Local steroid injections only reduce inflammation temporarily
EDITOR--I am surprised that the BMJ has published the article by Dammers et al without a public health warning.[1] As an orthopaedic surgeon, I occasionally use local steroid injection as temporary treatment for the carpal tunnel syndrome when operation cannot be carried out promptly. To suggest that patients should be offered steroid injection as definitive treatment, however, is both wrong and irresponsible. Pressure on the median nerve in the medium term can result in permanent damage to the nerve. Local steroid injections do not reduce the pressure on the nerve in the long term; all they do is reduce inflammation temporarily--nerve compression almost always returns, recurrence rates of 800/0 at one year[2] and 87% at 11 months[3] having been reported.
The danger with injections is that the patient feels better, believes that he or she is cured, and does not return to see the doctor for two or three years. Orthopaedic outpatient waiting lists of six months and over in the United Kingdom compound this problem. By this time the thenar muscles may be wasted and numbness of the hand in the distribution of the median nerve may have occurred; at that stage it may not respond to surgical decompression--that is, it is permanent.[4]
Local steroid injections are justified in one specific situation: in the carpal tunnel syndrome associated with pregnancy. These injections are effective in 85% of cases, but in some cases with serious axonal loss surgical release is justified?
W Angus Wallace professor of orthopaedic and accident surgery Queen's Medical Centre, Nottingham NG7 2UH Angus.Wallace@rcsed.ac.uk
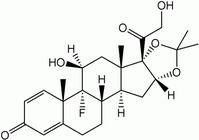
[1] Dammers JWHH, Veering MM, Vermeulen M. Injection with methylprednisolone proximal to the carpal tunnel: randomised double blind trial. BMJ 1999;319:884-6. (2 October.)
[2] Stahl S, Yarnitsky D, Volpin G, Fried A. Conservative therapy in carpal tunnel syndrome. Harefuah 1996;130:241-3.
[3] Weiss AP, Sachar K, Gendreau M. Conservative management of carpal tunnel syndrome: a reexamination of steroid injection and splinting. J Hand Surg [Am] 1994;19:410-5.
[4] Katz JN, Keller RB, Simmons BP, Rogers WD, Bessette L, Fossel AH, et al. Maine carpal tunnel study: outcomes of operative and nonoperative therapy for carpal tunnel syndrome in a community-based cohort. J Hand Surg [Am] 1998;23:697-710.
[5] Seror P. Carpal tunnel syndrome in pregnancy. J Gynecol Obstet Biol Reprod (Paris) 1997;26:148-53. [In French.]
Study does not show long term benefits of injection for the syndrome
EDITOR--Dammers et al's trial shows that, at one month follow up, symptoms of the carpal tunnel syndrome were considerably more likely to have resolved in patients who had received steroid injection than in those injected with a placebo.[1] The study does not, however, provide any evidence to support the suggestion that steroid injection is more effective than placebo after more than three months of follow up. This is because all non-responders were transferred to surgical treatment or steroid injection at either one month or three months' follow up, so we do not know whether their symptoms would have resolved after this.
In the United States DeStefano et al studied 227 patients who were not given surgical treatment (most were treated with splinting and oral analgesics or non-steroidal anti-inflammatory drugs and only six received steroid injection).[2] They found that at one year symptoms had completely resolved in over half of these patients given conservative management. For many patients, though, the response took several months to occur. The 50% response to steroid injection at one year reported by Dammers et al is therefore probably no different from the response that could be achieved by using non-invasive forms of conservative management.
Andrew C Hayward lecturer Division of Public Health and Epidemiology, School of Community Health Sciences, University of Nottingham Medical School, Nottingham NG7 2UH Andrew. Hayward@Nottingham.ac.uk
[1] Dammers JWHH, Veering MM, Vermeulen M. Injection with methylprednisolone proximal to the carpal tunnel: randomised double blind trial. BMJ 1999;319:884-6. (2 October.)
[2] DeStefano F, Nordstrom DL, Vierkant RA. Long-term symptom outcomes of carpal tunnel syndrome and its treatment. J Hand Surg [Am] 1997;22:200-10.
Study is needed to determine best treatment for this syndrome
EDITOR--Dammers et al report that injection of methylprednisolone near the carpal tunnel relieves symptoms of compression.[1] Every general practitioner knows that the carpal tunnel syndrome is a miserable condition that affects many people and may be disabling, so it is a subject well worth studying.
Although the authors mention possible danger from injections into the carpal tunnel itself, they present no evidence that such difficulties are widespread or that such injections are any less effective than other treatments. This was a placebo controlled experiment rather than a trial of different treatments.
Taught from a book, I have been injecting the carpal tunnel to the ulnar side of the palmaris longus tendon at the most distal wrist crease with lignocaine and triamcinolone hexacetonide for over a decade, without difficulty. I have never knowingly caused ill effects and have had apparent long term success in many cases. Our local orthopaedic surgeon seems to use a technique involving an (anecdotally more painful yet no more effective) injection into the hand. Perhaps there are yet other techniques than these three. I do not know whether my injections or those of my orthopaedic colleague do actually go into the carpal tunnel or whether they only go near it.
Practically speaking, those who manage the carpal tunnel syndrome need to know five things:
* which injection site and method are best;
* which preparation (methylprednisolone, hydrocortisone, triamcinolone) and what dose or volume are best;
* whether such procedures are most economically undertaken in general practice, in the orthopaedic clinic, or in neurology outpatient clinics;
* whether clinical diagnosis (as opposed to electrophysiological diagnosis) alone is an adequate basis for injection treatment;
* whether there is any prospective difference (for example, age, underlying cause or precipitant, length of symptomatic period) between patients for whom injections will be curative and patients who will need surgical treatment eventually.
The best site and preparation would have to be decided by reference to the patient's preference, the effectiveness in the short and long term, and the absence or presence of dangerous or unpleasant side effects. It would also be nice to know the scientific basis for the therapeutic effect of such injections.
Disappointingly, Dammers et al do not really help us on any of these points. Perhaps one day someone will organise a systematic study to elucidate the management of this, perhaps neglected, problem.
Tim Davies general practitioner East Street Medical Centre, Littlehampton BN17 6AW TDaviesUK@aol.com
[1] Dammers JWHH, Veering MM, Vermeulen M. Injection with methylprednisolone proximal to the carpal tunnel: randomised double blind trial. BMJ 1999;319:884-6. (2 October.)
Author's reply
EDITOR--Wallace fears a poor outcome for patients with the carpal tunnel syndrome if they receive injections as in our study. He would even like to see a health warning. Recurrences in our study, when they occurred, were usually seen within three months; nine tenths occurred within six months. In almost all patients these recurrences consisted of sensory symptoms. Wasting of thenar muscles is rare (8%) even in patients with long lasting symptoms. The favourable results of our study are probably explained by relief from pressure and not by anti-inflammatory effects as these are of short duration.
Hayward had expected many more spontaneous recoveries in the placebo group, as has been reported in the literature. In our study patients had had symptoms for at least three months; the average duration was over two years before treatment was started.
Davies wishes to know which injection site and method are best. We gave injections proximal to the carpal tunnel to avoid damage of the nerve as well. Possibly because of this our results are better than those that have been reported for other injection sites. After having read Davies's letter we expect that he will soon start a randomised study comparing different doses of methylprednisolone, injected, as is usual in Alkmaar, proximal to the carpal tunnel.
J W H H Dammers neurologist Medisch Centrum Alkmaar, Postbus 501, 1800 AM Alkmaar, Netherlands J.Dammers@mca.alkmaar.nl
COPYRIGHT 2000 British Medical Association
COPYRIGHT 2000 Gale Group