Clinical Scenario
A 60-year-old woman with osteoarthritis of her right knee has pain and swelling despite daily use of nonsteroidal anti-inflammatory drugs (NSAIDs).
Clinical Question
Would this patient benefit from an intraarticular injection of a corticosteroid?
Evidence-Based Answer
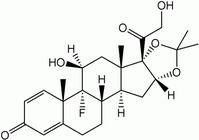
An injection of the knee joint with a corticosteroid may improve the patient's symptoms for up to three weeks after the injection (number needed to treat [NNT]= 3 to 4). There is no evidence that this intervention improves function, and there is little evidence of the benefits persisting beyond three weeks. Risk of dangerous adverse effects is minimal. Injection of hyaluronan and hylan products (Hyalgan, Orthovisc, Synvisc) may provide longer-lasting benefit.
Practice Pointers
This review (1) shows that intra-articular injection of a corticosteroid is useful in improving pain and the patient's global assessment of symptoms for up to three weeks in patients with osteoarthritis of the knee. The analysis was based on 26 trials with a total of 1,721 patients. However, most studies were small and brief, with fewer than 100 participants and a duration of less than 26 weeks. Only good-quality studies that used standardized rheumatologic outcome measures were included in the review. The authors made an adequate attempt to find all relevant articles and combined data using standard techniques.
There are many effective treatments available for mild symptomatic osteoarthritis, including patient education, physical and occupational therapy, oral and topical analgesics, and NSAIDs. (2-4) Nonetheless, many patients still suffer from pain and reduced function despite treatment efforts. Since the 1950s, patients have been given intra-articular corticosteroid injections when other nonsurgical therapies are inadequate. This review did not find strong evidence to support the use of one particular corticosteroid preparation, dose, injection technique, or frequency of injection, but triamcinolone hexacetonide (Aristospan) was superior to betamethasone (Celestone) in the number of patients reporting pain relief at four weeks. The reviewers also found no particular indication (e.g., joint effusion) that would help select patients who are more likely to benefit.
The same authors published a separate review (5) of injection with hyaluronan and hylan derivatives for osteoarthritis of the knee, in which they found this treatment to be effective. The Cochrane Collaboration has elsewhere reviewed corticosteroid injections for shoulder pain, (6) finding weak evidence for a small and short-lived benefit in rotator cuff disease and adhesive capsulitis. The collaboration also has reviewed local injection of corticosteroid for carpal tunnel syndrome (7) and found benefit lasting up to one month. Some evidence-based clinical guidelines (2,4) recommend intra-articular corticosteroid injection for treatment of osteoarthritis of the knee when other, more conservative, treatments are not effective. Several authors have described injection techniques in detail. (8-10) This Cochrane review covers the best and most recent evidence available and supports the use of intra-articular corticosteroids for osteoarthritis of the knee.
The Cochrane Abstract below is a summary of a review from the Cochrane Library. It is accompanied by an interpretation that will help clinicians put evidence into practice. Steven E. Roskos, M.D., presents a clinical scenario and question based on the Cochrane Abstract, followed by an evidence-based answer and a full critique of the review.
EB CME
This clinical content conforms to AAFP criteria for evidence-based continuing medical education (EB CME). EB CME is clinical content presented with practice recommendations supported by evidence that has been reviewed systematically by an AAFP-approved source. The practice recommendations in this activity are available online at http://www.cochrane. org/cochrane/revabstr/ AB005328.htm.
REFERENCES
(1.) Bellamy N, Campbell J, Robinson V, Gee T, Bourne R, Wells G. Intraarticular corticosteroid for treatment of osteoarthritis of the knee. Cochrane Database Syst Rev 2005;(2):CD005328.
(2.) Recommendations for the medical management of osteoarthritis of the hip and knee: 2000 update. American College of Rheumatology Subcommittee on osteoarthritis Guidelines. Arthritis Rheum 2000;43:1905-15.
(3.) Health care guideline: diagnosis and treatment of adult degenerative joint disease (DJD) of the knee. Bloomington, Minn.: Institute for Clinical Systems Improvement, 2004. Accessed online July 13, 2005, at: http://www.icsi.org/knowledge/detail.asp?catID=29&itemID=165.
(4.) Simon LS, Lipman AG, Jacox Ak, Caudill-Slosberg M, Gill LH, Keefe FJ, et al. Pain in osteoarthritis, rheumatoid arthritis, and juvenile chronic arthritis. 2d ed. Glenview, Ill.: American Pain Society, 2002. Summary accessed online July 13, 2005, at: http://www.guideline.gov/summary/ summary.aspx?ss=15&doc_id=3691.
(5.) Bellamy N, Campbell J, Robinson V, Gee T, Bourne R, Wells G. Viscosupplementation for the treatment of osteoarthritis of the knee. Cochrane Database Syst Rev 2005;(2):CD005321.
(6.) Buchbinder R, Green S, Youd JM. Corticosteroid injections for shoulder pain. Cochrane Database Syst Rev 2003;(1):CD004016.
(7.) Marshall S, Tardif G, Ashworth N. Local corticosteroid injection for carpal tunnel syndrome. Cochrane Database Syst Rev 2002;(4): CD001554.
(8.) Cardone DA, Tallia AF. Diagnostic and therapeutic injection of the hip and knee. Am Fam Physician 2003;67:2147-52.
(9.) Greene WB, ed. essentials of musculoskeletal care. 2d ed. Rosemont, Ill.: American Academy of orthopaedic Surgeons, 2001:20-3,371-2.
(10.) Pfenninger JL. Joint and soft tissue aspiration and injection (arthrocentesis). In: Pfenninger JL, Fowler GC, eds. Pfenninger and Fowler's Procedures for primary care. 2d ed. St. Louis: Mosby, 2003:1479-500.
STEVEN E. ROSKOS, M.D., is assistant professor of family medicine at the University of Tennessee, Graduate School of Medicine, Knoxville. He received his medical degree from temple University School of Medicine, Philadelphia, and completed a residency in family medicine at Lancaster General Hospital, Lancaster, Pa.
Address correspondence to Steven E. Roskos, M.D., Department of Family Medicine, University of Tennessee, Graduate School of Medicine, 1924 Alcoa Highway, U-67, Knoxville, TN 37920 (e-mail: sroskos@mc.utmck.edu). Reprints are not available from the author.
STEVEN E. ROSKOS, M.D., University of Tennessee, Graduate School of Medicine, Knoxville, Tennessee
COPYRIGHT 2005 American Academy of Family Physicians
COPYRIGHT 2005 Gale Group