* Poldermans D, Boersma E, Bax JJ, et al. The effect of bisoprolol on perioperative mortality and myocardial infarction in high-risk patients undergoing vascular surgery. N Engl J Med 1999; 341:1789-94.
CLINICAL QUESTION
Does the perioperative administration of bisoprolol prevent nonfatal myocardial infarction (MI) or cardiovascular mortality in high-risk patients undergoing vascular surgery?
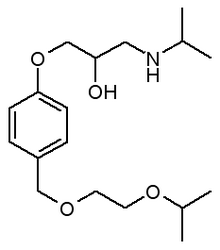
BACKGROUND * Many patients suffer from cardiovascular complications following major vascular surgery, and although various interventions have been proposed to improve the associated cardiovascular risks, none has been found to be efficacious. Since [Beta]-blockers demonstrate a major benefit in acute MI and other cardiovascular diseases, investigators studied the benefit of bisoprolol when given perioperatively to high-risk patients undergoing vascular surgery. Bisoprolol is a [Beta]-1 selective hydrophilic [Beta]-blocker without intrinsic sympathomimetic activity.
POPULATION STUDIED * All of the included patients were undergoing elective abdominal aortic or infrainguinal arterial reconstruction at study sites in Canada, the Netherlands, and Italy. Patients with cardiac risk factors -- older than 70 years, previous MI, treatment for congestive heart failure, ventricular arrhythmias, diabetes mellitus, or reduced capacity to perform activities of daily living -- underwent dobutamine stress echocardiography. Those with a positive result were considered to be high risk and were included in the study. Patients were excluded if they had significant heart wall motion abnormalities, asthma, or evidence of left main or triple coronary vessel disease during stress testing. A total of 1351 patients were screened, and 846 were found to have cardiac risk factors. Positive stress tests were documented in 173 patients, and 112 underwent randomization (59 bisoprolol plus standard care, 53 standard care alone). More than 80% of the patients were men.
STUDY DESIGN AND VALIDITY * This was a multicenter randomized controlled trial in which patients received standard perioperative care or standard care plus bisoprolol. Bisoprolol 5 mg daily was initiated at least 1 week before surgery (mean = 37 days before surgery; range = 7 to 89 days), and continued for 30 days postoperatively. Approximately 1 week after initiation, patients were reassessed and the dosage could be increased to a maximum of 10 mg daily if the heart rate remained at more than 60 beats per minute (bpm). Administration by nasogastric tube or intravenous metoprolol was substituted at times when patients were unable to take the medication orally. Bisoprolol was withheld if the heart rate dropped below 50 bpm or if the systolic blood pressure was less than 100 mm Hg.
Overall, the methods of this study were appropriate to answer the clinical question. Although physicians and patients were not blinded during the study, a monitoring committee evaluated outcomes in a masked fashion. The authors did not describe the methods used to prevent researchers from knowing to which group the patient would be assigned (concealed allocation). This lack of concealment could introduce selective enrollment of patients. The patient population studied was elderly; therefore, the impact of bisoprolol in younger or lower-risk patients undergoing vascular surgery may be less dramatic.
OUTCOMES MEASURED * The primary end points were death from cardiac causes or nonfatal myocardial infarction during the perioperative period.
RESULTS * The bisoprolol-treated group experienced fewer deaths (3.4% vs 17%, P=.02; number needed to treat [NNT]=7.3) and fewer nonfatal MIs (0% vs 17%, P [is less than] .001; NNT=5.9) than those receiving standard care alone. For the combined end point of death from cardiac causes or nonfatal MI, the overall rate in the bisoprolol group was 3.4% vs 34% in the standard care group (P [is less than].001; NNT=3.3). The study was stopped after interim analysis because of the significant difference between groups. Investigators did not report side effects associated with the administration of bisoprolol.
RECOMMENDATIONS FOR CLINICAL PRACTICE
This well-designed clinical trial demonstrates the major impact of perioperative administration of the [Beta]-blocker bisoprolol in high-risk patients undergoing vascular surgery. For every 3 high-risk patients treated, one death or nonfatal MI is prevented. It is not known if the benefits associated with bisoprolol will be realized with the use of other [Beta]-blockers.
--Lori M. Dickerson, PharmD Peter J. Carek, MD, MS Medical University of South Carolina Charleston E-mail: macfarl@musc.edu
COPYRIGHT 2000 Appleton & Lange
COPYRIGHT 2001 Gale Group