Psychopharmacology Notes
In July 2000, the prescription heartburn medication cisapride was withdrawn from the U.S. market by Janssen Pharmaceutica following numerous reports of fatal cardiac arrhythmias. More than 341 cases of arrhythmias and 80 deaths associated with cisapride were reported to the U.S. Food and Drug Administration (FDA, 2001a) between July 1993 and May 1999. A closer look at cisapride shows that its capacity to prolong the QT interval is the likely cause for malignant arrhythmias. The decision to remove cisapride follows the withdrawal of astemizol and terfenadine for similar concerns about QT prolongation. For each of these drugs, the risk for prolonged QTc (QT interval corrected for heart rate) and fatal arrhythmia increased when these effective agents were combined with other commonly used drugs that inhibit hepatic enzymes and drive up the level of the potentially arrhythmia-producing drug.
Although concern about QT prolongation is not new, these high-profile events have prompted greater awareness among psychiatric clinicians. This paper provides an overview of the normal cardiac cycle, describes QT prolongation and its implications, and applies this information to various antipsychotic medications. The final section discusses the impact of drug interaction on the risk of cardiac arrhythmia.
The Normal Cardiac Cycle
At rest, the cardiac muscle cells, or myocytes, are negatively charged (polarized). When the resting myocytes are depolarized, they become positively charged in a progressive wave starting at the sinoatrial (SA) node. Depolarization moves progressively through the heart muscle, causing the myocardium to contract in synchrony with heart valve action. During repolarization, the myocytes regain their negative charge. Each upward (positive) spike on an electrocardiogram (ECG) represents the process of depolarization moving toward a positive electrode on the patient.
The SA node, located in the right atrium, is the cardiac pacemaker. When it initiates regular intervals of depolarization, it is known as sinus rhythm. Each time the SA node emits an electrical impulse, depolarization begins. The wave spreads through both atria, resulting in simultaneous atrial contraction that is reflected by the p wave on an ECG.
The brief pause after the p wave on the ECG reflects the slowing down of the depolarization stimulus within the atrioventricular (AV) node prior to reaching the ventricles. This pause allows the blood in the atria to move past the AV valves and into the ventricles.
Depolarization then spreads through the bundle of His and the bundle branches and through the ventricles, causing them to contract. This ventricular contraction produces the QRS complex on the ECG. During ventricular contraction, the AV valves prevent backflow of the blood to the atria. Venous blood from the right ventricle is pumped to the lungs, and oxygenated blood is simultaneously pumped into the aorta and the rest of the body The ST segment on the ECG reflects the beginning of ventricular repolarization and the T wave is the final rapid stage of repolarization before the cycle begins all over again.
What is a prolonged QT? The QT interval is the time between the beginning of the ventricular complex (QRS) to the end of the T wave (Figure 1). In electrophysiologic terms, this interval is the sum of ventricular depolarization and repolarization. Given that the QT interval is a measure of time, it is highly influenced by heart rate. As the heart rate speeds up, the QT interval shortens. Conversely, the QT interval lengthens as the heart rate slows down. Because the QT interval is influenced by heart rate, it must be corrected for heart rate to be interpreted. This correction is given on standard ECG reports as the QTc.
When the QT is prolonged, it reflects the dispersion of repolarization within the myocardium and may lead to torsades de pointes (Tdp), a type of ventricular arrhythmia that is associated with prolonged QT intervals and can be fatal. Characteristic patterns that distinguish Tdp from other arrhythmias are the prolonged QT intervals, prominent U waves with varying amplitude, and polarity in the basic complexes.
The upper limit of normal for a QT interval has been variously defined ranging from 420 - 500 milliseconds (ms) (Perkins & Lieberman, 1998; Warner, Barnes, & Henry, 1996). Clinically significant QT-interval prolongation is typically defined by pharmaceutical companies as >500 ms (Litherland, 1997). Algra, Tijssen, Roelandt, Pool, and Lubsen (1993) conducted a study of 6,693 consecutive patients undergoing 24-hour ambulatory ECG and followed up with this cohort for as long as 2 years. A mean QTc in excess of 440 ms over 24 hours was associated with more than double the risk of sudden death. In addition, because deceased patients had greater preexisting cardiac morbidity, QTc prolongation may be associated with other cardiac conditions (Algra et al.).
In healthy individuals, several factors can influence the QT interval including food ingestion, time of day, and gender. Nagy and colleagues observed a 16-23 ms increase in the QTc after the ingestion of food in post-- prandial measurements (Nagy et al., 1997). Diurnal variability of the QTc was also found in a study of healthy volunteers in which variability was greatest on awakening (Molnar, Zhang, Weiss, Ehlert, & Rosenthal, 1996). In addition, significantly longer QTc intervals were found in female subjects (Molnar et al.).
A prolonged QT interval may be either congenital (idiopathic) or acquired. Affected individuals with congenital forms of QT prolongation typically have a positive family history of symptoms including syncope, dizzy spells, and sudden death. These symptoms may begin during infancy, and the syncope and dizzy spells can occur without any warning, usually in the morning hours or after strenuous exercise. To date, mutations on four genes (on chromosomes 3,7, and 11) have been associated with congenital QT prolongation. A fifth gene (on chromosome 4) also has been implicated, although the specific mutation has yet to be identified (Wojciech et al., 1998).
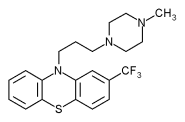
An acquired long-QT syndrome may be precipitated by one or several factors. It may develop as a result of an electrolyte abnormality such as hypokalemia, hypocalcemia, or hypomagnesemia, metabolic or endocrine disturbances, or induced by certain medications. Other risk factors that appear to increase the risk of drug-induced Tdp include age, sex, cardiac history, toxins, and central nervous system (CNS) insult. Of particular interest to psychiatric clinicians are drugs that delay repolarization such as phenothiazines, tricyclic antidepressants, and several common medications used in primary care (Table 1).
A study by Warner et al. (1996) showed a dose-related risk of QTc prolongation with chlorpromazine. In a study of 111 subjects receiving neuroleptics and 42 unmedicated controls between the ages of 21 and 74 years, QTc prolongation was present in 26 (23%) of the medicated sample (>420 ms) compared with 2% of the controls (x^sup 2^ = 7.89, df = 1, p
Table 2 summarizes available information on the association of QT prolongation and selected antipsychotic drugs. Because drug-drug interaction can influence the risk of QT prolongation, the table also cites the vulnerability of each drug to cytochrome P-450 inhibition.
Typical Antipsychotics
Thiodazine. In July 2000, Novartis Pharmaceuticals Corp. notified prescribers and pharmacists about important labeling changes for the phenothiazine, thioridazine (http://www.pharma.novartis.com). Although the warning was new, awareness of the relatively high risk of QTc prolongation with thioridazine was not new. Many years earlier, a controlled study (N = 6) by Ban and St. Jean (1964) demonstrated that thioridazine had a greater effect on cardiac conduction (including QTc prolongation) than chlorpromazine or trifluoperazine. The same investigators evaluated 114 psychotic patients receiving any 1 of 10 different psychotropic drugs at high doses for at least 4 months. Of the 114 patients, 29 developed abnormal ECGs, 77% (n = 17) of whom were taking thioridazine. The conduction changes observed with thioridazine were not only more frequent, but also were of a greater magnitude (Ban & St. Jean, 1965).
During this same period, there were many case reports of sudden death in patients treated with thioridazine in doses ranging from 200-1,600 mg/day (Hartigan-Go, Bateman, Nyberg, Martensson, & Thomas, 1996; Hollister & Kosek, 1965). Accumulated data over the past decade have revealed a clear relationship between dose and risk of QTc prolongation (Carillo et al., 1999; VonBahr et al., 1991). Given the dose relationship, drug interactions also are of concern. A randomized, double-- blind, placebo-controlled study (Hartigan-Go et al.) examined 9 healthy males following single-dose exposure to placebo or one of two doses (10 mg or 50 mg) of thioridazine. In this study, statistically significant lengthening of the QTc was found to be directly related to the dose, and plasma concentration of the drug and its metabolites when compared to placebo (p
Despite this body of evidence, it wasn't until after Pfizer Pharmaceuticals submitted its FDA application for ziprasidone, providing evidence that thioridazine had greater effects than ziprasidone on the cardiac cycle, that the product labeling for thioridazine changed in 2000. There is now a boxed WARNING on the label stating that thioridazine is known to prolong the QT interval and has been associated with Tdp and sudden death.
Droperidol. Droperidol, a butyrophenone, also has been implicated in cases of QTc prolongation. Reilly, Ayis, Ferrier, Jones, and Thomas (2000) conducted a study in 495 psychiatric patients and 101 healthy controls. An abnormal QTc defined as >456 ms was found in 8% (n = 40) of the patient sample. Significant predictors of QTc prolongation were in those on tricyclic antidepressant therapy (Odds Ratio [OR] = 4.4 [1.6-12.1], p = .004), droperidol (OR = 6.7 [1.8-24.8], p = .004), and thioridazine (OR = 5.3 [2.0-13.7], p
Haloperidol. Riker, Fraser, and Cox (1994) conducted a study involving 8 critically ill patients who were treated with continuous infusion of haloperidol (dose range 3-25 mg/hr) for agitation. One patient developed atrial dysrhythmia and intermittent third-degree atrioventricular block on Day 7, and the QTc interval increased from 480 ms to 640 ms when the infusion was increased to a dose of 865 mg/day on Day 6. Once the patient was taken off the medication, the QT interval shortened and the ECG was recorded as normal (Riker et al.).
An earlier case report described a patient with Tdp following oral treatment with haloperidol 20 mg/day for 5 days, and 50 mg/day for an additional 2 days. When the medication was discontinued, the patient's QT interval decreased from 720 ms to 520 ms within 24 hours. Within 72 hours, the QTc decreased to 360 ms, at which time the patient was discharged from the hospital in stable physical condition (Kriwisky, Perry, Tarchitsky, Gutman, & Kishon, 1990).
Atypical Antipsychotics
Sertindole. Sertindole, patented by H. Lundbeck, was considered an effective atypical antipsychotic when it was approved for use in what is now the European Union (EU) in 1996. In 1997 it was recommended for FDA approval in the United States and licensed by Abbott Laboratories, but the application was withdrawn due to concern about reports of sudden unexplained deaths in the EU. Subsequently, sertindole was withdrawn from the EU market and is available for research purposes in the EU but remains unavailable in the United States (http://www. lundbeck.com). Recent results from a study of 30 patients (Agelink et al., 2001) with schizophrenia receiving serial ECGs over a 3-week surveillance period found that upward dose adjustment of sertindole resulted in significant QTc prolongation. Doses started at 4 mg/day and increased incrementally by 4 mg/day every 4 days thereafter (within the recommendations of the manufacturer) until the best clinical response was obtained. Significant, average QTc prolongation (p
Ziprasidone. Ziprasidone, a new atypical antipsychotic, was released to the marketplace in early 2001. The approval was delayed in June 1998, however, after the FDA rejected its application due to concern about its capacity for QTc prolongation. Based on data provided by the company at the time of the first submission, FDA reviewers asked Pfizer to look more closely at the effects of ziprasidone on cardiac conduction. In a series of studies, Pfizer investigators showed that ziprasidone is rarely associated with a substantial increase in QTc (e.g., 20% prolongation), but small increases (e.g., 5% prolongation) are not unexpected. In addition, known inhibitors of CYP3A4 (the presumed pathway of ziprasidone) did not result in a substantial rise in the ziprasidone level (FDA, 2001b).
Risperidone. Buitelaar, van der Gaag, Cohen-Kettenis, and Melman (2001) conducted a 6-week double-- blind study of risperidone in adolescents and found no relevant changes in the cardiac cycle. Although risperidone has been shown to prolong the QTc interval in overdose, there is no average increase in those treated in the usual dose range (FDA, 2001c).
Olanzapine. Czekalla, Beasley, Dellva, Berg, and Grundy (2001) analyzed 12-lead ECGs from four controlled, randomized clinical trials of olanzapine in 2,700 patients with schizophrenia and other psychoses. Using a threshold of 430 ms to define a prolonged QTc, these investigators did not observe any significant changes in the QTc of olanzapine-treated subjects compared to placebo.
Drug Interaction
The experience with cisapride, astemizol, and terfenadine illustrates the importance of the risk of QTc prolongation as a result of drug interaction. Combined treatment of antipsychotics that have a propensity for QT prolongation with a drug that inhibits the cytochrome P450 enzyme that metabolizes the antipsychotic results in an elevated serum concentration of the antipsychotic, increasing the risk of arrhythmias. For example, the combination of pimozide, which has a modest potential for QTc prolongation, can be fatal when combined with clarithromycin (Flockhart et al., 2000). See Table 2 for some commonly prescribed medications that can inhibit cytochrome P-450 activity.
Clinical Implications
Prescribing trends in child psychiatry suggest that the use of psychotropic drugs to treat behavior problems is increasingly common (Zito et al., 2000). Antipsychotics are used for a range of problems in children such as psychosis, agitation, aggression, tics, severe mood instability, and severe impulse control problems (Scahill & Lynch, 1998). There is no dear consensus on how to monitor cardiovascular safety of the antipsychotics when used in pediatric populations. Given this uncertainty, the following recommendations should be viewed as tentative. Clearly, however, some of these drugs are associated with a higher risk of QTc prolongation. This list probably includes thioridazine, pimozide, ziprasidone, and droperidol.
* Thioridazine is no longer a first-line agent in the treatment of children with psychiatric illnesses. Before starting pimozide or ziprasidone, obtain an ECG interpreted by a specialist in pediatric cardiology. Repeat an ECG during the dose-adjustment phase, when a therapeutic dose is achieved, and periodically during maintenance treatment.
* Lawrence and Nasraway (1997) reviewed published reports of conduction disturbances associated with haloperidol or droperidol. Most of the cases involving a prolonged QT interval associated with haloperidol occurred in critically ill patients taking more than 50 mg/24 hours, which is highly unlikely in pediatric patients (Lawrence & Nasraway). Based on these findings, haloperidol is unlikely to prolong the QTc in healthy children at usual doses. Droperidol is typically used in the treatment of acute agitation and is not commonly used in children. Therefore, the risk for prolongation in pediatric populations is unknown.
* Drugs such as risperidone, haloperidol, quetiapine, and chlorpromazine appear to be of lower risk for QTc prolongation at the usual doses. Experience with clozapine in children is minimal and appears to be used only in highly unusual clinical circumstances. With all psychotropic administration, however, it is essential to identify known risk factors that contraindicate therapy. These risk factors can be elicited by a detailed medical history and family medical history. If psychotropic pharmacotherapy is indicated in a patient with one or several risk factors (e.g., electrolyte abnormality, metabolic or endocrine disease, family history of sudden death), this may influence drug selection.
Finally, awareness of the potential for drug interaction is essential for avoiding life-threatening cardiovascular events.
Acknowledgment. The authors acknowledge research support from NIMH Contract N0MH70009 (Dr. Scahill), M01-RR06022 (Yale Children's Clinical Research Center), and the Korczak Foundation (Dr. Scahill).
References
Agelink, M.W., Zeit, T., Baumann, B., Majewski, T., Lemmer, W., Postert, T., Lukas, K., & Klieser, E. (2001). In vivo cardiovascular effects of the new atypical neuroleptic sertindole. International Journal of Psychiatry and Clinical Practice, 5(1), 33-40.
Algra, A., Tijssen, J.G., Roelandt, JR, Pool, J., & Lubsen, J. (1993). QT interval variables from 24 hour electrocardiography and the two year risk of sudden death. British Heart Journal, 70, 43 - 48.
Ban, T.A., & St. Jean, A. (1964). The effect of phenothiazines on the electrocardiogram. Canadian Medical Association Journal, 91, 537-540.
Ban, T.A., & St. Jean, A. (1965). Electrocardiographic changes induced by phenothiazine drugs. American Heart Journal, 70, 575-576.
Buitelaar, J.K., van der Gaag, R.J., Cohen-Kettenis, P., & Melman, C.T. (2001). A randomized controlled trial of risperidone in the treatment of aggression in hospitalized adolescents with subaverage cognitive abilities. Journal of Clinical Psychiatry, 62,239-48.
Carillo, J.A., Ramos, S.I., Herriaz, A.G., Llerena, A., Agundez, J.A.G, Berecz, R., Duran, M., & Benitez, J. (1999). Pharmacokinetic interaction of fluvoxamine and thioridazine in schizophrenic patients. Journal of Clinical Psychopharmacology, 19,494-499.
Czekalla, J., Beasley, C.M., Jr., Dellva, M.A., Berg, P.H., & Grundy, S. (2001). Analysis of the QTc interval during olanzapine treatment of patients with schizophrenia and related psychosis. Journal of Clinical Psychiatry, 62, 191 - 198.
Flockhart, D.A., Drici, M., Kerbusch, T., Soukhova, N., Richard, E., Pearle, EL., Mahal, SK, & Babb, Vj. (2000). Studies on the mechanism of a fatal clarithromycin-pimozide interaction in a patient with tourette syndrome. Journal of Clinical Psychopharmacology, 20,317-324.
Hartigan-Go, K., Bateman, D.N., Nyberg, G., Martensson, E., & Thomas, S.H. (1996). Concentration-related pharmacodynamic effects of thioridazine and its metabolites in humans. Clinical Pharmacology and Therapeutics, 60, 543 - 553.
Hollister, L.E., & Kosek, J.C. (1965). Sudden death during treatment with phenothiazine derivatives. JAMA, 192,1035-1038.
Kriwisky, M., Perry G.Y., Tarchhtsky, D., Gutman, Y, & Kishon, Y (1990). Haloperidol-induced torsades de pointes. Chest, 98, 482 - 484.
Lischke, V., Behne, M., Doelken, P., Schledt, U., Probst, S., & Vettermann, J. (1994). Droperidol causes a dose-dependent prolongation of the QT interval. Anesthesia and Analgesia, 79, 983-986.
Lawrence, K.R., & Nasraway, S.A. (1997). Conduction disturbances associated with administration or butyrophenone antipsychotics in the critically ill: A review of literature. Pharmacotherapy, 17, 531 - 537.
Litherland, S. (1997). Drug treatment and schizophrenia in the 1990's. Drugs, 54, 794.
Molnar, J., Zhang, E, Weiss, j-, Ehlert, KA., & Rosenthal, J.E. (1996). Diurnal pattern of QTc interval: How long is prolonged? Possible relation to circadian triggers of cardiovascular events. Journal of the American College of Cardiology, 27, 76-83.
Nagy, D., DeMeersman, R., Gallagher, D., Pietrobelli, A., Zion, A.S., Daly, D., & Heymsfiled, S.B. (1997). QTc interval (cardiac repolarization): Lengthening after meals. Obesity Research, 6, 531 -537.
Novartis Pharmaceuticals. (2000). Important drug warning [letter]. Retrieved September 4,2001, from httop://www.pharma.novartis.com.
Perkins, D.O., & Lieberman, J.A. (1998). Medical complications and selectivity of therapeutic response to atypical drugs. American Journal of Psychiatry, 155, 252-256.
Reilly, J.G., Ayis, S.A., Ferrier, LN., Jones, S.I., & Thomas, S.H.L. (2000). QTc-interval abnormalities and psychotropic drug therapy in psychiatric patients. The Lancet, 355, 1048-1052.
Riker, R.R., Fraser, G.L., & Cox, PM. (1994). Continuous infusion of haloperidol controls agitation in critically ill patients. Critical Care Medicine, 22,433-440.
Scahill, L., & Lynch, K.A. (1998). Atypical neuroleptics in children and adolescents [Psychopharmacology notes]. Journal of Child and Adolescent Psychiatric Nursing, 11, 38-43.
Sertindole. (1998). Annual report. Retrieved September 4, 2001, from http://www.lundbeck.com.
U.S. Food and Drug Administration. (2001a). Janssen Pharmaceutica stops marketing cisapride in the U.S. [FDA talk paper]. Retrieved September 4, 2001, from http://www.fda.gov.bbs.topics/ANSWERS/ ANS01007.html.
U.S. Food and Drug Administration. (2001b). Psychopharmacological drugs advisory committee. Retrieved September 4, 2001, from http://www.fda.gov/OHRMS/DOCKETS/AC/00/backgrd/ 3619bl.him.
U.S. Food and Drug Administration. (2001c). Retrieved September 4, 2001, from http://www.verity.fda.gov/search97cgi/s97cgi.exe.
VonBahr, C., Movin, G., Nordin, C., Liden, A., Hammarlund-Udenaes, M., Hedberg, A., Ring, H., & Sjoqvist, F. (1991). Plasma levels of thioridazine and metabolites are influenced by the debrisoquin hydroxylation phenotype. Clinical Pharmacology and Therapeutics, 49, 234-240.
Warner, J.P., Barnes, TR., & Henry, J.A. (1996). Electrocardiographic changes in patients receiving neuroleptic medication. Acta Psychiatrica Scandinavica, 93, 311-313.
Wojciech, Z., Moss, Aj., Schwartz, PJ., Vincent, G.M., Robinson, J.L., Priori, S.G., Benhorin, J., Locati, E.H., Towbin, J.A., Keating, M.T., Lehmann, M.H., & Hall, WJ. (1998). Influence of the genotype on the clinical course of the long-QT syndrome. New England Journal of Medicine, 339, 960-965.
Zito, J.M., Safer, D.J., dosReis, S., Gardner, J.F., Boles, M., Lynch, F. (2000). Trends in the prescribing of psychotropic medications to preschoolers. JAMA, 283, 1025-1030.
Search terms: Cardiac conduction, drug interactions, pediatrics, psychotropic drugs, QT interval
Deirdre H. Carroll, MSN, RN, Ramya Shyam, and Lawrence Scahill, PhD, RN
Deirdre H. Carroll, MSN, RN
Psychiatric Nurse Practitioner
Yale Child Study Center
Ramya Shyam
Student, Brandeis University, Waltham, MA
Lawrence Scahill, PhD, RN
Associate Professor
Yale University School of Nursing
Yale Child Study Center, New Haven, CT
Author contact: Deirdre.Carroll@yale.edu, with a copy to the Editor: Poster@uta.edu
Copyright Nursecom, Inc. Oct-Dec 2002
Provided by ProQuest Information and Learning Company. All rights Reserved