BOSTON -- Managing bipolar disorder during pregnancy requires balancing the competing risks and benefits to the woman and her fetus, said Adele Viguera, M.D.
"Pregnancy, and particularly the postpartum period, is associated with a high risk of disease recurrence for women with bipolar disorder," said Dr. Viguera, director of the perinatal and reproductive psychiatry program at Massachusetts General Hospital in Boston. Although mood-stabilizing drugs can reduce this risk, most are associated with some degree of teratogenicity, she said.
Limited data exist to support the use in pregnancy of the mood stabilizers most commonly used to treat bipolar disorder.
In addition, mood stabilizers have been shown to increase the risk of certain types of birth defects or congenital malformations in infants who were exposed in utero, Dr. Viguera said during a meeting on bipolar disorder sponsored by Harvard Medical School.
To minimize the possibility of fetal damage, some women choose to discontinue their mood-stabilizing regimen, which itself markedly increases the risk of disease recurrence during pregnancy as well as postpartum illness. "More than half of women who discontinue treatment before or during pregnancy relapse, most frequently in the first trimester," Dr. Viguera said.
The risks associated with treatment and treatment cessation vary considerably, depending on the nature and degree of illness and the agents used to treat it. "There is no single optimal management approach," Dr. Viguera said. "Clinical management requires ongoing assessment of maternal and fetal status, risks, and benefits."
Further complicating management is the fact that the Food and Drug Administration has not approved for use during pregnancy any of the psychotropic medications used to treat bipolar disease, because these agents diffuse across the placenta. The risk of birth defects depends on the drug used, when exposure occurs, and the duration of the exposure. It is generally understood that the highest risk to the fetus is during the first trimester, "but later exposure can also lead to malformations, behavioral effects, low birth weight, and preterm delivery," Dr. Viguera said.
Women with bipolar disorder who have been stable for many years may be able to slowly decrease their medication dosage and stop using the medication before conception.
If symptoms develop during the first trimester, these women may be able to avoid using a mood stabilizer by treating some of the more troubling symptoms, such as irritability, insomnia, and hypomania, with an antipsychotic agent such as haloperidol or perphenazine. If symptoms appear after the first trimester, the mood stabilizer can be reintroduced with less risk of congenital malformation, Dr. Viguera said.
Among women who choose to continue a mood stabilizer during pregnancy to minimize the risk of recurrence, lithium appears to be the safest option. However, it is associated with a relatively small increased risk of a serious cardiac malformation.
Valproic acid, on the other hand, is associated with a 3%-5% risk of a neural tube defect and an 8.9% risk for all anomalies, compared with a baseline rate of 2%-4%.
The risk of bipolar relapse during the postpartum period is very high, as is the risk for postpartum psychosis among women with bipolar disorder. Consequently, medication prophylaxis generally is recommended, although there is some debate on timing, Dr. Viguera said.
"The goal is to maintain euthymia by reintroducing the mood stabilizer early," she said. Some studies have shown benefits to reintroducing the drug in the third trimester, and other studies have suggested 24-48 hours post partum. In any case, Dr. Viguera said, "the post partum treatment plan should be addressed in advance."
RELATED ARTICLE: Treating Bipolar Issues in Pregnancy
Following are some drugs commonly used to treat the symptoms of bipolar disorder during pregnancy:
* Lithium. Although effective in only a limited number of patients, lithium is a popular treatment for bipolar disorder. Recent studies have shown the teratogenicity rates are much lower than reported. The most common effects of fetal exposure are high birth weight and "floppy-baby" syndrome.
* Valproate and carbamazepine. These anticonvulsants are associated with major congenital malformations and carry a greater risk of birth defects than lithium. Valproate and carbamazepine have been linked to neural tube defects, craniofacial anomalies, urogenital problems, growth retardation, microcephaly, and heart defects.
Late last year, the American Epilepsy Society's pregnancy outcomes forum panel recommended that valproate should not be prescribed as firstline therapy for any indication in women of childbearing age because it significantly increases the risk of major malformations in infants who were exposed in utero.
* Lamotrigine. This anticonvulsant is associated with a low overall rate of fetal malformations, but it carries a higher rate of miscarriages and stillbirths than seen in unmedicated women. The agent also has been linked to a skin rash in infants who have different antigen characteristics than their mothers.
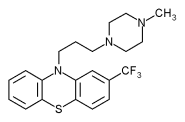
* Chlorpromazine. This first-generation antipsychotic often is used to treat mania during pregnancy. It is among the best-studied of the antipsychotics in pregnancy, and the data support its relative safety in this population. Related compounds, such as trifluoperazine and perphenazine, also may have low teratogenic risk, although they are not as well studied as phenothiazine chlorpromazine.
* Lorazepam and clonazepam. These benzodiazepines often are used to treat the anxiety, agitation, and sleep disturbances that accompany bipolar disorder. They have not been linked to significant increases in malformation rates, although chronic use of benzodiazepines during pregnancy has been linked to withdrawal symptoms in babies.
* Olanzapine. One of the newer atypical antipsychotics, olanzapine, is used for acute mania and for prophylaxis against recurrent mania; however, data on this and the other atypical antipsychotics in pregnancy are still too sparse to make conclusions regarding their reproductive safety, according to Dr. Viguera.
Strategies for minimizing the risks associated with all of these drugs include using monotherapy rather than a combination of drugs, and relying on the lowest possible effective dose, Dr. Viguera said. Folic acid supplementation--in addition to a daily prenatal vitamin--may help reduce the increased risk of neural-tube defects. She recommended that women taking anticonvulsants, in particular, take 4 mg of supplemental folic acid per day during the preconception period through the first trimester.
"All women taking these medications during the first trimester should obtain a high-resolution ultrasound at 16-18 weeks to detect the presence of fetal malformations," Dr. Viguera noted.
In addition, because drug metabolism changes during pregnancy, both maternal and fetal serum drug levels should be monitored regularly.
BY DIANA MAHONEY
New England Bureau
COPYRIGHT 2005 International Medical News Group
COPYRIGHT 2005 Gale Group