ABSTRACT
Intrathecal baclofen (ITB) is a relatively new treatment approach that may be useful for treating spasticity in patients with chronic stroke. In this paper, we examine ITB treatment of spastieity caused by stroke and the implications for physical therapy management. We also present ITB pharmacology, side effects, and the screening procedure.
INTRODUCTION
In the United States, stroke is the third most common cause of disability and death after heart disease and cancer.1,2 Every year there are approximately 700,000 new cases of stroke and about one-third of patients die from the incident.1,3,4 Stroke is defined as acute neurological dysfunction of vascular origin that lasts more than 24 hours and has signs and symptoms corresponding to the involvement of focal areas of the brain.5 Almost 75% of patients with stroke have motor impairments, resulting in disability, such as impaired transfer, pain, contractures, gait abnormalities, sleep disorders, and the inability to perform activities of daily living, all of which compromise safety.6-12
Spasticity develops in nearly 65% of patients with stroke and while it is a major cause of disability, in some cases it is beneficial in helping the patient stand or ambulate.13,14 Spasticity is assigned different meanings. However, a frequently cited definition proposed by Lance15 describes spasticity as a motor disorder characterized by a velocity-dependent increase in tonic stretch reflexes (muscle tone) with exaggerated tendon jerks, resulting from hyperexcitability of the stretch reflexes. It is one component of the upper motoneuron syndrome and may interfere with voluntary motor function in patients with residual muscle power.15,16
Current management of spasticity includes passive stretching, strengthening, physical modalities, splinting, biofeedback, cold, and electrical stimulation. These treatments have limited results.17,18 Pharmacological management of spasticity includes peripherally acting drugs such as botulinum toxin and dantrolene sodium or centrally acting drugs such as oral baclofen, diazepam, tizanidine, and clonidine.9-11,19,20 When physical, occupational, and medical management of spasticity fails, the patient with stroke may elect surgical management, such as intrathecal baclofen.21,22
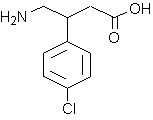
Continuous intrathecal baclofen (ITB) was introduced 2 decades ago to treat spasticity, and its beneficial effect has been well documented.23-26 Baclofen is infused via a subcutaneously placed programmable pump.23,27 The pump is implanted in the abdominal wall (Figure 1) with a catheter threaded into the subarachnoid space, at L1-2 and subsequently threaded as high as T-6. Intrathecal baclofen has been reported in the management of spasticity in stroke,28,29 cerebral palsy,30 spinal cord injury,31,32 and amyotrophic lateral sclerosis.33-35 Francisco describes the perfect ITB candidate as one who has had "a stroke with severe, functionally limiting, multijoint spastic hypertonia and predominant involvement of the lower limbs, and one who cannot either tolerate the effects of oral drugs or respond to adequate doses of other therapies."36
The reminder of this paper will examine ITB treatment of spasticity caused by stroke and the implications for physical therapy management. Spasticity management in spinal cord,37 multiple sclerosis,38 and cerebral palsy3'9 are reviewed elsewhere and are beyond the scope of this review.
BACLOFEN AND ITB PHARMACOLOGY
Baclofen (Lioresal®) is an agonist at the gamma-aminobutyric acid (GABA)-B receptor subtype with little or no action at the GABA-A or GABA-C subtypes.40-44 Baclofen acts predominately at the spinal level and attenuates motor output, especially on high frequency, and reflexively mediated muscle activity (ie, spastic motor activity). It inhibits both monosynaptic and polysynaptic reflexes possibly by decreasing excitatory neurotransmitter release from primary afferent terminals, although actions at supraspinal sites may also occur and contribute to its clinical effect.45
One advantage of intrathecal baclofen is that it allows effective cerebrospinal fluid (CSF) concentrations to be achieved with resultant plasma concentrations of 100 times less than those seen with oral administration.23,46 In addition the programmable pump used to deliver the baclofen allows for numerous dose adjustments that are needed during treatment. However, adverse effects of general CNS depression may still appear as indicated by sedation with tolerance, somnolence, ataxia, and respiratory and cardiovascular depression.
Selecting an ITB Candidate and Screening Protocol
According to Meythaler and colleagues,28,29 the ideal candidate is a patient with stroke who presents with severe chronic spasticity in the lower or upper extremities rated at 3 or 4 on the Ashworth47 scale (5-point scale) and an average of at least 2 on the Penn23 Spasm 4-point scale in the affected extremity, as well as having had intolerable CNS side effects with oral antispasticity agents.28,29 Specifically, the patients who use extensor tone to stand and have trunk control in unsupported bench sitting will demonstrate improvement in function with ITB therapy.48 Whereas those patients who move with hip and knee flexion and ankle dorsiflexion will not show the same success. However the appropriateness of the continuous ITB pump has not been established for patients' with seizures, ventriculoperitoneal shunts, or implantable, programmable medical devices (eg, spinal cord stimulators, pacemakers).
Prior to pump implantation, each patient undergoes an "intrathecal baclofen screening trial."28,29 It begins with an initial Ashworth screening often performed by the physical therapist, followed by a 50 µg intrathecal injection.48 The onset of action of baclofen in adults is generally 1/2 to 1 hour after intrathecal bolus administration. Peak spasmolytic effect is seen approximately 4 hours after dosing and effects may last 4 to 8 hours. Onset, peak response, and duration of action however may vary with individual patients depending on the dose and severity of symptoms.49,50 The Ashworth screening may then be repeated every 2 hours for the next 8 hours. If Ashworth scores do not drop, a higher dose (75 µg) is given on the next day.48 A third day may be necessary with a bolus injection of as much as 100 µg. The recommendation for permanent pump placement (ie, continuous ITB) is based on reduction in the subject's Ashworth scale or Penn Spasm score by 2 without the development of side effects.28,29 Hypotonia, even if greater than desired is a positive result on the screening test.48 However, it must be explained to the patient that the hypotonia is due to receiving the full dose of baclofen all at once via injection as opposed to being slowly titrated with the pump.
After the pump and catheter arc implanted the patient is asked to remain flat for a few days.48 This helps to prevent headaches and cerebral spinal fluid leaks. Other precautions include observing for any swelling over the pump or incision area. The patient may wear an ace wrap around the abdomen or an abdominal binder. These interventions are used to reduce swelling and also help the patient adjust to the change in muscle tone particularly in the upright position for the first few weeks. The patient is usually discharged from the hospital within 1 week only to return for intensive therapy as an outpatient following wound healing. Prior to discharge however, transfers and ambulation are assessed, and assistive devices may be adjusted so that that the patient can function safely.
IMPLICATIONS FOR PRACTICE
After pump implantation, the physical therapist should set goals that account for the patient's lower muscle tone. Transfers and mobility will feel different to the patient and may be more difficult to execute successfully. Splints will need to be reassessed as well as seating systems, and new assistive devices may be considered.
Therapy initially may be complicated by the fact that the pump will need frequent adjustments to titrate the dose of baclofen for proper response. A reduction in muscle tone is desired but weakness and sedation are unwanted. The ITB infusion pump is programmable so it can be set to provide a lower dose of baclofen during the day to allow the patient to use extensor spasticity in the lower extremity to stand and to minimize sedation. A higher dose can be programmed at night to decrease muscle spasms and allow the patient to sleep. Multiple dose adjustments over several months are usually needed to achieve the regimen that is most effective.28,29,50
Research has shown that ITB is effective at producing a significant drop in the Ashworth score and the average spasm score in patients with chronic stroke and those with acquired brain injury.26,28 However, the reduction in muscle tone is generally more profound in the lower extremities than in the upper extremities.51-53 Physical therapy continues to be necessary in the early postoperative period to address the reduction of muscle tone, spasticity, and spasm as well as the lack of improvement in the upper extremities. Treatment interventions include using partial body weight support,54-58 biofeedback,59-62 functional electrical stimulation, neuroprotheses application,63,64 constraint-induced therapy,65-70 and virtual reality.71-73 In addition many patients now find that traditional strengthening is emphasized whereas it was not a focus of their treatment plan prior to pump implantation. Most activities are okay to perform after pump placement with the exception of contact sports or any activity in which there is a risk of trauma to the pump and/or catheter. Forceful trunk rotation is also contraindicated because of the possibility that the catheter may dislodge. The use of heat modalities near the pump or catheter is also prohibited as is the use of hot tubs, saunas, scuba diving, and hyperbaric oxygen.48 These activities might alter the rate at which baclofen is dispensed.
The goals of therapy should be clearly identified and include increasing functional capacity, relieving discomfort, phasing out physical therapy intervention and phasing in everyday activities. Once determined, these goals should be very clear to everyone involved in the patient's care especially the patient. An unrealistic or unspoken expectation by patient, family, and/or carcgiver often leads to disappointment, depression and interpretations of treatment failure.
Effect of ITB on the Less Involved Side
The reflexes on the less involved side are affected by short periods (3 months) of ITB in patients with stroke.29 Furthermore, with continuous ITB (1 year) Meythaler et al reported that the reflex score decreased, but the reduction was not as significant as in the extremities affected by the stroke.28,29 Moreover, muscle strength, using the standard 1-5 motor assessment, did not reveal motor weakness of the less involved side nor did the patient or family notice a drop in the patient's strength.28,29 Francisco36 argued that the less involved limb did not become weak after ITB for 2 reasons. First, ITB probably has a selective effect on certain spinal cord receptors that also receive supraspinal input that is modified by cerebral disease. Second, the amount of infused baclofen is so small that it does not cause significant clinical muscle weakness.36 Currently, there is no conclusive evidence to recommend strengthening the uninvolved upper and/or lower extremities.
Measuring Spasticity versus Functional Improvement after ITB
Reduction of spasticity and spasm are presumed to improve active functional movements.25,28,29,42,74 However, not all research supports that assumption.13,75-77 The general assumption that once spasticity diminishes there will be improvement in voluntary motor function has been challenged. Some authors have noticed that with diminished spasticity there is improvement in function as demonstrated by progressing from wheclchair dependence to independent ambulation with assistive devices.28,29 In addition, patients exhibit easier dressing, diapering, transfer, orthotic wear, and sitting tolerance in almost 90% of cases that receive ITB.74 Similar results were reported for tnrombotic stroke42 and for children with CP.25 Other research suggests that reduction of spasticity may impair motor function if the patient relies on spasticity for support during walking and standing.13,76 Similarly, a recent study reported significant reduction in muscle tone without improvement in motor function when treating finger flexor hypertonia in patients with stroke using botulinum toxin (ie, patient may be able to open the hand to grip but no longer have the strength to hold the object).75
Inappropriate outcome measures have been touted as one reason why functional improvements may not always correspond with successful reduction in tone.78 An outcome measure must be sensitive enough to detect changes in functional improvement. Using the Ashworth scale,47 Muscle Spasm scale,23 and reflex scale to detect changes in function is not be appropriate since they do not measure functional improvement but instead evaluate selected impairments. The impairments measure can convey whether ITB was effective in reducing tone. But, using a measure that captures an overall functional change, that is of interest to the patient and family, may be more appropriate. Some examples of functional performance evaluations include the Functional Independence Measure (FIM),79 Barthel Indices,80-82 Nottingham Health Profile (NHP),83 and the Timed Up and Go test.84 Another appropriate outcome measure is the Canadian Occupational Performance Measure (COPM), a disability measure, which is used to evaluate performance and satisfaction relative to individualized problem areas as defined by the subject or his famly.85,86 Although the COPM has not been used as an outcome measure in patients with stroke, it has been tested and used in other patient populations.87-89
ITB Complications
Continuous ITB has been an effective treatment for patients with stroke who did not respond well to oral medication for spasticity. Both oral medication and ITB have risks, and the physical therapist should be aware of the most common complications that can affect the patient (Table 1).90,91 Abrupt discontinuation of ITB is a cause for concern since this may result in fever, altered mental state, exaggerated return of spasticity, and rigidity.90 Reasons for the abrupt termination may be attributed to a malfunctioning catheter, low drug volume in the pump, battery failure, and of course human programming errors. Early signs of withdrawal include return to baseline spasticity, pruritis, hypotension, and paresthesias. Late signs of withdrawal resemble autonomie dysreflexia or malignant hyperthermia and can be fatal. Emergency treatment includes administration of an GABA agonist. Therapists should encourage the patient to keep their scheduled refill visits and educate them on the symptoms of baclofen withdrawal. Intrathecal baclofen overdose is rare but will cause drowsiness, dizziness, respiratory depression, seizures, loss of consciousness, and coma.90
The therapist also should be aware that there are complications associated with ITB bolus screening test doses. In 1002 test doses, nausea and vomiting (2.6%), sedation (2.2%), urinary retention (1.6%), hypotension (1.2%), seizures (0.2%), and headache (0.1%) were seen.74 The longterm complications seen in 936 subjects after implantation was performed were infection (1.7%), scroma (cerebrospinal fluid collection) (0.8%), hydrocephalus (0.2%), and seizures (0.1%).74 Finally, the most common reason for pump replacement was infection and battery failure (1%).74 A similar study followed up on the effects of ITB in 75 subjects diagnosed with spinal cord injury or multiple sclerosis over a period of 5 to 41 months after pump implant.91 The authors reported 12 patients developed drug-related symptoms, 6 developed wounds, and 3 developed pump problems.90 These studies found that the short- and long-term complications for ITB did not exceed 2.6 for any single complication.
In summary, ITB reduces spasticity; however, it is invasive and considered an expensive mode of treatment that requires close monitoring of the pump and the patient. It is necessary for physical therapists to be familiar and monitor these complications in their patients. Finally, the potential benefits associated with continuous ITB outweigh its risks.
CONCLUSION
Physical therapists encounter situations in which spasticity is responsible for major disability in patients with stroke.6 In addition to careful goal setting, spasticity management following stroke requires a skillful combination of treatment modalities to achieve the best outcome. The consequences of reducing spasticity should be assessed, and treatment of spasticity should be considered when it causes pain or interferes with such functions as ambulation, transfers, and activities of daily living. If spasticity offers stability to a joint and acts as a prop for the limbs, its reduction may only jeopardize the patient's functional capacity.14,75,76 On the other hand, if there is minimal weakness with predominant spasticity, its treatment "will result in tremendous improvement in functional capability for the patient.28 Physical therapy along with antispasticity drugs and surgical management remain the corner-stone in management of patients with spasticity.
REFERENCES
1 American Heart Association. Stroke Statistics. Available at: http://www.americanheart.org/presenter.jhtml? identifier=4725. Accessed September 1, 2000.
2 American Heart Association. 1998 Heart and Stroke Statistical Update. Dallas, Tex: American Heart Association; 1998.
3 Broderick J, Brott T, Kothari R, et al. The Greater Cincinnati/Northern Kentucky Stroke Study: Preliminary first-ever and total incidence rates of stroke among blacks. Stroke. 1998;29:415-421.
4 Rosamond WD, Folsom AR, Chambless LE, et al. Stroke incidence and survival among middle-aged adults: 9-year follow-up of the Atherosclerosis Risk in Communities (ARIC) cohort. Stroke. 1999;30:736-743.
5 Post-Stroke Rehabilitation Guideline Panel, United States, Agency for Health Care Policy and Research. Post-stroke rehabilitation. Rockville, Md: U.S. Dcpt. of Health and Human Services, Public Health Service, Agency for Health Care Policy and Research; 1995.
6 Wojner AW Optimizing ischemic stroke outcomes: an interdisciplinary approach to poststroke rehabilitation in acute care. Crit Care Nurs Q. 1996;19:47-61.
7 Nyberg L, Gustafson Y. Patient falls in stroke rehabilitation. A challenge to rehabilitation strategies. Stroke. 1995;26:838-842.
8 Forster A, Young J. Incidence and consequences of falls due to stroke: A systematic inquiry [see comments]. BMJ. 1995;311:83-86.
9 Young RR, Delwaide PJ. Drug therapy: Spasticity (second of two parts). N Engl J Med. 1981;304:96-99.
10 Young RR, Delwaide PJ. Drug therapy: Spasticity (first of two parts). N Engl J Med. 1981;304:28-33.
11 Katz RT. Management of Spasticity. Am J Phys Med Rehabil. 1988;67:108-116.
12 Gresham GE, Phillips TF, Wolf PA, McNamara PM, Kannel WB, Dawber TR. Epidemiologic profile of long-term stroke disability: The Framingham study. Arch Phys Med Rehabil. 1979;60:487-491.
13 McGuire JR, Harvey RL. The prevention and management of complications after stroke. Phys Med Rehabil Clin N Am. 1999;10:857-74, ix.
14 Landau WM. Editorial: Spasticity: The fable of a neurological demon and the emperor's new therapy. Arch Neurol. 1974;31:217-219.
15 Lance JW Symposium Synoposis. In: Feldman RG, Young RR, Koella WP, eds. Spasticity, Disordered Motor Control. Chicago, Ill: Year Book Medical Publishers; CIBA-GEIGY Corporation; 1980:485-494.
16 Mizrahi EM, Angel RW Impairment of voluntary movement by Spasticity. Ann Neurol. 1979;5:594-595.
17 O'Sullivan SB. Stroke. In: O'Sullivan SB, Schmitz TJ, eds. Physical Rehabilitation Assessment and Treatment. Philadelphia, Pa: F.A. Davis; 2001:519-581.
18 Ward AB.A summary of Spasticity management-a treatment algorithm. Eur J Neurol. 2002;9 Suppl 1:48-52.
19 Esquenazi A, Mayer N. Botulinum toxin for the management of muscle overactivity and spasticity after stroke. Curr Atberoscler Rep. 2001;3:295-298.
20 Barnes MP. Medical management of spasticity in stroke. Age Ageing. 2001;30 Suppl 1:13-16.
21 Lazorthes Y, Sol JC, Sallerin B, Verdie JC. The surgical management of Spasticity. Eur J Neurol. 2002; 9 Suppl 1:35-41.
22 Peacock WJ, Arens LJ, Berman B. Cerebral palsy spasticity. Selective posterior rhizotomy. Pediatr Neurosci. 1987;13:61-66.
23 Penn RD, Savoy SM, Corcos D, et al. Intrathecal baclofen for severe spinal spasticity. N Engl J Med. 1989;320: 1517-1521.
24 Nance P, Schryvers O, Schmidt B, Dubo H, Loveridge B, Fewer D. Intrathecal baclofen therapy for adults with spinal spasticity: Therapeutic efficacy and effect on hospital admissions. Can J Neurol Sci. 1995;22:22-29.
25 Albright AL, Barron WB, Fasick MP, Polinko P, Janosky J. Continuous intrathecal baclofen infusion for spasticity of cerebral origin. JAMA. 1993;270:2475-2477.
26 Meythaler JM, Devivo MJ, Hadley M. Prospective study on the use of bolus intrathecal baclofen for spastic hypertonia due to acquired brain injury. Arch Phys Med Rehabil. 1996;77:461-466.
27 Almeida GL, Campbell SK, Girolami GL, Penn RD, Corcos DM. Multidimensional assessment of motor function in a child with cerebral palsy following intrathecal administration of baclofen. Phys Ther. 1997; 77:751-764.
28 Meythaler JM, Guin-Renfroe S, Brunner RC, Hadley MN. Intrathecal baclofen for spastic hypertonia from stroke. Stroke. 2001;32:2099-2109.
29 Meythaler JM, Guin-Renfroe S, Hadley MN. Continuously infused intrathecal baclofen for spastic/dystonic hemiplegia: a preliminary report. Am J Phys Med Rebabil. 1999;78:247-254.
30 Meythaler JM, Guin-Renfroe S, Law C, Grabb P, Hadley MN. Continuously infused intrathecal baclofen over 12 months for spastic hypertonia in adolescents and adults with cerebral palsy. Arch Phys Med Rebabil. 2001; 82:155-161.
31 Meythaler JM, Steers WD, Tuel SM, Cross LL, Haworth CS. Continuous intrathecal baclofen in spinal cord spasticity. A prospective study. Am J Phys Med Rehabil. 1992;71:321-327.
32 Meythaler JM, Steers WD, Tuel SM, Cross LL, Sesco DC, Haworth CS. Intrathecal baclofen in hereditary spastic paraparesis. Arch Phys Med Rehabil. 1992;73:794-797.
33 Marquardt G, Lorenz R. Intrathecal baclofen for intractable spasticity in amyotrophic lateral sclerosis. J Neurol. 1999;246:619-620.
34 Marquardt G, Seifert Y Use of intrathecal baclofen for treatment of spasticity in amyotrophic lateral sclerosis. J Neurol Neurosurg Psychiatry. 2002;72:275-276.
35 Orsnes G, Crone C, Krarup C, Petersen N, Nielsen J. The effect of baclofen on the transmission in spinal pathways in spastic multiple sclerosis patients. Clin Neurophysiol. 2000;111:1372-1379.
36 Francisco GE. Can Intrathecal baclofen therapy unleash functional recovery after stroke? Stroke. 2001;32:2108-2109.
37 Taricco M, Adone R, Pagliacci C, Telaro E. Pharmacological interventions for spasticity following spinal cord injury. Cochmne Database Syst Rev. 2000;CD001131.
38 Shakespeare DT, Boggild M, Young C. Anti-spasticity agents for multiple sclerosis. Cocbrane Database Syst Rev. 2001;CD001332.
39 Butler C, Campbell S. Evidence of the effects of intrathecal baclofen for spastic and dystonic cerebral palsy. AACPDM Treatment Outcomes Committee Review Panel. Dev Med Child Neurol. 2000;42:634-645.
40 Ochs G, Struppler A, Meyerson BA, et al. Intrathecal baclofen for long-term treatment of spasticity: A multicentre study. J Neurol Neurosurg Psychiatry. 1989; 52:933-939.
41 Zhang SJ, Jackson MB. GABA-activated chloride channels in secretory nerve endings. Science. 1993;259:531-534.
42 Gwartz BL. Intrathecal baclofen for spasticity caused by thrombotic stroke. Am J Phys Med Rehabil. 2001; 80:383-387.
43 Grades JM, Nance P, Elovic E, McGuire J, Simpson DM. Traditional pharmacological treatments for spasticity. Part II: General and regional treatments. Muscle Nerve Suppl. 1997;6:S92-120.
44 O'Brien CF, Seeberger LC, Smith DB. Spasticity after stroke. Epidemiology and optimal treatment. Drugs Aging. 1996;9:332-340.
45 Bowery NG, Bettler B, Froestl W, et al. International Union of Pharmacology. XXXIII. Mammalian gammaaminobutyric acid(B) receptors: Structure and function. Pbarmacol Rev. 2002;54:247-264.
46 Campbell SK, Almeida GL, Penn RD, Corcos DM. The effects of intrathecally administered baclofen on function in patients with spasticity. Phys Ther. 1995;75:352-362.
47 Ashworth B. Preliminary trial of carisoprodol in multiple scloerosis. Practitioner. 1964;192:540-542.
48 Barry MJ, VanSwearingen JM, Albright AL. Intrathecal Baclofen therapy and the role of the physical therapist. Ped Phys Ther. 2000;12:77-86.
49 Katzung BG. Basic & Clinical Pharmacology. New York, NY: Lange Medical Books/McGraw-Hill; 2001;458-459[09].
50 Goodman LS, Hardman JG, Limbird LE, Gilman AG. Goodman & Gilman's The Pharmacological Basis of Therapeutics. New York, NY: McGraw-Hill; 2001: 1930[09].
51 Meythaler JM, McCary A, Hadley MN. Prospective assessment of continuous intrathecal infusion of baclofen for spasticity caused by acquired brain injury: A preliminary report. J Neurosurg, 1997;87:415-419.
52 Meythaler JM, Guin-Renfroe S, Grabb P, Hadley MN. Long-term continuously infused intrathecal baclofen for spastic-dystonic hypertonia in traumatic brain injury: 1-year experience. Arch Phys Med Rehabil. 1999;80:13-19.
53 Grabb PA, Guin-Renfroe S, Meythaler JM. Midthoracic catheter tip placement for intrathecal baclofen administration in children with quadriparetic spasticity. Neurosurgery. 1999;45:833-836.
54 Visintin M, Barbeau H, Korner-Bitensky N, Mayo NE. A new approach to retrain gait in stroke patients through body weight support and treadmill stimulation. Stroke. 1998;29:1122-1128.
55 Sullivan KJ, Duncan PW New perspectives for locomoter training after stroke: Emerging evidence from basic science and clinical research. Neurology Report. 2000;24:55-59.
56 Hesse S, Bertelt C, Jahnke MT, et al. Treadmill training with partial body weight support compared with physiotherapy in nonambulatory hemiparetic patients. Stroke. 1995;26:976-981.
57 Hesse S, Malezic M, Schaffrin A, Mauritz KH. Restoration of gait by combined treadmill training and multichannel electrical stimulation in non-ambulatory hemiparetic patients. Scand J Rehabil Med. 1995;27:199-204.
58 Hesse S, Konrad M, Uhlenbrock D. Treadmill walking with partial body weight support versus floor walking in hemiparetic subjects. Arch Phys Med Rehabil. 1999;80:421-427.
59 Moreland JD, Thomson MA, Fuoco AR. Electromyographic biofeedback to improve lower extremity function after stroke: A meta-analysis. Arch Phys Med Rehabil. 1998;79:134-140.
60 Intiso D, Santilli V, Grasso MG, Rossi R, Caruso I. Rehabilitation of walking with electromyographic biofeedback in foot-drop after stroke. Stroke. 1994; 25:1189-1192.
61 Moreland J, Thomson MA. Efficacy of electromyographic biofeedback compared with conventional physical therapy for upper-extremity function in patients following stroke: a research overview and meta-analysis. Phys Ther. 1994;74:534-543.
62 Crow JL, Lincoln NB, Nouri FM, De Weerdt W. The effectiveness of EMG biofeedback in the treatment of arm function after stroke. International Disability Studies. 1989;11:155-160.
63 Chae J, Yu D. A critical review of neuromuscular electrical stimulation for treatment of motor dysfunction in hemiplegia. Assist Technol. 2000;12:33-49.
64 Daly JJ, Ruff RL, Haycook K, Strasshofer B, Marsolais EB, Dobos L. Feasibility of gait training for acute stroke patients using FNS with implanted electrodes. J Neurol Sci. 2000;179:103-107.
65 Deibert EM, Dromerick AW. Motor restoration and spasticity management after stroke. Curr Treat Options Neurol. 2002;4:427-433.
66 van der Lee JH, Wagenaar RC, Lankhorst GJ, Vogelaar TW, Deville WL, Bouter LM. Forced use of the upper extremity in chronic stroke patients: results from a single-blind randomized clinical trial. Stroke. 1999;30:2369-2375.
67 Miltner WH, Bander H, Sommer M, Dettmers C, Taub E. Effects of constraint-induced movement therapy on patients with chronic motor deficits after stroke: A replication. Stroke. 1999;30:586-592.
68 Taub E, Miller NE, Novack TA, et al. Technique to improve chronic motor deficit after stroke. Arch Phys Med Rehabil. 1993;74:347-354.
69 Taub E, Wolf SL. Constaint induced movement techniques to facilitate upper extremity use in stroke patients. Top Stroke Rehabil. 1997;3:38-61.
70 Blanton S, Wolf SL. An application of upper-extremity constraint-induced movement therapy in a patient with subacute stroke. Phys Ther 1999;79:847-853.
71 Merians AS, Jack D, Boian R, et al. Virtual reality-augmented rehabilitation for patients following stroke. Phys Ther. 2002;82:898-915.
72 Gourlay D, Lun KC, Lee YN, Tay J. Virtual reality for relearning daily living skills. Int J Med Inf. 2000;60:255-261.
73 Jack D, Boian R, Merians AS, et al. Virtual reality-enhanced stroke rehabilitation. IEEE Trans Neural Syst Rehabil Eng. 2001;9:308-318.
74 Stempien L, Tsai T. Intrathecal baclofen pump use for spasticity: a clinical survey. Am J Phys Med Rehabil 2000;79:536-541.
75 Bakheit AM, Thilmann AF, Ward AB, et al. A randomized, double-blind, placebo-controlled, dose-ranging study to compare the efficacy and safety of three doses of botulinum toxin type A (Dysport) with placebo in upper limb spasticity after stroke. Stroke. 2000;31:2402-2406.
76 Sahrmann SA, Norton BJ. The relationship of voluntary movement to spasticity in the upper motor neuron syndrome. Ann Neurol. 1977;2:460-465.
77 Middel B, Kuipers-Upmeijer H, Bouma J, et al. Effect of intrathecal baclofen delivered by an implanted programmable pump on health related quality of life in patients with severe spasticity. J Neurol Neurosurg Psychiatry. 1997;63:204-209.
78 Pierson SH. Outcome measures in spasticity management. Muscle Nerve Suppl. 1997;6:S36-S60.
79 Dodds TA, Martin DP, Stolov WC, Deyo RA. A validation of the functional independence measurement and its performance among rehabilitation inpatients. Arch Phys Med Rehabil. 1993;74:531-536.
80 Dewing J. A critique of the Barthel Index. Br J Nurs. 1992;1:325-329.
81 Wade DT, Collin C. The Barthel ADL Index: A standard measure of physical disability? Int Disabil Stud. 1988; 10:64-67.
82 Mahoney FT, Barthel D. Functional evaluation: Barthel Index. Md State Med J. 1965;14:61-65.
83 Kind P, Carr-Hill R. The Nottingham health profile: A useful tool for epidemiologists? Soc Sci Med. 1987;25: 905-910.
84 Podsiadlo D, Richardson S. The timed "Up & Go": A test of basic functional mobility for frail elderly persons. J Am Geriatr Soc. 1991;39:142-148.
85 Law M, Baptiste S, McColl M, Opzoomer A, Polatajko H, Pollock N. The Canadian occupational performance measure: an outcome measure for occupational therapy. Can J Occup Ther. 1990;57:82-87.
86 Law M, Polatajko H, Pollock N, McColl MA, Carswell A, Baptiste S. Pilot testing of the Canadian Occupational Performance Measure: Clinical and measurement issues. Can J Occup Ther. 1994;61:191-197.
87 Barry M, Labright A. Use of Canadian Occupational Performance Measure as an outcome measure for Intrathecal Baclofen therapy. Pediatr Phys Ther. 1996;8:183-184.
88 Fragala MA, O'Neil ME, Russo KJ, Dumas HM. Impairment, Disability, and Satisfaction outcomes after lower-extremity Botulinum Toxin an injections for children with Cerebral Palsy. Pediatr Phys Ther. 2002;14: 132-144.
89 Carpenter L, Baker GA, Tyldesley B. The use of the Canadian occupational performance measure as an outcome of a pain management program. Can J Occup Ther. 2001;68:16-22.
90 Medtronic Inc. Lioresal Intrathecal. Available at: http://www.medtronic.com. Accessed June 30, 2003
91 Physicians Desk Reference. 51st ed. Montvale, NJ: Medical Economics Company; 1997.
92 Coffe Y JR, Cahill D, Steers W, et al. Intrathecal baclofen for intractable spasticity of spinal origin: Results of a long-term multicenter study. J Neurosurg. 1993;78:226-232.
Mohamed Ibrahim, PT, MS, NCS1
John Wurpel, PhD,2
Barbara Gladson, PhD, PT, OTR3
1 Assistant Professor, Physical Therapy Program, SUNY-Downstate Medical Center, Brooklyn, NY (Mohamed.ibrahim@downstate.edu)
2 Associate Professor, St. John's University, Dept of Pharmaceutical Science, Jamaica, NY
3 Associate Professor, Doctoral Program in Physical Therapy, University of Medicine and Dentistry of New Jersey, Newark, NJ
Copyright Neurology Report Dec 2003
Provided by ProQuest Information and Learning Company. All rights Reserved