A 52-year-old music educator came to us with an 18-month history of intermittent hoarseness, loss of voice, and vocal fatigue in both his speaking and singing voice. He said that his problem was related directly to the heavy vocal demands inherent in his occupation. An earlier period of voice rest over the summer had failed to improve his condition. During his office visit, his voice was hoarse and breathy, and it had a raspy quality.
Strobovideolaryngoscopy revealed mild to moderate edema of the vocal folds and a right vocal fold lesion that was consistent with a subepithelial vocal fold cyst. Flexible laryngoscopy demonstrated supraglottic hyperfunction during connected speech, which is indicative of muscle-tension dysphonia. We prescribed voice therapy. Following completion of this program, the patient was reevaluated. Strobovideolaryngoscopy revealed a scar that involved more than half of the membranous left vocal fold and a cyst on the right vocal fold.
The patient underwent a detailed microlaryngoscopic examination as well as palpation of the vocal folds. Vocal fold scarring was found bilaterally, as well as a small right subepithelial mass that was believed to be either a cyst or a fibrous mass. During microlaryngoscopy, triamcinolone was injected into the subepithelial plane of the left vocal fold with a 27-gauge needle.
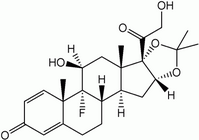
At both the 1-week and 10-month follow-up visits, strobovideolaryngoscopy revealed a white, subepithelial plaque at the site of the triamcinolone injection (figure). The plaque did not have a negative impact on the vibration of the left vocal fold. However, we were initially alarmed by the appearance of this new lesion. The patient was subsequently treated with a fat-graft reconstruction of the left vocal fold and removal of the right vocal fold cyst via a microflap approach. He did well following surgery and has resumed teaching and singing.
[FIGURE OMITTED]
Soon thereafter, we found another patient to have a similar "triamcinolone plaque," and we were advised of a third case by R.T. Sataloff, MD (oral communication, 1999). Since then, we have switched from using triamcinolone to high-concentration (10 mg/ml) dexamethasone when injecting a steroid into the vocal folds. Dexamethasone solution is clear and does not leave any residual deposit. The triamcinolone plaque is believed to be the result of the chalky material present in the triamcinolone solution itself.
Treatment of vocal fold scaring includes both surgical and nonsurgical rehabilitation. (1) The initial treatment of dysphonia associated with vocal fold scarring should be nonsurgical. Patients with dysphonia secondary to vocal fold scarring often demonstrate an associated compensatory muscle-tension dysphonia (secondary). Several different vocal fold injection methods have been advocated for the treatment of vocal fold scars, including steroid injection into the lamina propria. There have been reports that steroid injections improve vocal fold suppleness, vocal fold closure, and voice quality, (2) although success has not been consistent. When this technique is used, the steroid chosen should be aqueous and should not contain components that can form a precipitate.
References
(1.) Rosen CA. Vocal fold scar: Evaluation and treatment. Otolaryngol Clin North Am 2000;33:1081-6.
(2.) Bouchayer M, Cornut G. Microsurgery for benign lesions of the vocal folds. Ear Nose Throat J 1988:67:446-9, 452-4, 456-64.
From the Department of Otolaryngology-Head and Neck Surgery, University of Pittsburgh School of Medicine.
COPYRIGHT 2003 Medquest Communications, LLC
COPYRIGHT 2004 Gale Group