Baclofen
Baclofen (brand names Kemstro® and Lioresal®) is a derivative of gamma-aminobutyric acid, and is an agonist specific to mammalian but not fruit fly (Drosophila) GABAB receptors. It is used for the treatment of spastic movement, especially in instances of spinal cord injury and in multiple sclerosis. Its beneficial effects result from actions at spinal and supraspinal sites. Baclofen can also be used to treat hiccups. more...
Description of compound
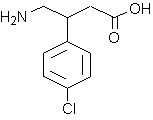
Baclofen is a white to off-white, odorless or practically odorless crystalline powder, with a molecular weight of 213.66. It is slightly soluble in water, very slightly soluble in methanol, and insoluble in chloroform.
Routes of administration
Baclofen can be administered either orally or intrathecally (directly into the spinal fluid). Intrathecal administration is often indicated in spasticity patients, as very little of the oral dose actually reaches the spinal fluid.
Intrathecal administration is particularly used in patients with multiple sclerosis who have severe painful spasms which are not controllable by oral baclofen. A test dose is given to assess the effect, and if successful a chronic intrathecal catheter in inserted and connected to a computer-controlled implanted pump. The reservoir in the pump can be replenished by percutaneous injuection. These pump systems are quite sophisticated and expensive so careful patient selection is required.
History
Historically Baclofen was designed to be a drug for epilepsy in the 1920’s, and was derived from diazepam (Valium©). The effect on epilepsy was disappointing but it was found that in certain patients spasticity decreased. Baclofen was and is still given orally with variable effects. In the severely affected children, the oral dose is so high that side effects appear and the treatment loses its benefit. How and when Baclofen came to be used in the spinal sack is not really clear but this is now an established method for the treatment of spasticity in many conditions.
How Baclofen works
Baclofen has its effect in the spinal cord, which is the main connection between the brain and then rest of the body. The spinal cord is a reflex system, a feedback loop. The most obvious reflex is the withdrawal to heat. This movement is brisk and not very well controlled. This is what happens in Cerebral Palsy. Without adequate control from the brain, every movement is like a reflex, being rough and uncontrolled. The reflex can spread through the body causing spasms or “arching”. These spasms can be painful and interrupt sleep.
Baclofen works on this reflex circuit. The reflex circuit in the spinal cord contains the Renshaw cells. These cells are very sensitive to a natural chemical produced by the nervous system: GABA, gamma-amino-butyric-acid. GABA slows the reflex circuit down and Baclofen acts like GABA. The dose of intrathecal Baclofen necessary to slow down the reflex circuit is variable but is generally one thousand times smaller than the oral dose.
Pharmacokinetics
The drug is rapidly absorbed after oral administration and is widely distributed throughout the body. Biotransformation is low and the drug is predominantly excreted in the unchanged form by the kidneys.
Read more at Wikipedia.org