Biocides (antiseptics, disinfectants, preservatives, sterilants) are used in clinical medicine as intervention strategies that prevent the dissemination of nosocomial pathogens. Biocides are also used for personal hygiene and to prevent cross-contamination of food-borne pathogens in homes, restaurants, day care centers, and nursing homes. However, laboratory evidence has emerged suggesting that the mechanism of nonsusceptibility to biocides may counter-select for resistance to antibiotics. Nature conserves successful survival strategies. Using existing mechanisms of resistance to antibiotics and their means of dissemination, microorganisms have adopted this same survival strategy for biocide nonsusceptibility. These mechanisms are intrinsic in nature or are acquired. The consequences to biocide efficacy in the clinical setting are probably not significant from the biocide perspective. But, the selective pressure biocides exert on bacterial populations that have mechanisms of resistance similar to those to antibiotics or that are also substrates for antibiotic resistance is of concern.
ABBREVIATIONS: CM = cytoplasmic membrane; LPS = lipopolysaccharides; MRSA = methicillin-resistant Staphylococcus aureus; OM = outer membrane; PG = peptidoglycan; PMF = proton motive force; RND = resistance-nodulation-division.
INDEX TERMS: biocide, biofilm, efflux, mechanism of action.
Clin Lab Sci 2005;18(3):181
LEARNING OBJECTIVES
1. Identify the mechanism of action and targets of antiseptics.
2. Discuss the mechanisms of resistance to antiseptics.
3. Describe the intrinsic and acquired mechanisms of antiseptic nonsusceptibility.
4. Discuss the mechanisms used to disseminate resistant determinants of antiseptics.
Semmelweis's mandate that physicians wash examining fingers with chlorine to prevent puerperal (childbed) fever provided the scientific evidence to justify the use of biocides in the practice of medicine.1 Biocides (antiseptics, disinfectants, preservatives, and sterilants) are now an integral component in the practice of clinical medicine and serve primarily to prevent the dissemination of nosocomial pathogens in the hospital environment.2 Antiseptics are used as surgical hand scrubs, healthcare personnel hand washes, preoperative skin preparations, and total body washes. Biocides are also used in vascular catheter-care site preparation and are impregnated into catheters to prevent catheter related blood stream infections.3-5 Disinfectants are used to decontaminate or sterilize medical instruments and patient care items, while preservatives are used to prevent the growth of organisms in multi-use medical products, although not always successfully.5,7 Biocides are also used in homes, restaurants, day care centers, and nursing homes for personal hygiene and to prevent cross-contamination of food-borne pathogens.8,9 Intended use of biocides in these settings are not unlike those in the clinical setting: to prevent the dissemination of potential pathogens. However, as with antibiotics, increased use of biocides may contribute to the emergence and/or selection of pathogens less susceptible to biocides and resistant to antibiotics.10,11 These observations suggest that antiseptics and antibiotics have common mechanisms of action and possible resistance.
The present article discusses the mechanisms by which biocides exert their biological effect, mechanisms that influence their biological activity, and the possible consequences of these mechanisms in the clinical setting. Although the use of biocides in homes, restaurants, day care centers, and nursing homes is not discussed, the principles discussed regarding the use of biocides in clinical environments are generally applicable to the other environments since their strategic use is the same: the prevention of the dissemination of pathogens.12-14
BIOCIDE MECHANISMS OF ACTION
Biocide mechanisms of action are determined using the same methods used in the evaluation of the action of antibiotics. These methods include evaluation of the effects on intracellular components such as interactions with macromolecules and their biosynthetic processes, inhibition of oxidative phosphorylation, and interference with enzymes and electron transport. They also include effects upon membranes such as microscopic examination of cells exposed to biocides; effects on model membranes; and examination of uptake, lysis, and leakage of intracellular components.15 Since the methods used to assess the mechanism of action include evaluation of their effects on the membrane and intracellular components, these targets are used ill our discussion. Although the antimicrobial spectrum of activity and efficacy of biocides is well documented, complete characterization of their mechanisms of action, especially at low concentrations, is lacking. Detailed discussions of the mechanisms of action of biocides are presented elsewhere.15,16
The cell wall of gram-positive bacteria is composed of a cytoplasmic membrane (CM), which overlies the cytoplasm and a thick peptidoglycan (PG) outer layer. Gram-negative bacteria add an outer membrane (OM), composed of lipopolysaccharides (LPS), lipoproteins, and proteins, separated from the CM by a periplasmic space.17
In gram-negative bacteria, the OM is critical in maintaining the cell wall's integrity as a permeability barrier. The core region of the LPS is negatively charged, impeding permeability and reducing susceptibility to negatively charged antiseptics. Gram-negative bacteria are less sensitive to biocides than gram-positive bacteria because of the LPS layer. Anionic biocides, such as chlorhexidine, neutralize the negative charge and mediate changes in hydrophobicity of the OM thereby promoting uptake. Aldehydes such as glutaraldehyde, interact principally with OM lipoproteins by cross-linking with unprotonated amines resulting in loss of cell wall function. Cross-linking with thiol, sulphydryl, and amino groups also results in inhibition of protein, DNA, and RNA synthesis.16,18,19
Biocides also disrupt the CM by dissipating the proton motive force (PMF) of efflux pumps, and interacting with CM enzymes.16 The PMF is a proton gradient across the CM that develops when the extracellular concentration of protons (H+) is greater than the intracellular concentration. Efflux pumps use the PMF by coupling biocide efflux to the counterflow of protons.16 Quaternary ammonium compounds and biguanides are thought to combine with CM phospholipids causing disruption and leakage of intracellular components.20,21 Biocide mediated inactivation of CM proteins also occurs by inhibition of the electron transport chain and rapid denaturing of proteins.22,23 Once biocides penetrate the CM, they reach and inhibit the cellular anabolic functions by interacting with DNA, RNA, and proteins.24,25 The interaction includes cross-linking of thiol, sulphydryl, and amino groups by aldehydes; reactions with cysteine and methionine thiol groups of proteins and nucleotides by iodine; and sulfhydryl groups and double bonds by hydrogen peroxide.15,16
Thus biocides, unlike antibiotics, have multiple targets within the microbial cell. This multiple target effect is thought to contribute to their bactericidal activity and dictates against the emergence of resistance. However, recent studies suggest that mutation or overexpression of triclosan and chlorhexidine target sites produces nonsusceptible microorganisms.14,2629 These studies suggest that if an antibiotic and antiseptic have a similar mode of action, an organism with reduced susceptibility to the antiseptic may also exhibit resistance to the antibiotic. For instance, in Escherichia coli and Mycobacterium smegmatis, triclosan binds enoyl-acyl protein reductase, an enzyme involved in fatty acid synthesis.26 Certain strains of M. smegmatis have missense mutations in enoyl reductase genes; they demonstrate decreased susceptibility to triclosan as determined by minimum inhibitory concentration studies and also exhibit resistance to the antituberculosis drug isoniazid.30 Conversely, a resistant strain originally selected on isoniazid is found to be triclosan non-susceptible. These studies point out a potentially disturbing clinical issue; if both the antiseptic and the antibiotic act on the same target site, then use of either compound may select for and confer resistance to the other.
In prior sections and the remainder of this article, the term nonsusceptible is used instead of resistance to describe the action of biocides. In the clinical setting, the term resistant is frequently used with antibiotics and suggests that an organism exhibiting this phenotype is likely to result in clinical failure when the antibiotic is used. Currently, biocide susceptibility testing is performed with the methods developed for susceptibility testing of a systemic antibiotic. The interpretation of results may not correlate with the clinical efficacy of the biocide. Thus, to describe a microorganism as resistant to a biocide from susceptibility data derived in this manner does not parallel resistance to a systemic antibiotic. At present, interpretative criteria are not necessary for biocides and topical antimicrobial therapies because the concentrations used in clinical practice are substantially greater than the susceptibilty of pathogens to the biocide or antimicrobial.
In this review and for reasons previously discussed, nonsusceptibility to biocides, instead of resistance, is used to describe microorganisms not conforming to the susceptibility patterns of wild-type populations. Although the microorganisms are characterized as nonsusceptible by in vitro testing and molecular methods, microorganisms appear to remain susceptible to approved concentrations of biocides when used as directed in the product label. Regulatory agencies use in vitro and surrogate clinical simulation studies that mimic use conditions to assess the efficacy of topical antiseptics. However, the ability of these surrogate tests to predict efficacy in clinical settings requires validation with clinical trials.31
MECHANISMS OF NONSUSCEPTIBILITY TO BIOCIDES
Antiseptic nonsusceptibility mechanisms may be conveniently divided into intrinsic and acquired.8,15,32
Intrinsic nonsusceptibility to biocides
Intrinsic nonsusceptibility is mediated by impermeability; efflux, particularly in gram-negative bacteria; biofilms ; and enzyme inactivation. Impermeability is influenced by the composition of the cell wall and physiologic adaptation of the microorganism to its environmant.8 Among bacteria, biocide sensitivity is based on the permeability of the biocide through the cell wall, gram-positive bacteria being more sensitive to biocides, followed by mycobacteria and gram-negative bacteria, the least sensitive.33
Gram-negative bacteria are generally less susceptible to biocides because of their complex cell wall, which is composed of the inner CM and associated efflux pumps, peptidoglycan, and an OM with associated LPS components. The OM also contains hydrophilic channels, porins that regulate the passage of solutes.34 The main component responsible for the impermeability of the OM is the LPS. Change in cell wall expression or structure leads to increased nonsusceptibility of gram-negative bacteria to biocides.33 LPS is the primary barrier to the penetration by hydrophobic molecules to the phospholipids and to the cell interior. Pseudomonas aeruginosa and Providentiel stuartii show high-level nonsusceptibility to biocides. This capability may be associated with differences in LPS composition and cation content in the OM, and subtle changes within the structural envelope, respectively.35,36 In addition, hydrophilic molecules pass readily into gramnegative bacteria but exposure of P. aeruginosa and E. coli to biocides results in porin loss and subsequent decreased susceptibility to biocides.34
Efflux pumps are transporter proteins involved in the removal of toxic substances from the interior as discussed in the companion article on antibiotic resistance. Efflux pumps are found in gram-positive and gram-negative bacteria and are specific for a single drug or substrate while others are capable of transporting multiple substrates. Multidrug efflux pumps showing wide specificity to biocides, dyes, detergents, and antibiotics are found in gram-negative bacteria.37 In E. coli, the Acr AB efflux system belongs to the multidrug efBux system family, resistance-nodulation-division (RND), and acts as a transporter of a range of biocides and antibiotic substrates. Upregulation of acrAB is mostly a property of the multiple antibiotic resistance activator (MarA). Environmental stimuli can increase expression of MarA resulting in elevated levels resulting in nonsusceptibility.37 Biocides such as pine oil stimulate reduced susceptibility not only to pine oil but also to clinically useful antibiotics. Mutations found in the multiple antibiotic resistance represser (MarR), allow expression of MarA and activation of the efflux pump acrAB resulting in reduced susceptibility not only to pine oil but also to triclosan.37,38
Physiologic adaptation resulting in noiisusccptiblity to biocides is usually encountered as a biofilm in the clinical setting especially with indwelling medical devices or contaminated products.39 A biofilm is a microbiological community of sessile organisms irreversibly attached to a surface and embedded in a self-produced polymeric extracellular matrix. The organisms of a biofilm exhibit an altered growth rate.39 The nonsusceptibility of bacteria in biofilms to biocides is caused by numerous factors including nutrient depletion within the biofilm resulting in altered growth rates, binding of the biocide to the biofilm, and neutralization or degradation of the biocide.39
Degradation or inactivation, via enzymatic mechanisms, has been reported for formaldehyde, chlorhexidine, and quaternary ammonium compounds but at concentrations below those used in clinical practice.8,12 Thus the clinical significance of this mechanism may be its importance in selecting bacterial species capable of hyperexpressing these enzymes and serving as reservoirs for their dissemination if plasmid mediated.
Acquired nonsusceptibility to biocides
Acquired nonsusceptibility to biocides can occur by mutation of target site, overexpression of the target site, and plasmid mediated efflux.8,9,15
In gram-negative bacteria, studies that describe changes in permeability leading to acquired biocide nonsusceptibility suggest target site mutation.38 Although the changes leading to biocide nonsusceptibility have not been fully characterized at the genetic or molecular level, the phenotypic observations described suggest changes in the outer membrane fatty acid and protein composition, ultrastructure, and surface hydrophobicity.19,39
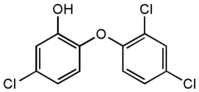
Studies with triclosan, a bis-phenol found in many products, describe a defined target site, and by mutation or hyperproduction of this site, non-susceptible microorganisms are isolated.14,40-42 In E. coli, triclosan binds enoyl-acyl protein reductase (Fab1), an enzyme involved in fatty acid synthesis.43 A similar mechanism of action is described for M. smegmatis, where strains with enoyl reductase missense mutations have decreased susceptibility to triclosan and resistance to the antituberculosis drug isoniazid.30 Conversely, the same study found that a resistant strain originally selected on isoniazid was also triclosan non-susceptible. These studies provide evidence that the antiseptic and the antibiotic act on the same target site and the emergence of resistance to one compound counter-selects for resistance to the other compound.
As previously discussed, efflux pumps can mediate intrinsic nonsusceptiblity to biocides. In addition, studies reveal a mechanism of enhanced nonsusceptibility to antiseptics mediated by overexpression or mutation of regulatory regions of genes of multidrug efflux pumps.44-46 Mutation of the represser/operator region controlling efflux pump gene expression (MarA), or mutation of the efflux pump structural gene, results in either enhanced efflux or reduced affinity to the tantiseptic for the efflux pump.44,45 Efflux is responsible for low-level nonsusceptibility to cationic biocides in antibiotic resistant cocci and in gram-negative bacteria.
Plasmid-associated nonsusceptibility in staphylococci has been demonstrated for cationic biocides such as chlorhexidine gluconate and quaternary ammonium compounds.11,15 S. aureus and coagulase-negative staphylococci isolated from human and veterinary sources were evaluated and shown to carry multidrug resistant plasmids conferring nonsusceptibility to biocides and antibiotics.47-49 The qacA, B, C, and D genes encoding multidrug efflux pumps mediated the nonsusceptibility. The multidrug resistant determinants qacA-G encode proton-dependent export proteins and have significant homology to other energy dependent transporters such as those found in tetracycline exporter mediated resistance.12 Although evidence of plasmid-borne biocide resistance in gram-negative bacteria is limited, plasmid-encoded changes suggest alterations of the OM proteins, and composition of the OM LPS and reduced expression of porins.12
Consequences of reduced susceptibility to biocides
The nonsusceptibility of microorganisms to biocides and the targets some biocides share with antibiotics is of clinical concern because antibiotics are important armaments in the treatment of disease. The concern is primarily the use of biocides in non-clinical environments and the impact such use has on the selection of pathogens cross-resistant to therapeutically useful antibiotics.10,14,50 There are two distinct issues that arise from these observations. The first is whether the development of nonsusceptibility to biocides by nosocomial pathogens, skin flora, and other microorganisms results in decreased efficacy of the topical biocides used in homes, restaurants, day care centers, nursing homes, and healthcare settings. Biocides, when used as disinfectants and sterilants, are used at concentrations substantially higher than levels required to show bactericidal effects. Concentrations of skin antiseptics and preservatives, although lower than disinfectants and sterilants, also demonstrate bacteriostatic and bactericidal effects versus nonsusceptible vegetative pathogens. Although mechanisms resulting in nonsusceptibility to biocides are observed in laboratory studies, clinical evidence has not emerged that combinations of intrinsic and acquired mechanisms of nonsusceptiblity result in clinical failure of biocides when used at recommended concentrations.51 However, we must consider that biocide concentration decreases to sub-therapeutic concentration as we progress away from their point of use and this may provide the environment and selective pressure for nonsusceptible microorganisms.
The second issue is the consequence to the medical community of biocides that select for nonsusceptible microorganisms that are cross-resistant to antibiotics.10,11,14,51 If biocide nonsusceptible organisms that are cross resistant to important antibiotics emerge in clinical and domicile environments, we create an undesirable outcome: a microorganism that may not be treatable in the clinical setting. The use of the biocide triclosan in the domicile environment may explain the emergence of community acquired methicillin-resistant S. aureus (caMRSA).10,14 The emergence of caMRSA is not associated with the risk factors normally seen in the emergence of antibiotic resistance and suggests that other, previously unidentified risk factors, such as use of triclosan, may be responsible.'51 Since triclosan is also used in the clinical environment, the in vitro susceptibility of methicillin-resistant S. aureus and S. epidermidis to triclosan suggests that MRSA isolates do not have higher minimum inhibitory concentrations (MICs) to triclosan when compared to wild-type populations. However, S. epidermidis does, suggesting a possible association between the use of triclosan and selection for a nonsusceptible subpopulation.52,53 Thus, the in vitro observations do not support the proposed hypothesis.
Clearly, nature is conservative in the application of strategies that enhance survival of living organisms. Therefore, it is reasonable to expect that existing survival strategies, e.g., antibiotic resistance, may be applicable to other toxic molecules, e.g., biocides encountered by microorganisms. Mutants of M. smegmatis, whether selected on triclosan or isoniazid, showed cross-resistance to both drugs via mutation of the inhA gene.30 The published literature suggests that microorganisms adapt the same strategies in dealing with the toxic effects of antibiotics and biocides. For example, the same mechanisms that mediate resistance to antibiotics, i.e., efflux, changes in target site, and impermeability are the mechanisms used to produce nonsusceptibility to biocides.8,12,15,30,40
In addition, mechanisms mediating nonsusceptibility by efflux i.e., qacA-G, are found on plasmids; the same evolutionary strategy used by bacteria to disseminate antibiotic resistant determinants.48,49 From the pathogens' perspective, die acquisition of plasmids mediating biocide nonsusceptibility and antibiotic resistance is a desirable survival strategy. These parallels between nonsusceptibility to biocides and antibiotic resistance demonstrate that evolution is a conservative yet dynamic process and when successful strategies evolve, microorganisms adapt these strategies to counter toxic environments. Thus, it is logical that if the mechanism of action of the antibiotic and the antiseptic are the same, cross-resistance is likely to occur. In addition, if the biocide and antibiotic resistant determinants are resident in the same host, then exposure of the host to either the biocide or the antibiotic counter-select for the other mechanism.
There is concern that inappropriate use of biocides may result in the selection of antibiotic resistant pathogens. Increased selection pressure by antibiotics and biocides will result in population shifts to less susceptible organisms. But, we must also realize the importance of biocide use in the clinical and domicile environments. Semmelweis documented the importance of antiseptics in clinical medicine; the importance of biocides in the domicile environment remains to be determined. The current debate appears to focus on the justification for the prevalence of biocide containing products in domicile environments and the consequences such uses may have on selection of antibiotic resistant resident and transient microorganisms. Laboratory studies have shown the potential for cross-resistance between antiseptics and some antibiotics, prompting professional organizations to question the benefit of antimicrobial impregnated household products, and to warn of potential for the emergence of antiseptic mediated resistance to useful antibiotics.54,55 Implied in this concern is acknowledgement that biocides are an important and critical component of the practice of medicine and the healthcare community. As with antibiotics, we must use biocides in a conservative and beneficial manner to assure their continued usefulness.
CONCLUSION
Biocides are an integral and necessary component of the clinical strategy used to prevent the dissemination of nosocomial infections in the clinical community. Their efficacy is well documented. Unlike antibiotics, the mechanism of action of biocides remains poorly characterized. The published literature accepts that biocides have multiple target sites with use concentrations resulting in bactericidal effects. However, the use of subtherapeutic concentrations may allow the identification of specific targets. Characterization of the target sites is necessary to understand whether single target sites exist and the relationship of these targets in the selection of resistance to important antibiotics. In addition, surveillance studies are needed to understand the prevalence of mechanisms of nonsusceptibility to biocides in the microbial community. By applying the same epidemiological tools used to monitor antibiotic resistance to monitor changing susceptibility patterns to biocides, we can then make reasonable risk/benefit decisions regarding the potential implications of biocide use and the emergence of antibiotic resistance.
REFERENCES
1. Semmelweis IP. The etiology, concept, prevention of childbed fever. Reprinted Amer J Obstet Gynecol 1995;172 (1 pt1):236-7.
2. Rutala WA, Weber DJ. Control: the role of disinfectants and sterilization. J Hosp Infect 1999;43:S43-S55.
3. Chalyakunapruk N, Vcenstra DL, Lipsky BA, and others. Chlorhexidine compared with povidone-iodine solution for vascular catheter-site care: a meta analysis. Ann Intern Med 2001;136:792-801.
4. Veenstra DL, Saint S, Saha S, and others. Efficacy of antiseptic-impregnated central venous catheters in preventing catheter related bloodstream infections. JAMA 1999;281:261-7.
5. Kinitons B, Mimoz O, Lafeni L, and others. Chlorhexidine versus povidone iodine in preventing colonization of continuous epidural catheters in children. Anesthesiology 2001;94:239-44.
6. Rutala WA, Weber DJ. Infection control: the tole of disinfection and sterilization. J Hosp Infect 1999;43:S43-S55.
7. Nakashima AK, Highsmith AK, Martone B. Survival of Serratia marcescens in benzalkonium chloride and in multi-dose medication vials: relationship to epidemic septic arthritis. J Clin Microbiol 1987;25:1019-21.
8. International Scientific Forum on Home Hygiene (IFH). Microbial resistance and biocides: a review by the International Scientific Forum on Home Hygiene. Available at http://www. ifh-homehygiene.org/2003/2public/antresFINAL.pdf. Accessed October 18, 2003.
9. International Scientific Forum on Home Hygiene (IFH). Biocide usage and antimicrobial resistance in home settings: an update, a review by the International Scientific Forum on Home Hygiene. Available at http://www.ifh-homehygiene.org/2003/2public/ antres_update.doc. Accessed October 18, 2003.
10. Levy SB. Antibiotic and antiseptic tesistance: impact on public health. Pediatr Infect Dis. 2000;19:S120-S2.
11. Russell AD. Do biocides select for antibiotic resistance? J Pharm Pharmacol 2000;52:227-33.
12. Gilbert P, McBain AJ. Potential impact of increased use of biocides in consumer products on prevalence of antibiotic resistance. Clin Microbiol Rev 2003;16:189-208.
13. Cole EC, Addison RM, and others. Investigation of antibiotic and antibacterial agent cross-resistance in target bacteria from homes of bacterial users and nonusers. J Appl Microbiol 2003; 95:664-76.
14. Levy SB. Antibacterial household products: cause for concern. Emerging Infect Dis 2002;7:512-5.
15. McDonnell G, Russell AD. Antiseptics and disinfectants: activity, action, and resistance. Clin Microbiol Rev 1999;12:147-79.
16. Maillard, J-Y. Bacterial target sites for biocide action. J Appl Microbiol Symposium 2002;92:16S-27S.
17. Walsh C. Antibiotics that act on cell wall biosynthesis. In: Antibiotics actions, origins, resistance. Washington DC: American Society for Microbiology; 2003. p 23-49.
18. Jones DS, German SP, McCafferty DF, and others. The effects of three non-antibiotic antimicrobial agents on the surface hydrophobicity of certain microorganisms evaluated by different methods. J Bacteriol 1991 ;71:218-27.
19. Gorman SP, Scott EM, Russell AD. Antimicrobial activity, uses and mechanisms of action of glutaraldehydes. J Bacteriol 1980:48:161-90.
20. Tattawasart U, Maillard J-Y, Furr, JR, and others. Comparative response of Pseudomonas aeruginosa to antibacterial agents. J Appl Microbiol 1999;87:323-32.
21. Demon GE. Chlorhexidine. In: Block SS, editor. Disinfection, sterilization, and preservation. Philadelphia PA: Lea & Febiger; 1991. p 274-89.
22. Joswick HL, Corner TL, Silvernale JN, and others. Antimicrobial action of hexachlorophene: release of cytoplasmic materials. J Bacteriol 1971; 108:492-500.
23. Larson EI, Morton HE. Alcohols. In: Block SS, editor. Disinfection, sterilization, and preservation. Philadelphia PA: Lea & Febiger; 1991. p 191-203.
24. McGucken PV, Woodside W. Studies on the mode of action of glutaraldehydes on Escherichia colt. J Appl Bacteriol 1973;36:419-26.
25. Stewart GSAB, Jassim AS, Denyer SP. Mechanisms of action and rapid biocide testing. Soc Appl Bacteriol Tech Ser 1991;27:319-29.
26. McMurry LM, Oethinger M, Levy SB. Triclosan targets lipid synthesis. Nature 1998;394:531-2.
27. Heath RJ, You YT, Shapiro MA, and others. Broad-spectrum antimicrobial biocides target the FabI component of fatty acid synthesis. J Biol Chem 1998;273:30316-20.
28. Satstzu M, Shimizu K, Kono N. Triclosan-resistant Staphylococcus aureus (letter) Lancet 1993;341:20.
29. Tattawasart U, Maillard J-Y, Furr JR, and others. Development of chlorhexidine and antibiotic resistance in Pseudomonas stutzeri. Proceedings of the 98th General Meeting of the American Society for Microbiology. 1999. p 533.
30. McMurry LM, McDermott PF, Levy SB. Genetic evidence that InhA of Mycobacterium smegmatis is a target for triclosan. Antimicrob Ag Chemother 1999;43:711-13.
31. Sheldon, AT. Food and Drug Administration perspective on topical antiseptic drug product development. In: Paulson DS. Handbook of topical antimicrobials: industrial applications in consumer products and pharmaceuticals. Marcel Dekker Inc: 2003. 19-48.
32. Russell AD, Chopra I. Understanding antibacterial action and resistance. 2nd ed. Chichester: Ellis Horwood 1996.
33. Lambert PA. Cellular impermeability and uptake of biocides and antibiotic in gram-positive bacteria and mycobacteria. J Appl Microbiol Symposium 2002;92:46S-54S.
34. Denyer SP, Maillard JY. Cellular impermeability and uptake of biocides and antibiotics in gram-negative bacteria. J Appl Microbiol Symp 2002;92:35S-45S.
35. Brown MRW. The role of the cell envelope in resistance. In: Brown MRW, editor. Resistance of Pseudomonas aeruginosa. Chichester, UK: John Wiley & Sons Ltd; 1975. p 71-99.
36. Ismaeel N, El-Mong T, Furr JR, and others. Resistance of Providencia stuartii to chlorhexidine: a consideration of the role of the inner membrane. J Appl Bacteriol 1986;60:361-7.
37. Alekshum MN, Levy SB. The Escherichia coli mar locus-antibiotic resistance and more. ASM News. 2004;70:451-6.
38. Poole, K. Mechanisms of bacterial biocide and antibiotic resistance. J Appl Microbiol Symp 2002;55S-64S.
39. Donlan RM, Costerton JW Biofilms: survival mechanisms of clinically relevant microorganisms. Clin Microbiol Rev 2002;15:167-93.
40. Satstzu M, Shimizu K, Kono N. Triclosan-resistant Staphylococcus aureus (letter). Lancet 1993;341:20.
41. Tattawasart U, Maillard J-Y, Furr JR, and others. Development of chlorhexidine and antibiotic resistance in Pseudomonas stutzeri. Proceedings of the 98th General Meeting of the American Society for Microbiology 1999. p 533.
42. Russell AD. Whither triclosan? J Antimicrob Chemother 2004;53:693-5.
43. McMurry LM, Oethinger M, Levy SB. Triclosan targets lipid synthesis. Nature 1998;394:531-2.
44. Moken MC, McMurry LM, Levy SB. Selection of multipleantibiotic resistant (Mar) mutants of Escherichia coli by using the disinfectant pine oil: roles of the mar and acrAB locus. Antimicrob Ag Chemother 1997;41:2270-2.
45. McMurry LM, Oethinger M, Levy SB. Overexpression on marA, soxS, or acrAB produces resistance to triclosan. In: Laboratory and clinical strains of E. coli FEMS Micro Letter. 1998;166:305-9.
46. Chuanchuen R, Schweizer H. Multidrug efflux pumps and triclosan resistance in Pseudomonas aeruginosa. Proceedings of the 100th General Meeting of the American Society for Microbiology 2000. p A-31.
47. Yamamoto T, Tamura Y, Yokota T. Antiseptic and antibiotic resistance plasmids in Staphylococcus aureus that possess ability to confer chlorhexidine and acrinol resistance. Antimicrob Ag Chemother. 1988;32:932-5.
48. Mayer S, Boos M, Beyer A, and others. Distribution of the antiseptic resistance genes qacA, qacB and qacC in 497 methicillin-resistant and -susceptible European isolates of Staphylococcus aureus. J Antimicrob Chemother 2001;47:896-907.
49. Anthonisen I-L, Sunde M, Steiunm TM, and others. Organization of the antiseptic resistance gene qacA and Tn552-related β-lactamase genes in multidrug-resistant Staphylococcus haemolyticus strains of animal and human origins. Antimicrob Ag Chemother 2002;46:3606-12.
50. Aiello AE, Larson E Antibacterial cleansing and hygiene products as an emerging risk factor for antibiotic resistance in the community. Lancet 2003;3:501-6.
51. Cookson BD, Bolton MC, Platt JH. Chlorhexidine resistance in methicillin-resistant Staphylococcus aureus or just an elevated MIC? An in vitro and in vivo assessment. Antimicrob Ag Chemother 1991;35:1997-2002.
52. Al-Door Z, Morrison D, Edwards, G, and others. Susceptibility of MRSA to triclosan. J Antimicrob Chemother 2003;51:185-6.
53. Schmid MB, Kaplan N. Reduced triclosan susceptibility in methicillin-resistant Staphylococcus aureus. Antimicrob Ag Chemother 2004;48:1397-9.
54. The use of antimicrobial household products: APIC 1997 Guidelines Committee Position Statement. APIC News 1997;6:13.
55. Use of antimicrobials in consumer products (Resolution 506, A-99). Report of the Council on Scientific Affairs. American Medical Association House of Delegates. AAPHP News-Fall 1999.
Albert T Sheldon Jr PhD is President, Antibiotics and Antiseptic Consultants Inc, Silver Spring MD.
Address for correspondence: Albert T Sheldon Jr PhD, President, Antibiotic and Antiseptic Consultants Inc, (AAC), 8206 Queen Annes Drive, Silver Spring MD 20910. (301) 920-1902. ATSheldon@Starpower.net
Connie Mahon MS CLS is the Focus: Antimicrobial Resistance guest editor.
Focus Continuing Education Credit: see pages 188 to 191 for learning objectives, test questions, and application form.
Albert T Sheldon Jr is an employee of Antibiotic and Antiseptic Consultants Inc and as such has no financial holdings and receives no financial support from any manufacturers. The views and opinions expressed in this publication are the author's.
Copyright American Society for Clinical Laboratory Science Summer 2005
Provided by ProQuest Information and Learning Company. All rights Reserved