Background: [Beta]-blockade controls the ventricular response to exercise in chronic atrial fibrillation (AF), but the effects of [Beta]-blockers on exercise capacity in AF have been debated.
Methods: Twelve men with AF (65 [+ or -] 8 years) participated in a randomized, double-blind, placebo-controlled study of betaxolol (20 mg daily). Patients underwent maximal exercise testing with ventilatory gas exchange analysis, and a separate, submaximal test (50% of maximum) during which cardiac output was measured by a [CO.sub.2] rebreathing technique.
Results: After betaxolol therapy, heart rate was reduced both at rest (92 [+ or -] 27 vs 62 [+ or -] 12 beats/min; p [is less than] 0.001) and at peak exercise (173 [+ or -] 22 vs 116 [+ or -] 24 beats/min; p [is less than] 0.001). Maximal oxygen uptake ([VO.sub.2]) was reduced by 19% after betaxolol (21.8 [+ or -] or 5.3 with placebo vs 17.6 [+ or -] 5.1 mL/kg/min with betaxolol; p [is less than] 0.05), with similar reductions observed for maximal exercise time, minute ventilation, and [CO.sub.2] production. [VO.sub.2] was reduced by a similar extent (19%) at the ventilatory threshold. Submaximal cardiac output was reduced by 15% during betaxolol therapy (12.9 [+ or -] 2.3 vs 10.9 [+ or -] 1.3 L/min; p [is less than] 0.05), and stroke volume was higher (88.0 [+ or -] 21 vs 105.6 [+ or -] 19 mL/beat; p [is less than] 0.05).
Conclusion: Betaxolol therapy in patients with AF effectively controlled the ventricular rate at rest and during exercise, but also caused considerable reductions in maximal [VO.sub.2] and cardiac output during exercise. The observed increase in stroke volume could not adequately compensate for reduced heart rate to maintain [VO.sub.2] during exercise.
(CHEST 1999; 115:1175-1180)
Key words: atrial fibrillation; beta blockade; exercise capacity; oxygen uptake
Abbreviations: AF = atrial fibrillation; VE = minute ventilation; [VCO.sub.2] = carbon dioxide output; [VO.sub.2] = oxygen uptake
Chronic atrial fibrillation (AF) is usually characterized by a rapid, irregular ventricular response at rest and during exercise, and can be associated with reduced exercise capacity, fatigue, and a higher risk for thromboembolie events.[1,2] Conventional pharmacologic therapy for chronic AF attempts to balance control of the rapid, irregular ventricular rate with the negative inotropic effects of most interventions. For example, [Beta]-blockade has been shown to be effective in reducing the ventricular rate at rest and during exercise; reductions in maximal heart rate have been demonstrated in the order of 25 to 40 beats/min.[3-9] Control of the ventricular response is generally thought to make the heart more efficient by increasing ventricular filling time, and therefore end-diastolic volume, leading to an increase in stroke volume. On the other hand, adequate ventricular control by [Beta]-blockade has resulted in reductions in exercise capacity; peak oxygen uptake ([VO.sub.2]) or exercise time has been reduced by 15 to 20% in some studies,[4,7] although [Beta]-blockade has had minimal effects on exercise capacity in others.[6,9]
Because heart rate is a major determinant of cardiac output, the attenuation of exercise capacity by [Beta]-blockade is presumably caused by reductions in cardiac output, but the extent to which cardiac output is reduced during exercise after [Beta]-blockade therapy in these patients has not been documented. The conflicting data on the effects of [Beta]-blockade on exercise capacity in AF may be due to differences in the extent to which cardiac output was reduced. In this study we performed a randomized, crossover evaluation of the effects of betaxolol (a recently approved [Beta]-receptor antagonist) on exercise capacity in patients with chronic AF. To evaluate the influence of [Beta]-blockade therapy on stroke volume and cardiac output, a subgroup of patients underwent submaximal exercise testing while these variables were measured using [CO.sub.2] rebreathing techniques.
MATERIALS AND METHODS
Twelve men (mean age, 66 [+ or -] 8 years) with chronic AF of at least 1 year's duration participated in the study. Clinical characteristics of the subjects are listed in Table 1. Acutely ill patients were excluded, as were those with congestive heart failure, angina, inability to walk on a treadmill, symptomatic lung disease, or thyroid dysfunction. Patients remained on their normal therapeutic doses of digoxin. All rights and privileges were honored in accordance with a protocol approved by the Human Subjects Investigational Review Board at Stanford University, and written informed consent was obtained.
(*) Dig = digoxin; War = warfarin; Dilt = diltiazem; Lis = lisinopril; Nif = nifedipine; Max = maxzide; ASA = aspirin; Enal = enalapril; DM = diabetes mellitus; TIA = transient ischemic attack; HTN = hypertension; ETOH = history of alcohol abuse; CAD = coronary artery disease; CVA = cerebrovascular accident; LONE = lone atrial fibrillation.
Study Protocol
Each patient underwent a randomized, double-blind, placebo-controlled crossover protocol, with a minimum washout period of 1 week between treatments. Patients received either 20 mg of betaxolol once daily or placebo. Betaxolol is a cardio-selective [Beta]-receptor antagonist with no partial sympathomimetic activity, and a relatively long half life (16 to 22 h). Twenty mg of betaxolol represents a medium-range dose based on recent clinical studies.[8,10,11]
Exercise Testing
Subjects were asked to abstain from food, coffee, and cigarettes for at least 3 h prior to testing. Initially, all subjects received a complete history and physical examination, followed by a maximal exercise test using a manually incremented treadmill protocol. The purpose of this test was to habituate subjects to the procedure and gas exchange apparatus, establish clinical stability, and determine maximal [VO.sub.2]. On study days, an individualized ramp treadmill test was performed.[12] Changes in speed and grade of the treadmill were individualized (based on a given subject's exercise capacity on the baseline test) to yield a test duration of approximately 10 ruin. A standard 12-lead ECG and manual BP were obtained throughout the exercise test and recovery period. The number of QRS complexes multiplied by 10 in a 6-s rhythm strip was used to determine heart rate.[13] Exercise was continued until volitional fatigue, and the Borg 6-20 scale[14] was used to quantify subjective effort.
Gas Exchange
Respiratory gas exchange variables were acquired continuously during exercise using the CS-100 System (Schiller America; Tustin, CA). Variables were recorded using running recursive sums of 30 s of data printed every 10 s.[15] Gas exchange variables analyzed were [VO.sub.2] (mL/kg/min and L/min, standard temperature and pressure, dry), [CO.sub.2] production (L/min, standard temperature and pressure, dry), minute ventilation (VE [L/ruin, body temperature and pressure, saturated]), oxygen pulse ([VO.sub.2] divided by heart rate), and respiratory exchange ratio ([CO.sub.2] output [VCO.sub.2] divided by [VO.sub.2]). The ventilatory threshold was determined using plots of the ventilatory equivalents for [O.sub.2] and [CO.sub.2] and the V-slope method by two independent, blinded (to study phase and the other observer) observers, as outlined previously.[16]
Cardiac Output
Cardiac output was determined during submaximal exercise using a [CO.sub.2] rebreathing technique developed by Defares[17] and described in detail elsewhere.[18] Briefly, this technique is based on the application of [CO.sub.2] rather than [O.sub.2] to the Fick equation:
cardiac output = [VCO.sub.2]/a-[VCO.sub.2] difference
where [VCO.sub.2] is the volume of [CO.sub.2] produced and a-[VCO.sub.2] difference is the difference in the [CO.sub.2] content between the arterial and venous blood. Arterial [CO.sub.2] content is estimated from end-tidal P[CO.sub.2] from gas exchange. Venous [CO.sub.2] content is determined by rebreathing a [CO.sub.2] gas mixture and estimating an equilibrium point between the [CO.sub.2] content of the lung and the venous blood. Software developed by Medical Graphics Corp (St. Paul, MN) was used to make the cardiac output measurements.
After patients had rested for approximately 30 min following the maximal test, a treadmill workload was chosen that represented approximately 50% of the individual's peak [VO.sub.2] on the baseline test. After a warm-up period, patients were taken to their respective 50% workloads until a constant (steady-state) [VO.sub.2] was achieved (5 to 7 min). Patients then began rebreathing a 4% [CO.sub.2]/35% [O.sub.2] gas mixture for a period of 10 to 15 s. An exponential curve for the rise in [VCO.sub.2] was generated, representing the point at which the [CO.sub.2] content of the lung was equal to that of the venous blood. This value for venous [CO.sub.2] content completes the Fick equation, permitting an estimation of cardiac output.
Statistics
Data are presented as mean [+ or -] SD. Student's t tests for paired observations were performed to evaluate differences between hemodynamic and gas exchange data obtained during betaxolol and placebo therapy. Simple linear regression was performed to evaluate the relationship between the change in maximal [VO.sub.2] (betaxolol minus placebo) and hemodynamic responses to exercise.
RESULTS
Clinical characteristics of the 12 patients are presented in Table 1. A 13th patient experienced lightheadedness during betaxolol therapy and was removed from the study. There were otherwise no untoward events during the therapeutic regimens or exercise evaluations.
Resting Data
Heart rate was significantly reduced during betaxolol therapy, both in the supine (92 [+ or -] 27 beats/ min for placebo vs 62 [+ or -] 12 beats/min for betaxolol; p [is less than] 0.001) and standing (99 [+ or -] 23 vs 66 [+ or -] 14 beats/ min; p [is less than] 0.001) positions (Table 2). Systolic BP was reduced only in the supine position during betaxolol therapy.
Table 2--Hemodynamic and Gas Exchange Data During Placebo and Betaxolol Therapy(*)
(*) Values are expressed as mean [+ or -] SD.
Ventilatory Threshold
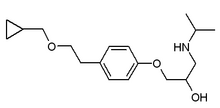
Heart rate at the ventilatory threshold was reduced by 39 beats/min on betaxolol therapy (p [is less than] 0.001), and systolic BP was reduced by 14 mm Hg (p [is less than] 0.01). [VO.sub.2] was reduced by 19% (14.1 [+ or -] 3.8 vs 11.4 [+ or -] 3.1 mL/kg/min; p = 0.09; Fig 1). The ventilatory threshold occurred at a similar percentage of maximal [VO.sub.2] (66 [+ or -] 15% with placebo and 65 [+ or -] 12% with betaxolol), and no differences were observed for VE, exercise time, or perceived exertion at this point.
[Figure 1 ILLUSTRATION OMITTED]
Cardiac Output
Cardiac output, estimated during submaximal exercise by [CO.sub.2] rebreathing, was reduced by 15% during betaxolol therapy (12.9 [+ or -] 2.3 vs 10.9 [+ or -] 1.3; p [is less than] 0.05). Given this reduction in cardiac output and a 43-beat/min reduction in heart rate during steady-state submaximal exercise (p [is less than] 0.001), a significant increase in stroke volume was observed during the betaxolol phase (88.0 [+ or -] 20.8 mL/beat with placebo vs 105.6 [+ or -] 19.4 mL/beat with betaxolol; p [is less than] 0.05).
Maximal Exercise
All patients reported fatigue, leg fatigue, or shortness of breath end points at maximal exertion. During both phases of the study, patients achieved mean respiratory exchange ratios of approximately 1.10 and perceived exertion levels greater than 19, suggesting that maximal effort was generally achieved. No differences were observed between betaxolol and placebo phases for these variables.
Maximal heart rate was reduced considerably by betaxolol (from 173 [+ or -] 22 beats/min with placebo to 116 [+ or -] 24 beats/min with betaxolol; p [is less than] 0.001). A 19% reduction in maximal [VO.sub.2] was observed with betaxolol (21.8 [+ or -] 5.3 vs 17.6 [+ or -] 5.1 mL/kg/min; p [is less than] 0.05; Fig 1), with similar reductions observed for maximal exercise time, VE, and [CO.sub.2] production. Maximal oxygen pulse was significantly higher (2.4 mL/beat) after betaxolol therapy (p [is less than] 0.01).
Relation Between Change in Peak [VO.sub.2] and Hemodynamic Measurements
Correlation coefficients between the change in peak [VO.sub.2] (placebo minus betaxolol) and hemodynamic responses are presented in Table 3. The change in peak [VO.sub.2] was not significantly related to resting or maximal heart rates during placebo therapy, or to changes (placebo minus betaxolol) in resting or maximal heart rates, cardiac output, heart rate range, or stroke volume.
Table 3--Correlation Coefficients Between the Change in Peak [VO.sub.2] (Placebo - Betaxolol) and Hemodynamic Responses(*)
(*) [Delta] = a change in a given variable, placebo minus betaxolol. Heart rate range is the difference between rest and peak exercise heart rate.
DISCUSSION
Ventricular Control and Exercise Capacity
Control of the ventricular response has long been the major therapeutic challenge of treating patients with chronic AF. Previous efforts to control the rapid, irregular heart rate at rest and during exercise have met with mixed results. Digoxin, a mainstay of therapy for this condition, generally fails to control the ventricular rate during exercise.[1,9,19,20] Goldman et al,[19] for example, observed that near-toxic levels of digoxin were required before adequate heart rate control was achieved. Results of studies using [Beta]-blockade therapy have been paradoxical; while adequate heart rate control is generally achieved, exercise capacity is hindered considerably in some studies, but not in others (Table 4). DiBianco et al[7] and Atwood et al[4] observed reductions in exercise capacity after [Beta]-blockade therapy on the order of 15 to 20%, which concurs with the findings in the present study.
Table 4--Summary of Previous Studies on the Effects of [Beta]-Blockade on Maximal Heart Rate and Exercise Capacity in Atrial Fibrillation(*)
(*) All [Beta]-blockers were used in combination with digoxin.
([dagger]) Exercise time.
([double dagger]) Measured oxygen uptake.
Presumably, the considerable reduction in maximal heart rate caused by [Beta]-blockade (25 to 35 beats/min in previous studies), along with its negative inotropic effects, reduces maximal cardiac output and accounts for the reduction in exercise capacity. In studies in which exercise capacity increased after [Beta]-blockade, increases in stroke volume presumably more than compensated for the reductions in heart rate to maintain cardiac output. In the present study, the use of once-daily betaxolol had a striking effect on the ventricular response to exercise; we observed mean reductions of 39 beats/min (29%) at the ventilatory threshold and 57 beats/min (33%) at maximal exercise. Both an inordinately high heart rate response to exercise (a hallmark of AF) and an inordinately reduced heart rate response (as might occur with [Beta]-blockade) are undesirable. The typical uncontrolled ventricular response to exercise in AF probably hinders cardiac output by incomplete and irregular ventricular filling that reduces end-diastolic volume. Conversely, reductions in cardiac output during exercise after [Beta]-blockade have been documented in normal subjects,[21] and have been suggested, although not directly measured, in patients with AF. More than likely, a balance exists at which heart rate is controlled without compromising cardiac output in AF. The differences between the present findings and those of previous studies are likely attributable to the extent to which the ventricular response is controlled in the different populations of patients with AF; factors such as serum digoxin level, concomitant medications, and underlying disease undoubtedly influence the degree of ventricular control.[1,22,23]
Effect of [Beta]-Blockade on Cardiac Output
The determination of cardiac output by submaximal [CO.sub.2] rebreathing is relevant in the context of the present study for several reasons. First, the influence of [Beta]-blockade therapy on cardiac output at rest and during exercise in patients with AF has not been previously studied. Second, the technique is noninvasive, and although particulars concerning methodology have been argued, numerous studies have validated it.[17,18,24 Third, since the technique must be performed submaximally, a steady-state workload can be individualized for a given patient, approximating activities of daily living (mean, 3.0 metabolic equivalents in the present study).
Submaximal cardiac output was reduced by a mean of 2.0 L/min (16%) at this level of exercise after [Beta]-blockade therapy in the present study, a reduction that was commensurate with the reduction in maximal [VO.sub.2]. Submaximal and maximal heart rates were reduced by comparatively greater degrees, suggesting that the compensatory change in stroke volume (which increased by 17.6 mL/beat, or 20%, submaximally) did not adequately compensate for the reduction in heart rate. Interestingly, a trend was observed for an increase in perceived effort at the ventilatory threshold after [Beta]-blockade therapy (p = 0.11), which confirms our previous observations.[4,25] These untoward effects of [Beta]-blockade on cardiac performance, [VO.sub.2] and perceived effort submaximally would appear to be important considerations for patients with AF who continue to work or prefer an active lifestyle.
Effect of [Beta]-Blockade on Individual Patients The effect of betaxolol on maximal [VO.sub.2] varied considerably; most patients demonstrated reductions, whereas several did not change appreciably. We speculated that patients who had the least ventricular control initially would benefit the most from [Beta]-blockade (ie, they would most need a strong negative chronotrope). When we evaluated the relationship between maximal heart rate on placebo vs the change in maximal [VO.sub.2] (placebo minus betaxolol), we found only a modest association (Table 3). Likewise, the relationships between the changes in peak [VO.sub.2] and maximal heart rate, submaximal stroke volume, and the heart rate range (maximum minus rest) were only modest (r = 0.21 to 0.55). Thus, while betaxolol clearly reduced heart rate and cardiac output during exercise, and therefore reduced peak [VO.sub.2], there was considerable variation among patients. Establishing which patients might benefit from [Beta]-blockade therapy on the basis of resting or exercise heart rates remains a difficult undertaking.
SUMMARY
Once-daily betaxolol therapy in patients with chronic AF resulted in significant reductions in the ventricular rate at rest and during exercise. Maximal [VO.sub.2] was significantly reduced, but there was considerable variation among patients. Submaximally, stroke volume increased as a compensatory mechanism for the reduction in heart rate, but it is doubtful that the increase in stroke volume was adequate to maintain cardiac output at higher levels of exercise in most patients. Patients with AF who have a relatively controlled ventricular response may benefit from alternative therapies such as calcium-channel blockers, which have been shown to have significant although more modest effects on heart rate during exercise, and do not attenuate maximal [VO.sub.2].[25]
REFERENCES
[1] Atwood JE, Myers J. Exercise hemodynamics of atrial fibrillation. In: Falk RH, Podrid PJ, eds. Atrial fibrillation: mechanisms and Management, 2nd ed. Philadelphia: Lippincott-Raven, 1997; 219-240
[2] Falk RH. Antithrombotic therapy in atrial fibrillation. In: Falk RH, Podrid PJ, eds. Atrial fibrillation: mechanisms and management. 2nd ed. Philadelphia: Lippincott-Raven, 1997; 277-298
[3] Yahalom J, Klein H, Kaplinsky E. Beta-adrenergic blockade as adjunctive oral therapy in patients with chronic atrial fibrillation. Chest 1977; 71:582-592
[4] Atwood JE, Sullivan M, Forbes S, et al. Effect of beta-adrenergic blockade on exercise performance in patients with chronic atrial fibrillation. J Am Coll Cardiol 1987; 10:314-320
[5] Molajo AO, Coupe MO, Bennett DH. Effect of Corwin (ICI 118587) on resting and exercise heart rate and exercise tolerance in digitalised patients with chronic atrial fibrillation. Br Heart J 1984; 52:392-395
[6] Wong CK, Lau CP, Leung WH, et al. Usefulness of labetalol in chronic atrial fibrillation. Am J Cardiol 1990; 66:1212-1215
[7] DiBianco R, Morganroth J, Freitag JA, et al. Effects of nadolol on the spontaneous and exercise-provoked heart rate of patients with chronic atrial fibrillation receiving stable dosages of digoxin. Am Heart J 1984; 108:1121-1127
[8] Koh KK, Kwon KS, Park HB, et al. Efficacy and safety of digoxin alone and in combination with low-dose diltiazem or betaxolol to control ventricular rate in chronic atrial fibrillation. Am J Cardiol 1995; 75:88-90
[9] Zoble RG, Brewington J, Olukotun AY, et al. Comparative effects of nadolol-digoxin combination therapy and digoxin monotherapy for chronic atrial fibrillation. Am J Cardiol 1987; 60:39D-45D
[10] Christ M, Rauen P, Klauss V, et al. Spontaneous changes of heart rate, blood pressure, and ischemia-type-ST segment depressions in patients with hypertension without significant coronary artery disease: beneficial effects of beta-blockade. J Cardiovasc Pharmacol 1996; 28:755-763
[11] Alpert MA, Mukerji V, Villarreal D, et al. Efficacy of betaxolol in the treatment of stable exertional angina pectoris: a dose-ranging study. Angiology 1990; 41:365-376
[12] Myers J, Buchanan N, Walsh D, et al. Comparison of the ramp versus standard exercise protocols. J Am Coll Cardiol 1991; 17:1334-1342
[13] Atwood JE, Myers J, Sandhu S, et al. Optimal sampling interval to estimate heart rate at rest and during exercise in atrial fibrillation. Am J Cardiol 1989; 69:45-48
[14] Borg G. Perceived exertion as an indicator of somatic stress. Scand J Rehabil Med 1970; 2:92-98
[15] Myers J, Walsh D, Sullivan M, et al. Effect of sampling on variability and plateau in oxygen uptake, J Appl Physiol 1990; 68:404-410
[16] Shimizu M, Myers J, Buchanan N, et al. The ventilatory threshold: method, protocol, and evaluator agreement. Am Heart J 1991; 122:509-516
[17] Defares JG. Determination of [PVCO.sub.2] from the exponential [CO.sub.2] rise during rebreathing. J Appl Physiol 1958; 13:159-164
[18] Myers J. Essentials of cardiopulmonary exercsie testing. Champaign, IL: Human Kinetics, 1996
[19] Goldman S, Probst P, Selzer A, et al. Inefficacy of "therapeutic" serum levels of digoxin in controlling the ventricular rate in atrial fibrillation. Am J Cardiol 1975; 35:651-655
[20] David D, DiSegni E, Klein HO, et al. Inefficacy of digitalis in the control of heart rate in patients with chronic atrial fibrillation: beneficial effect of an added [Beta]-adrenergic blocking agent. Am J Cardiol 1978; 44:1378-1382
[21] Wilmore JH. Exercise testing, training, and beta- adrenergic blockade. Physician Sports Med 1988; 16:45-52
[22] Atwood JE, Myers J, Sullivan M, et al. Maximal exercise testing and gas exchange in patients with chronic atrial fibrillation. J Am Coll Cardiol 1988; 11:508-513
[23] Ueshima K, Myers J, Ribisl PM, et al. Hemodynamic determinants of exercise capacity in chronic atrial fibrillation. Am Heart J 1993; 125:1301-1305
[24] Franciosa JA, Ragan DO, Rubenstone SJ. Validation of the [CO.sub.2] rebreathing method for measuring cardiac output in patients with hypertension or heart failure. J Lab Clin Med 1976; 88:672-682
[25] Myers J, Atwood JE, Sullivan M, et al. Perceived exertion and gas exchange after calcium and [Beta]-blockade in atrial fibrillation. J Appl Physiol 1987; 63:97-104
(*) From the Cardiology Division, Palo Alto Veterans Affairs Health Care System and Stanford University, Palo Alto, CA.
Manuscript received October 6, 1998; revision accepted October 7, 1998.
Correspondence to: J. Edwin Atwood, MD, Cardiology Division (111-C), VA Palo Alto Health Care Systems, 3801 Miranda Ave, Palo Alto, CA 94304
COPYRIGHT 1999 American College of Chest Physicians
COPYRIGHT 2000 Gale Group