Abstract
A 54-year-old male presented with a sudden generalized eruption of itchy violaceous papules, annular plaques, superficial vesicles, and erosions involving his trunk, limbs, oral cavity, and genitalia. The biopsy showed features of lichen planus (LP). Direct and indirect immunofluorescence (IF) was negative. Systemic treatment with oral corticosteroids in the form of 10 tablets of betamethasone 0.5 mg in a single dose was given after breakfast on 2 consecutive days every week. Complete arrest of progression, control of itching, and flattening of lesions was achieved within 3 weeks allowing tapering of the dose of corticosteroid by 0.5 mg every 2 weeks over next 10 weeks. No side effects of corticosteroid therapy were noted and the patient is in remission.
**********
Case Report
A 54-year-old male presented with a 2-month history of sudden eruption of generalized, intensely itchy violaceous papules, plaques, superficial vesicles, and erosions involving his trunk, limbs, and genitalia. His past history was not contributory. There was no history of any drug intake at the time of appearance of the lesions. He had been treated with topical steroids, emollients, and antihistamines by a general practitioner before being referred to us. Cutaneous examination revealed multiple, discrete as well as coalescing, 2 mm to 10 mm, flat, violaceous papules and numerous 1 cm to 4 cm annular plaques with a raised, purple, thready border on his entire trunk and limbs (Figure 1).
Whitish streaks were seen on top of these papules. Superficial vesicles and erosions were noted on several of these lesions (Figure 1). Irregular violaceous plaques with white streaks were present on both buccal mucosae. Annular lesions with erosions were noted on the glans penis. The palms, soles, nails, and scalp were not affected. Clinical diagnosis of acute generalized vesicular and erosive LP was made. Biopsies taken from a flat papule on the right leg and a vesicular lesion on the abdomen showed hyperkeratosis, acanthosis, wedge-shaped hypergranulosis in the epidermis; dense band-like inflammatory infiltrate of lymphocytes and histiocytes in the upper dermis hugging the basal layer of the epidermis causing basal cell vacuolar degeneration at many places. Pigment incontinence and melanophages were seen in the dermis. Biopsy from the vesicular lesion showed a separation at the epidermo-dermal junction with microvesiculation over the band-like infiltrate. Direct as well as indirect IF was negative. The findings were consistent with the diagnosis of LP. The patient's complete blood cell count, fasting, and post-prandial blood sugar levels, liver, and renal functional tests, urinalysis, and chest x-ray were normal. Serology for Hepatitis B surface antigen (HbsAg) and Hepatitis C virus (HCV) were negative.
[FIGURE 1 OMITTED]
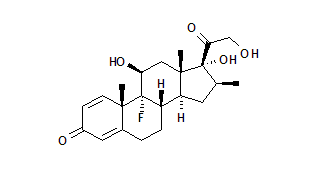
The patient was given oral corticosteroids in a weekly pulse form (10 tablets of betamethasone 0.5 mg in a single dose after breakfast on 2 consecutive days every week). Triamcinolone in Orabase was applied 3 times daily on the oral lesions. Mometasone furoate 1% cream mixed with white petrolatum was applied twice daily on the trunk and limb lesions. Itching subsided completely with the first pulse itself. All papules and plaques became flat, the vesicles subsided, and the erosions dried up within 3 weeks. No fresh lesions appeared. After the 8th week, the dose of oral steroids was reduced by 0.5 mg betamethasone every 2 weeks over next 10 weeks. All the lesions healed leaving behind dark brown hyperpigmentation (Figure 2). There has been no recurrence in 6 months after follow-up.
Discussion
LP is an immune-mediated, common skin disease characterized by skin lesions (pruritic, polygonal, purple papules with white striae on the surface), oral and genital mucosal, and nail involvement, occurring either alone or in various combinations. Hair follicles may be affected. Several variants such as bullous, actinic, atrophic, linear, hypertrophic, follicular (lichen planopilaris), annular, and guttate are described. (1) The disease is characterized by recurrent crops and usually resolves within 2 years leaving behind hyperpigmentation. However, sometimes the disease runs a very prolonged course. Acute vesicular form is rare and needs to be differentiated from lichen planus pemphigoides (LPP), a variant in which bullae appear over lesional as well as normal looking skin in a patient having classical LP. (1) In Bullous LP, the vesicles appear over existing LP lesions, presumably due to severe interface dermatitis. (1) Direct immunofluorescence (DIF) and indirect IF is positive in LPP, but negative in LP. A number of treatments have been used to treat LP, however, systemic and topical corticosteroids remain the mainstay of therapy of LP. (1) Daily or alternate day systemic corticosteroids are able to control the signs and symptoms of LP, but have significant side effects.
High-dose corticosteroids in a parenteral pulse form were first used in renal transplant patients to prevent graft rejection. (2) Since then, pulsed high-dose corticosteroids have been used successfully for many systemic and cutaneous disorders. (3-13) A novel approach to minimize the side effects of corticosteroids has been suggested to give corticosteroids in a weekly pulse form (giving 5 mg betamethasone in a single morning dose after breakfast on 2 consecutive days every week) till the arrest (stoppage of progression) of the disease as well as amelioration of the signs and symptoms. (14) The weekly dose of the oral corticosteroids is reduced by 0.5 mg every 2 to 4 weeks depending upon the severity of the condition. This form of weekly pulse therapy with CS has been called oral mini-pulse therapy (OMP) (14) to differentiate it from the parenteral corticosteroid pulse therapy successfully used for many autoimmune systemic as well as cutaneous diseases for more than 30 years now. (3-13) OMP has been successfully used in many steroid responsive dermatoses such as vitiligo, (14-15) alopecia areata, (16-18) myositis, (19) and even infantile hemangioma. (20) Most of these studies report a rapid arrest of progression of the condition and a low incidence of corticosteroid-related minor side effects in these patients. No acute or clinical side effects were noted in our patient. Hematological and clinical chemistry followed at monthly intervals did not reveal any abnormality in this patient. There was no weight gain or any other clinical side effect noted in this patient. OMP with corticosteroids has many advantages over daily or alternate day steroids such as less frequent dosing thus ensuring compliance and decreased risk of short- and long-term side effects associated with corticosteroid therapy. Controlled studies with corticosteroid OMP in a larger number of patients having LP and other steroid responsive dermatoses are required.
[FIGURE 2 OMITTED]
References
1. Black MM. Lichen planus and lichenoid disorders. In: Champion RH, Burton JL, Burns DA, et al, eds. Textbook of Dermatology. 6th ed. Oxford, England: Blackwell Science, 1998:1899-1926.
2. Kountz SL, Cohn R. Initial treatment of renal allografts with large intrarenal doses of immunosuppressive drugs. Lancet. 1969;1:338-340.
3. Cathcart ES, Schienberg MA, Idelson BA, Couser WG. Beneficial effects of methylprednisolone "pulse" therapy in diffuse proliferative lupus nephritis. Lancet. 1976;1:163-166.
4. Nield GH, Lee HA. Methylprednisolone "pulse" therapy in the treatment of polyarteritis nodosa. Postgrad Med J. 1977;53:382-387.
5. Liebling MR, Leib E, McLaughlin K, Blocka K, Furst DE, Nyman K, et al. Pulse methylprednisolone therapy in rheumatoid therapy. Ann Int Med. 1981;94:21-26
6. Johnson RB, Lazarus GS. Pulse therapy. Arch Dermatol. 1982;118:76-84.
7. Snyder RA, Schwartz RA, Schneider JS, Elias PM. Intermittent megadose corticosteroid therapy for generalized lichen planus. J Am Acad Dermatol. 1982;6:1089-1090.
8. Pasricha JS, Thanzama J, Khan UK. Intermittent high dose dexamethasone-cyclophosphamide pulse therapy for pemphigus. Br J Dermatol. 1988;119:73-77.
9. Sharada B, Kumar A, Kakker R, Adya CM, Pande I, Uppal SS, et al. Intravenous dexamethasone pulse therapy in diffuse systemic sclerosis. A randomized placebo-controlled study. Rheumatol Int. 1994;14:91-4.
10. Goldberg JW, Lidsky MD. Pulse methylprednisolone therapy for persistent subacute cutaneous lupus erythematosus. Arthritis Rheumatism. 1984;27:837-838.
11. Sigel J, Engelstein WH. High dose methylprednisolone in the treatment of bullous pemphigoid. Arch Dermatol. 1984;1157-1165.
12. Pai BS, Srinivas CR, Sabitha L, Shenoi SD, Balachandran CN, Acharya S. Efficacy of dexamethasone pulse therapy in progressive systemic sclerosis. Int J Dermatol. 1995;34:726-8.
13. Roujeau JC. Pulse glucocorticoid therapy. Arch Dermatol. 1996;132:1499-1502.
14. Pasricha JS, Khaitan BK. Oral mini-pulse therapy with betamethasone in vitiligo patients having extensive or fast-spreading disease. Int J Dermatol. 1993;32:753-7.
15. Radakovic-Fijan S, Furnsinn-Friedl AM, Honigsmann H, Tanew A. Oral dexamethasone pulse treatment for vitiligo. J Am Acad Dermatol. 2001;44:814-7.
16. Sharma VK. Pulsed administration of corticosteroids in the treatment of alopecia areata. Int J Dermatol. 1996;35:133-6.
17. Sharma VK, Muralidhar S. Treatment of widespread alopecia areata in young patients with monthly oral corticosteroid pulse. Pediatr Dermatol. 1998;15:313-7.
18. Sharma VK, Gupta S. Twice weekly 5 mg dexamethasone oral pulse in the treatment of extensive alopecia areata. J Dermatol. 1999;26:562-5.
19. van der Meulen MF, Hoogendijk JE, Wokke JH, de Visser M. Oral pulsed high-dose dexamethasone for myositis. J Neurol. 2000;247:102-5.
20. Verma K, Verma KK. Infantile periocular haemangioma treated with two days in a week betamethasone oral mini pulse therapy. Indian J Pediatr. 2001;68:355-6.
Nawaf Al-Mutairi MD FRCP, Arun Joshi MD, Amr Zaki MD, Ashok Kumar Sharma MD DNB, Osama Nour-Eldin MSc
Department of Dermatology, Farwaniya Hospital, Kuwait
Address for Correspondence
Nawaf Al-Mutairi, MD, FRCP
P.O.Box: 280
Farwaniya
State of Kuwait.
Phone: 965 4894238
Fax: 965 4808167
e-mail: nalmut@usa.net
COPYRIGHT 2005 Journal of Drugs in Dermatology, Inc.
COPYRIGHT 2005 Gale Group