruits, five were excluded because of use of glucocorticosteroids (OCS) and two for use of ICS in the previous 6 months. Exclusion criteria for the BMD study included known osteoporosis, other disorders of calcium metabolism, or a condition that might interfere with participation. Participants were randomized to triamcinolone acetonide (Azmacort) six puffs twice a day (1,200 µg/day) or placebo. We obtained written consent, approved by the institutional review board at each center. Methods for the LHS II have been described (1, 36).
BMD Measurements
BMD scans of the hip and lumbar spine were performed using dual-energy X-ray absorptiometry at baseline and the end of the first and third years with Hologic model 1000, 1000W, or 2000 pencil-beam scanner. We used the same equipment for the entire study. Scanners were calibrated at the beginning and annually with a single standard spine model. Scanners were calibrated against local standards on each day of testing. Digitized data were analyzed without knowledge of treatment assignment at a central reading center. Hip data are presented only for the femoral neck and lumbar spine data for L2 to L4. Hologic reference values were used (10).
Osteocalcin
Serum osteocalcin levels were drawn before 10:00 A.M. at baseline and at 3, 12, and 36 months of treatment. Samples were stored at -70°C until shipped for batch processing using radioimmuno assay (ELSA-OSTEO; CIS US Inc., Bedford, MA). The laboratory was unaware of treatment assignment. A two-level calibration against standard samples was performed each day of testing.
Data Analysis
Descriptions of data were based on counts for categorical data or means and SDs for continuous variables. Bivariate comparisons between the treatment groups used chi-square statistics (for categorical variables) or unpaired t tests (for continuous variables). Controlled comparisons of outcome variables were done with multivariate linear regression using PROC GLM in SAS (SAS version 6.12; SAS, Inc., Cary, NC) (37). No adjustment was made for multiple comparisons; nominal p values are shown.
Changes in BMD were analyzed separately for baseline to Year 1, baseline to Year 3, and Year 1 to Year 3. Baseline characteristics included treatment group, age, sex, race, smoking status, baseline BMD of the femoral neck and lumbar spine, use of calcium or vitamins, use of estrogen and self-reported menopausal status in women, FEV^sub 1^ percentage predicted before and after bronchodilator, methacholine responsiveness, number of cigarettes per day, body mass index, activity level, and weight change. The results are summarized in terms of percentage changes in BMD associated with each significant predictor or specified increments in the predictor.
Baseline data were available for all of the 412 participants. Femoral neck BMD results are reported for those with three technically acceptable measurements (baseline, Year 1, and Year 2) from the hip (n = 359; 8 [2%] had technically inadequate data, and 45 [11%] had missing data). Lumbar spine BMD results are reported for those with three technically acceptable measurements from the spine (n = 328; 45 [11%] had technically inadequate data, and 39 [9%] had missing data). Other follow-up data are reported for all participants who belonged to one group or the other (n = 363).
RESULTS
Participant Characteristics
The baseline characteristics of participants are shown in Table 1. The ICS group participants were slightly younger and had a slightly higher FEV^sub 1^, and fewer reported taking calcium supplements.
Follow-up
The longitudinal analyses of BMD included participants with technically satisfactory scans at all three study visits (328 lumbar spine and 359 femoral neck). Technically, inadequate spinal scans were mostly due to degenerative joint disease or scoliosis. Follow-up rates and technically satisfactory scan rates were similar in the two treatment groups. The average weight gain over 3 years was 0.41 ± 5.8 kg (mean ± SD). There was no difference between the groups in this regard (p = 0.54).
Adherence
Adherence was monitored by inhaler canister weight at 3-month visits. Good adherence (≥ 9 puffs/day averaged over 3 years) was observed in 46.6% of participants; 21.2% had satisfactory adherence (6-8.99 puffs/day); 13.2% had less than satisfactory adherence (3-5.99 puffs/day); 8.3% had poor adherence (1-2.99 puffs/day), and 10.7% had very poor adherence (
Baseline Bone Density
Table 2 shows bone densities for lumbar spine and femoral neck by treatment assignment with sexes combined and separated. We found no differences between the active drug and placebo group for any of the baseline measurements. A baseline femoral neck BMD below the fifth percentile (10) was observed in 15 men and 21 women. A baseline lumbar spine BMD below the fifth percentile was observed in 26 men and 9 women.
Change in Femoral Neck BMD
Femoral neck BMD showed no change and no difference between the ICS and placebo groups during the first year of treatment (Table 2 and Figure 1). Between Year 1 and Year 3, there was a -1.66 ± 4.40% change in femoral neck BMD in the active treatment group but no change (0.1 ± 4.01%) in the placebo group (p
We analyzed the results by adherence level (Table 3). The difference in femoral neck BMD between the ICS group and the placebo group was significant only for those who used nine or more inhalations per day (-1.92%, p = 0.003).
A multivariate analysis was performed (Table 4) to determine whether other factors contributed to the loss of femoral neck BMD and whether there was any subgroup that might be at particular risk. In addition to the effect of the study medication, age of more than 56 years (the median age among our participants) was associated with a greater loss of femoral neck BMD. Sex, baseline femoral BMD, cigarette smoking, and the use of estrogen, calcium supplements, vitamin D, or multivitamins were not significant predictors of change in femoral BMD.
At Year 3, in the ICS group, 31 (16 men and 15 women) had a more than 6% decrease in femoral neck BMD compared with baseline. In the placebo group, 13 (8 men and 5 women) had a more than 6% decrease in femoral neck BMD. The difference between the ICS group and placebo group was significant for men and women combined (p = 0.002) and for women (p = 0.008) but not for men (p = 0.091). In the ICS group, 20 participants (6 men and 14 women) had a femoral neck BMD below the fifth percentile at 3 years; in the placebo group, 15 participants (7 men and 8 women) had a femoral neck BMD below the fifth percentile (p = NS).
Change in Lumbar Spine BMD
Between baseline and Year 1, there was no change in spine BMD for either treatment group, and the difference between groups was not significant (Table 2 and Figure 2). Between Year 1 and Year 3 the active treatment group showed a -0.30 ± 3.49% decrease in BMD, and the placebo group showed a 1.52 ± 4.15% increase in BMD (p
We analyzed the effect of drug adherence on changes in lumbar spine BMD (Table 3). The ICS participants who used nine or more puffs per day showed a significantly lower lumbar spine BMD (-2.15%, p = 0.003). The numbers of participants in the lower adherence subgroups were small, and no significant effects were observed.
A multivariate analysis (Table 4) showed that in addition to the effect of the medication, women had a greater loss of spine BMD than men did. Participants who were older than the median age of 56 years had a greater increase in spine BMD. Smoking appeared to have a deleterious effect in proportion to number of cigarettes smoked at baseline (p = 0.056). Baseline spine BMD and the use of estrogen, vitamin D, calcium, and multivitamins were not predictors of change in spine BMD.
No difference was observed between the ICS group and the placebo group in the number of participants with spine BMD below the fifth percentile or with a decline of 6% or more at 3 years.
Other Factors Considered in Analysis of BMD
At the beginning of the study, we excluded potential participants who reported recent use of oral or systemic glucocorticosteroids (OCS). During the course of the study, some participants were given short courses of OCS as part of their medical care (34 ICS and 34 placebo). We found no difference between those who used OCS and those who did not. After controlling for OCS, the medication effect of ICS on BMD was significant at both the femoral neck (p
More participants in the ICS group than the placebo group (11 ICS vs. 2 placebo) used thyroid replacement. Participants in the ICS group who used thyroid replacement had a slightly (but not significantly) greater BMD loss in both femur and spine than those who did not. When we reanalyzed the changes in femoral and spinal BMD excluding participants using thyroid replacement therapy, the results were unchanged, and the differences from baseline to Year 3 remained significant (p
Self-reported physical activity levels (no regular exercise, moderate, vigorous) had no effect on femoral or spinal BMD. After controlling for baseline physical activity, the effect of ICS on BMD was unchanged and still significant (p
Osteocalcin
The osteocalcin levels were similar at baseline between groups (Figure 3). The ICS group had lower osteocalcin levels than the placebo group after 3 months of treatment (p = 0.002). This difference between treatment groups persisted but was smaller at Year 1 (p = 0.031). The difference had disappeared by Year 3 (p = 0.675). Osteocalcin levels were lower in both treatment groups at Year 1 and Year 3 compared with baseline and 3 months. The differences between treatment groups were significant at both 3 months and Year 1. We found no association between changes in osteocalcin levels and changes in BMD at any point (data not shown).
Clinical Indicators of Osteoporosis
We found no difference in the number of participants who lost 1 cm or more of height during the course of the study (36 men and 18 women in the ICS group and 28 men and 27 women in the placebo group, p = NS). Likewise, there was no difference in the number of participants who lost 2 cm or more of height (17 men and 9 women in the ICS group and 14 men and 11 women in the placebo group, p = NS). A small number of participants reported fractures of the spine or hip during the study: five men and one woman in the ICS group and seven men and eight women in the placebo group (p = NS, p = 0.23). Fracture of any bone was reported by 14 participants in the ICS group (seven men and seven women) and 21 participants in the placebo group (6 men and 15 women, p = 0.29 for ICS vs. placebo). The number of participants who reported a diagnosis of osteoporosis during the study was not different between the ICS group (no men and 11 women) and the placebo group (2 men and 12 women, p = NS).
DISCUSSION
The primary end-point result of this randomized controlled clinical trial is that participants with COPD assigned to use 1,200 µg/ day of inhaled triamcinolone for 3 years demonstrated reduced BMD of both the lumbar spine and the femoral neck compared with participants assigned to placebo: a mean deficit of 1.78% in femoral neck BMD and 1.33% in lumbar spine BMD. These differences in BMD occurred in both men and women. In addition, more users of triamcinolone than users of placebo experienced a 6% or more decline in femoral neck BMD. On the other hand, there was no difference in complications attributable to loss of BMD (e.g., fractures, loss of height, diagnoses of osteoporosis).
We cannot determine whether the change in BMD observed at 3 years would continue, level off, or accelerate with continued use of ICS. Although the magnitude of loss of BMD observed would not cause serious morbidity in healthy persons, it could contribute to the risk of fracture among people with pre-existing osteoporosis. If the observed loss of BMD, a surrogate indicator of fracture risk, were to persist for many years of ICS treatment, it might contribute to development of osteoporosis and fractures in susceptible individuals. The effects of ICS on other elements of fracture risk, such as bone architecture, are not known. Studies of postmenopausal osteoporosis indicate that the relative risk of fracture approximately doubles for every 1 SD (approximately 10%) decrease in BMD below the age-adjusted mean for the hip and spine (10, 38-40). A large number of persons with COPD currently use, or at some point may use, ICS. The results of this study support and extend other evidence that ICS have systemic effects. Many persons with COPD have risk factors for osteoporosis, including older age, smoking, poor nutrition, and sedentary lifestyle (33-35).
The strengths of this study, in comparison with most previous studies of ICS on BMD, include a randomized, placebo-controlled design, larger number of participants, a high rate and long duration of follow-up, inclusion of large numbers of susceptible individuals (women, smokers, older individuals), rigorous centralized quality control of BMD scans, and objective monitoring of drug adherence. These factors may account for the positive findings in this study in comparison to previous negative studies, most of which were smaller and had shorter follow-up times.
An important and unexpected finding of this study was the delay in the decline in BMD, which was not apparent during the first year of the study. There was little or no change in BMD during the first year, although osteocalcin levels indicate that the metabolic effect of the ICS began early. The losses in BMD occurred during the second and third years of the trial.
Therefore, short-term studies of the effect of ICS on bone density cannot be used to predict longer term effects (41). These findings contrast with findings in studies using OCS, in which the loss of BMD is greater and occurs within the first 6 to 12 months of the start of therapy followed by slower subsequent rates of loss (10, 42-45).
An additional contrast with other studies is the larger effect in the femoral neck than in the lumbar spine, although similar findings have been reported (46). Histomorphometric studies show a greater effect of OCS on trabecular bone than on cortical bone so that one might expect a greater impact on the lumbar spine (11, 47), although both lumbar spine and femoral neck contain both trabecular and cortical bone. No study has analyzed the localization of bone loss with ICS, and the predominant site of bone loss in this study cannot be determined from our data.
Is the effect that we observed limited to triamcinolone or applicable to other ICS? Some newer formulations of ICS such as budesonide and fluticasone have more rapid first-pass hepatic metabolism and thus may have less systemic effect. On the other hand, these agents may be more potent or may be used in higher doses that may enhance systemic side effects. These newer agents have not been thoroughly tested for long-term effects on BMD (48, 49). Similarly, a lower dose may reduce the risk of loss of bone density.
The effect of continued smoking on the rate of decline in spine BMD was significant in this study. Other studies support this observation. Smoking prevalence is high in persons with COPD; therefore, if ICS are prescribed, smoking cessation should be encouraged for this reason among others.
In addition to the primary finding, we found that older participants had greater ICS-related loss of BMD at the hip but paradoxically increased BMD at the lumbar spine. The increase in spine BMD is not predicted by reference equations but has been documented to occur in population studies of men. It may be due to the effects of degenerative osteoarthritis (50, 51). Alternatively, it could be related to the large number of participants who used supplemental estrogen, calcium, vitamin D, and multivitamins (10). The positive trend in Z scores of all groups from baseline to Year 3 suggests that the LHS II cohort had a slower decline in BMD than the reference population (10). This does not alter the observed differences between the ICS-treated and the placebo groups, which are independent of the changes in Z scores. Osteocalcin levels indicated the presence of a systemic effect of ICS therapy but were not predictive in individual patients of the eventual loss in BMD.
Whereas recent studies have better defined the potential benefits of ICS in persons with COPD, this study indicates that ICS may contribute to accelerated decline in BMD in this population. Consensus recommendations suggest they be limited to persons with moderate to severe COPD and frequent exacerbations (52, 53). When prescribing moderate or higher doses of ICS to patients with COPD, it may be prudent to consider the recommendations of the American College of Rheumatology for the prevention of steroid-induced osteoporosis (54, 55). Smoking cessation, limitation of alcohol consumption, and regular exercise should be encouraged. It has been recommended that patients with asthma with lifetime "cumulative doses of 5,000 mg [equivalent to 11.4 years at the dose used in the present study] should be monitored by bone densitometry and considered for active intervention to reduce the risk of osteoporotic fracture in later life" (56). In this population, that recommendation seems prudent. In contrast, measurement of osteocalcin does not appear to be helpful in identifying persons likely to experience greater loss of BMD.
In summary, we found that in persons with mild to moderate COPD, the use of moderate to high dose inhaled triamcinolone was associated with accelerated loss of spinal and femoral BMD after 3 years. We did not observe an increase in clinical indicators of osteoporosis during the time course of the study. In the absence of longer term (> 3 years) safety data, the expected benefits of ICS therapy in COPD must be weighed against potential risks, including the risk of osteoporosis. Monitoring of BMD and the use of agents that may reduce bone loss (e.g., calcium supplementation, vitamin D supplementation, or bisphosphonates) should be considered for patients with an increased risk for osteoporosis.
References
1. The Lung Health Study Research Group. Effect of inhaled triamcinolone on the decline in pulmonary function in chronic obstructive pulmonary disease. N Engl J Med 2000;343:1902-1909.
2. Pauwels RA, Lofdahl C-G, Laitinen LA, Schouten JP, Postma DS, Pride NB, Ohlsson SV. Long-term treatment with inhaled budesonide in persons with mild chronic obstructive pulmonary disease who continue smoking. N Engl J Med 1999;340:1948-1953.
3. Vestbo J, Sorensen T, Lange P, Brix A, Torre P, Viskum K. Long-term effect of inhaled budesonide in mild and moderate chronic obstructive pulmonary disease: a randomised controlled trial. Lancet 1999;353: 1819-1823.
4. Burge PS, Calverley PMA, Jones PW, Spencer S, Anderson JA, Maslen TK. Randomised, double blind, placebo controlled study of fluticason propionale in patients with moderate to severe chronic obstructive pulmonary disease: the ISOLDE trial. BMJ 2000;320:1297-1303.
5. Paggiaro PL, Dahle R, Bakran I, Frith L, Hollingworth K, Efthimiou J. Multicentre randomised placebo-controlled trial of inhaled fluticasone propionale in patients with chronic obstructive pulmonary disease. International COPD Study Group. Lancet 1998;351:773-780.
6. Alsaeedi A, Sin DD, McAlister FA. The effects of inhaled corticosteroids in chronic obstructive pulmonary disease: a systematic review of randomized placebo-controlled trials. Am J Med 2002;13:59-65.
7. Mahler DA, Wire P, Horstman D, Chang CN, Yates J, Fischer T, Shah T. Effectiveness of fluticasone propionate and salmeterol combination delivered via the Diskus device in the treatment of chronic obstructive pulmonary disease. Am J Respir Crit Care Med 2002;166:1084-1091.
8. Calverley P, Pauwels R, Vestbo J, Jones P, Pride N, Gulsvik A, Anderson J, Maden C. Trial of Inhaled Steroids and long-acting beta2 agonists study group: combined salmeterol and fluticasone in the treatment of chronic obstructive pulmonary disease: a randomised controlled trial. Lancet 2003;361:449-456.
9. Sin DD, Tu JV. Inhaled corticosteroids and the risk of mortality and readmission in elderly patients with chronic obstructive pulmonary disease. Am J Respir Crit Care Med 2001;164:580-584.
10. Bonnick SL. Bone densitometry in clinical practice: application and interpretation. Totowa, NJ: Humana Press; 1998.
11. Dubois EF, Roder E, Dekhuijzen PN, Zwinderman AE, Schweitzer DH. Dual energy X-ray absorptiometry outcomes in male COPD patients after treatment with different glucocorticoid regimens. Chest 2002;121: 1456-1463.
12. McEvoy CE, Nicwoehner DE. Adverse effects of corticosteroid therapy for COPD: a critical review. Chest 1997;111:732-743.
13. Cumming RG, Mitchell P, Leeder SR. Use of inhaled corticosteroids and the risk of cataracts. N Engl J Med 1997;337:8-14.
14. Garbe E, Suissa S, LeLorier J. Association of inhaled corticosteroids with cataract extraction in elderly patients. JAMA 1998;280:539-543.
15. Agertoft L, Larsen FE, Pedersen S. Posterior subcapsular cataracts, bruises and hoarseness in children with asthma receiving long-term treatment with inhaled budesonide. Eur Respir J 1998;12:130-135.
16. Garbe E, LeLorier J, Boivin JF, Suissa S. Inhaled and nasal glucocorticoids and the risks of ocular hypertension or open-angle glaucoma. JAMA 1997;277:722-727.
17. Opatowsky I, Feldman RM, Gross R, Feldman ST. Intraocular pressure elevation associated with inhalation and nasal corticosteroids. Ophthalmology 1995;102:177-179.
18. Lipworth BJ. Systemic adverse effects of inhaled corticosteroid therapy: a systematic review and meta-analysis. Arch Intern Med 1999;159:941-955.
19. Malo JL, Cartier A, Gherao H, Mark S, Brown J, Laviolette M, Boulet LP. Skin bruising, adrenal function and markers of bone metabolism in asthmatics using inhaled beclomethasone and fluticasone. Eur Respir J 1999;13:993-998.
20. Roy A, Leblanc C, Paquctle L, Ghezzo H, Cote J, Cartier A, Malo JL. Skin bruising in asthmatic subjects treated with high doses of inhaled steroids: frequency and association with adrenal function. Eur Respir J 1996;9:226-231.
21. Wong CA, Walsh LJ, Smith CJP, Wisniewski AF, Lewis SA, Hubbard R, Cawte S, Green DJ, Pringle M, Tattersfleld AE. Inhaled corticosteroid use and bone-mineral density in patients with asthma. Lancet 2000;355:1399-1403.
22. Luengo M, del Rio L, Pons F, Picado C. Bone mineral density in asthmatic patients treated with inhaled corticosteroids: a case-control study. Eur Respir J 1997;10:2110-2113.
23. Herrala J, Puolijoki H, Impivaara O, Liippo K, Tala E, Nieminen MM. Bone mineral density in asthmatic women on high-dose inhaled beclomethasone dipropionate. Bone 1994;15:621-623.
24. Struijs A, Mulder H. The effects of inhaled glucocorticoids on bone mass and biochemical markers of bone homeostasis: a 1-year study of beclomethasone versus budesonide. Neth J Med 1997;50:233-237.
25. McEvoy CE, Ensrud KE, Bender E, Genant HK, Yu W, Griffith JM. Niewoehner DE. Association between corticosleroid use and vertebral fractures in older men with chronic obstructive pulmonary disease. Am J Respir Crit Care Med 1998;157:704-709.
26. Israel E, Banerjee TR, Fitzmaurice GM, Kotlov TV, LaHive K, LeBoff MS. Effects of inhaled glucocorticoids on bone density in premenopausal women. N Engl J Med 2001;345:941-947.
27. Jones A, Fay JK, Burr M, Stone M, Hood K, Robert G. Inhaled corticosteroid effects on bone metabolism in asthma and mild chronic obstructive pulmonary disease. Cochrane Database Syst Rev 2002;CD003537.
28. Halpern MT, Schmier JK, Van Kerkhove MD, Watkins M, Kalberg CJ. Impact of long-term inhaled corticosteroid therapy on bone mineral density: results of a meta-analysis. Ann Allergy Asthma Immunol 2004;92:201-207; quiz 207-208, 267.
29. Hubbard RB, Smith CJ, Smeeth L, Harrison TW, Tattersfield AE. Inhaled corticosteroids and hip fracture: a population-based case-control study. Am J Respir Crit Care Med 2002;166(12 Pt 1):1563-1566.
30. Lee TA, Weiss KB. Fracture risk associated with inhaled corticosteroid use in chronic obstructive pulmonary disease. Am J Respir Crit Care Med 2004;169:855-859.
31. Suissa S, Baltzan M, Kremer R, Ernst P. Inhaled and nasal corticosteroid use and the risk of fracture. Am J Respir Crit Care Med 2004;169:83-88.
32. Pauwels RA, Yernault JC, Demedts MG, Geusens P. Safety and efficacy of fluticasone and beclomethasone in moderate to severe asthma: Belgian Multicenter Study Group. Am J Respir Crit Care Med 1998;157(3 Pt 1):827-832.
33. Cummings SR, Nevitt MC, Browner WS, Stone K, Fox KM, Ensrud KE, Cauley J, Black D, Vogt TM. Risk factors for hip fracture in white women: study of Osteoporotic Fractures Research Group. N Engl J Med 1995;332:767-773.
34. Law MR, Hackshaw AK. A meta-analysis of cigarette smoking, bone mineral density and risk of hip fracture: recognition of a major effect. BMJ 1997;315:841-846.
35. Biskobing DM. COPD and osteoporosis. Chest 2002;121:609-620.
36. Anthonisen NR, Connett JE, Kiley JP, Altose MD, Bailey WC, Buist AS, Conway WA Jr, Enright PL, Kanner RE, O'Hara P, et al. Effects of smoking intervention and the use of an inhaled anticholinergic bronchodilator on the rate of decline of FEV1. JAMA 1994;272:1497-1505.
37. SAS Institute Inc. SAS/STAT software 1999; version 8.0. Cary, NC: SAS Institute Inc.
38. Marshall D, Johnell O, Wedel H. Mela-analysis of how well measures of bone mineral density predict occurrence of osteoporotic fractures. BMJ 1996;312:1254-1259.
39. Eastell R. Treatment of postmenopausal osteoporosis. N Engl J Med 1998;338:736-746.
40. Ross P, Davis J. Vagel J, Wasnich RD. A critical review of bone mass and the risk of fractures in osteoporosis. Calcif Tissue Int 1990;46:149-161.
41. Allen DB. Limitations of short-term studies in predicting long-term adverse effects of inhaled corticosteroids. Allergy 1999;54:29-34.
42. Laan RF, van Riel PL, van de Putte LB, van Erning LJ, van't Hof MA, Lemmens JA. Low-dose prednisone induces rapid reversible axial bone loss in patients with rheumatoid arthritis: a randomized, controlled study. Ann Intern Med 1993;119:963-968.
43. Saito JK, Davis JW, Wasnich RD, Ross PD. Users of low dose glucocorticoids have increased bone loss rates: a longitudinal study. Calcif Tissue Int 1995;57:115.
44. Lo Cascio V, Bonucci E, Imbimbo B, Ballanti P, Adami S, Milani S, Tartarotti D, DellaRocca C. Bone loss in response to long-term glucocorticoid therapy. Bone Miner 1990;8:39-51.
45. Reid IR, Heap SW. Determinants of vertebral mineral density in patients receiving long term glucocorticoid therapy. Arch Intern Med 1990;150: 2545-2548.
46. Hanania NA, Chapman KR, Sturtridge WC, Szalai JP, Kesten S. Doserelated decrease in bone density among asthmatic patients treated with inhaled corticosleroids. J Allergy Clin Immunol 1995;96(5 Pt 1):571-9, 1995.
47. Seeman E, Wahner HW, Offord KP, Kumar R, Johnson WJ, Riggs BL. Differential effects of endocrine dysfunction on the axial and the appendicular skeleton. J Clin Invest 1982;69:1302-1309.
48. Lipworth BJ. Airway and systemic effects of inhaled corticosteroids in asthma: dose response relationship. Pulm Pharmacol 1996;9:19-27.
49. Brown PH, Matusiewicz SP, Shearing C, Tibi L, Greening AP, Crompton GK. Systemic effects of high dose inhaled steroids: comparison of beclomethasone dipropionate and budesonide in healthy subjects. Thorax 1993;48:967-973.
50. Liu G, Peacock M, Eilam O, Dorulla G, Braunstein E, Johnston CC. Effect of osteoarthritis in the lumbar spine and hip on bone mineral density and diagnosis of osteoporosis in elderly men and women. Osteoporos Int 1997;7:564-569.
51. Peacock DJ, Egger P, Taylor P, Cawley MI, Cooper C. Lateral bone density measurements in osteoarthritis of the lumbar spine. Ann Rheum Dis 1996;55:196-199.
52. Pauwels RA, Buist AS, Calverley PM, Jenkins CR, Hurd SS, GOLD Scientific Committee. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: NHLBI/ WHO Global Initiative for Chronic Obstructive Lung Disease (GOLD) Workshop Summary. Am J Respir Crit Care Med 2001;163: 1256-1276.
53. American Thoracic Society/European Respiratory Society. Standards for the diagnosis and management of patients with COPD: American Thoracic Society/European Respiratory Society COPD Guidelines, 2004. http://www.thoracic.org/copd/ (Accessed June 1, 2004)
54. Smith BJ, Phillips PJ, Heller RF. Asthma and chronic obstructive airway diseases are associated with osteoporosis and fractures: a literature review. Respirology 1999;4:101-109.
55. American College of Rheumatology Task Force on Osteoporosis Guidelines. Recommendations for the prevention and treatment of glucocorticoid-induced osteoporosis. Arthritis Rheum 1996;39:1791-1801.
56. Sambrook PN. Commentary: inhaled corticosteroids, bone density, and the risk of fracture. Lancet 2000;355:1385.
Paul D. Scanlon, John E. Connett, Robert A. Wise, Donald P. Tashkin, Thelma Madhok, Melissa Skeans, Paul C. Carpenter, William C. Bailey, A. Sonia Buist, Michael Eichenhorn, Richard E. Kanner, Gail Weinmann, and the Lung Health Study Research Group
Mayo Clinic, Rochester; University of Minnesota Coordinating Center, Minneapolis, Minnesota; Johns Hopkins University School of Medicine, Baltimore; National Heart, Lung, and Blood Institute, Bethesda, Maryland; University of California, Los Angeles, California; University of Alabama at Birmingham, Birmingham, Alabama; Oregon Health Sciences University, Portland, Oregon; Henry Ford Hospital, Detroit, Michigan; and University of Utah, Salt Lake City, Utah
(Received in original form October 1, 2003; accepted in final form September 13, 2004)
Supported by a cooperative agreement with NIH-NHLBI-5U01-HL50267-05 and by Rhône-Poulenc Rorer, Inc. (now Aventis Pharmaceuticals, Inc.) (Collegeville, PA), who provided the study medication, the placebo, and support for ancillary safety studies.
Correspondence and requests for reprints should be addressed to John E. Connett, Ph.D., Lung Health Study Coordinating Center, 2221 University Ave SE, Suite 200, Minneapolis, MN 55414. E-mail: john-c@blueox.ccbr.umn.edu
Am J Respir Crit Care Med Vol 170. pp 1302-1309, 2004
Originally Published in Press as DOI: 10.1164/rccm.200310-1349OC on September 16, 2004
Internet address: www.atsjournals.org
Conflict of Interest Statement: P.D.S. received funding support for this study from Rhone Poulenc Rorer (now Aventis) and also received (during 2001-2004) research funding from Boehringer Ingelheim, Dey Pharmaceutical, GlaxoSmithKline, LaRoche, and ONO Pharmaceutical, and he received an honorarium from Boehringer Ingelheim for a lecture 2001; J.E.C. was Principal Investigator of a grant from Rhone Poulenc Rorer to support an ancillary study on bone density changes associated with the use of triamcinolone acetonide; R.A.W. received consulting fees from Pfizer between July 1, 2001 and July 1, 2004, and received consulting fees from GlaxoSmithKline in 2003 and 2004 for serving on a mortality review committee and has received research grants from Boehringer Ingelheim between 2002 and 2004 and from Otsuka Medical Research Institute in 2003 and 2004 and from Pfizer in 2003, and he also has pending research grants from AstraZeneca, GlaxoSmithKline, and Boehringer Ingelheim; D.P.T. does not have a financial relationship with a commercial entity that has an interest in the subject of this manuscript; T.M. does not have a financial relationship with a commercial entity that has an interest in the subject of this manuscript; M.S. does not have a financial relationship with a commercial entity that has an interest in the subject of this manuscript; P.C.C. does not have a financial relationship with a commercial entity that has an interest in the subject of this manuscript; W.C.B. has received research contracts from drug companies as sponsors of investigational drug research projects and has received honoraria from pharmaceutical companies for delivering lectures as part of Continuing Medical Education programs for physicians with appropriate disclosure and has grants from the American Lung Association for an Asthma Clinical Research Center and others from the National Institutes of Health, which may occasionally use a therapy/drug from pharmaceutical companies, some of which are GlaxoSmithKline, Schering-Plough, Merck, Inspire, Rhone Poulenc Rorer, Pharmaceutical Dev, Aventis, and Boehringer Ingelheim; A.S.B. does not have a financial relationship with a commercial entity that has an interest in the subject of this manuscript; M.E. does not have a financial relationship with a commercial entity that has an interest in the subject of this manuscript; R.E.K. does not have a financial relationship with a commercial entity that has an interest in the subject of this manuscript; G.W. does not have a financial relationship with a commercial entity that has an interest in the subject of this manuscript.
Acknowledgment: The authors thank Steven Cummings, M.D., Dennis Black, Ph.D., Kristine Ensrud, M.D., and Marc Hochberg, M.D., for assistance in interpretation of bone density results; Mary F. Hauser, M.D., and Heinz W. Wahner, M.D., for assistance with bone density measurements; and Patricia Muldrow for assistance in preparation of the article.
The principal investigators and senior staff of the clinical and coordinating centers, the National Heart, Lung, and Blood Institute, and members of the Safety and Data Monitoring Board are as follows: Case Western Reserve University, Cleveland, OH: M.D. Altose, M.D. (Principal Investigator), S. Redline, M.D. (Co-Principal Investigator), C.D. Deitz, Ph.D., K.J. Quinlan; Henry Ford Hospital, Detroit, MI: M.S. Eichenhorn, M.D., (Principal Investigator), W.A. Conway, M.D. (Co-Principal Investigator), R.L. Jentons, M.A., K. Braden, M. Ketchum; Johns Hopkins University School of Medicine, Baltimore, MD: R.A. Wise, M.D. (Principal Investigator), S. Permutt, M.D. (Co-Principal Investigator), C.S. Rand, Ph.D. (Co-Principal Investigator), M. Daniel, V. Santopietro, K.A. Weeks; Mayo Clinic, Rochester, MN: P.D. Scanlon, M.D. (Principal Investigator), A.M. Patel, M.D. (Co-Principal Investigator), J.P. Utz, M.D. (Co-Principal Investigator), D.E. Williams, M.D. (Co-Principal Investigator), G.M. Caron, K.S. Mieras, L.C. Walters (Bone Density Quality Control Coordinator); Oregon Health Sciences University, Portland, OR: A.S. Buist, M.D. (Principal Investigator), L.R. Johnson, Ph.D. (LHS Pulmonary Function Coordinator), V.J. Bortz, S.L. Persons, H.A. Schueler; University of Alabama at Birmingham, AL: W.C. Bailey, M.D. (Principal Investigator), C.M. Brooks, Ed.D. (Co-Principal Investigator), L.B. Gerald, Ph.D., M.S.P.H. (Co-Principal Investigator), S. Erwin; University of California, Los Angeles, CA: D.P. Tashkin, M.D. (Principal Investigator), A.H. Coulson, Ph.D. (Co-Principal Investigator), B.C. Kleerup, M.D. (Co-Principal Investigator), V.C. Li, Ph.D., M.P.H. (Co-Principal Investigator), M.A. Nides, Ph.D., LP. Zuniga, Y.E. Lee; University of Manitoba, Winnipeg, Manitoba, Canada: N.R. Anthonisen, M.D. (Principal Investigator), J. Manfreda, M.D. (Co-Principal Investigator), S.C. Rempel-Rossum, J.M. Stoyko; University of Minnesota Coordinating Center, Minneapolis, MN: J.E. Connett, Ph.D. (Principal Investigator), M.O. Kjelsberg, Ph.D. (Co-Principal Investigator), MT. Bollenbeck, M.S., K.J. Kurnow, M.S., P.L. Lindgren, M.S., T.C. Madhok, Ph.D., M.A. Skeans, M.S., H.T. Voelker; University of Pittsburgh, Pittsburgh, PA: R.M. Rogers, M.D. (Principal Investigator), G.R. Owens, M.D. (Principal Investigator, deceased), F.M. Vitale, M.A., M.E. Pusateri; University of Utah, Salt Lake City, UT: R.E. Kanner, M.D. (Principal Investigator), G.M. Villegas, C. Esplin, R.S. Stayner; Safety and Data Monitoring Board: R. Bascom, M.D., J.R. Landis, Ph.D., J.R. Maurer, M.D., Y. Phillips, M.D., S.I. Rennard, M.D., J.K. Stoller, M.D., I. Tager, M.D., A. Thomas, Jr., M.D.; National Heart, Lung, and Blood Institute, Bethesda, MD: J.P. Kiley, Ph.D. (Director, Division of Lung Diseases), G. Weinmann, M.D. (Director, Airway Biology & Disease Program; former Project Officer), M.C. Wu, Ph.D. (Division of Epidemiology and Clinical Applications).
Copyright American Thoracic Society Dec 15, 2004
Provided by ProQuest Information and Learning Company. All rights Reserved