* Evidence summary
In recent years, beta-blockers have been shown to substantially decrease mortality in patients with congestive heart failure, coronary heart disease, and hypertension. Patients with both cardiovascular disease and COPD, however, are much less likely to receive beta-blocker therapy than comparable patients without COPD. Clinicians may be fearful of using beta-blockers in these patients because of the possibility of worsening respiratory function from the potential side effect of bronchoconstriction. (1)
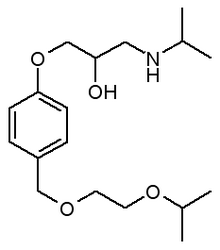
A 2004 meta-analysis synthesized the data of 19 clinical controlled trials that compared active therapy with either placebo or prior-to-treatment controls, assessing differences in FE[V.sub.1], response to a [beta.sub.2]-agonist, and patient-reported respiratory symptoms. (2) Trials included in the meta-analysis used cardioselective beta-blockers and evaluated either single-dose treatments or therapy of longer duration (2 days to 3.3 months). The authors concluded that patients with COPD who received cardioselective beta-blockers (such as metoprolol, atenolol, or bisoprolol) did not experience a statistically significant short-term deterioration in FE[V.sub.1], worsening of COPD symptoms, or decreased responsiveness to [beta.sub.2]agonists. The authors reported similar results for an analysis restricted to only those patients with severe COPD.
This meta-analysis was limited by the relatively small number of participants (N = 141 in single-dose treatment studies; N = 126 in studies of longer duration treatment) in the handful of eligible studies. Consequently, rare or minimally harmful effects could have gone undetected.
A retrospective analysis of a cohort study analyzed the tolerability of carvedilol, a nonselective beta- and alpha-adrenergic blocker, in patients with COPD who had been taking the medication for at least 3 months. Eighty-five percent of the 89 patients with COPD tolerated carvedilol. The authors of the study (which was funded by the manufacturer of carvedilol) did not state why the other 15% of patients did not tolerate carvedilol, nor did they mention whether the patients with COPD had reversible airflow obstruction. (3)
One of the sites that participated in this study subsequently published a smaller retrospective analysis of a cohort study that examined the outcomes of 31 patients with heart failure and COPD without reversible airflow obstruction who were started on carvedilol therapy. Over the 2.4 years that the patients were followed, 1 patient stopped taking carvedilol (mean dose 29 [+ or -] 19 mg daily) due to wheezing. (4) Whether these 31 patients were also included in the larger study is unclear.
A 2004 narrative review article cited these 2 studies and concluded that carvedilol was well-tolerated in patients with COPD without reversible airflow obstruction, but no evidence exists regarding its tolerability in patients with reversible airflow obstruction. (5)
Recommendations from others
A 2002 evidence-based clinical guideline on the diagnosis and management of COPD reported that the use of cardioselective betablockers in patients with COPD did not significantly worsen respiratory status, citing a previous version of the meta-analysis reviewed above as its source of evidence. (6) The American College of Cardiology and the American Heart Association recommended the cautious administration of low-dose, short-acting cardioselective betablockers for acute coronary syndrome in patients with COPD. (7)
A recent consensus workshop summary report issued by experts convened by the National Heart, Lung, and Blood Institute, cited continuing uncertainty regarding the use of beta-blockers for COPD patients with heart disease, and called for additional studies of management strategies for these often-coexisting conditions. (8)
REFERENCES
(1.) Andrus MR, Holloway KP, Clark DB. Use of beta-blockers in patients with COPD. Ann Pharmacother 2004; 38:142-145.
(2.) Salpeter SS, Ormiston T, Salpeter E, Poole P, Cates C. Cardioselective beta-blockers for chronic obstructive pulmonary disease (Cochrane Review). Cochrane Database Syst Rev 2005;(1).
(3.) Krum H, Ninio D, Macdonald R Baseline predictors of tolerability to carvedilol in patients with chronic heart failure. Heart 2000; 84:615-619
(4.) Kotlyar E, Keogh AM, Macdonald PS, Arnold RH, McCaffrey DJ, Glanville AR. Tolerability of carvedilol in patients with heart failure and concomitant chronic obstructive pulmonary disease or asthma. J Heart Lung Transplant 2002; 21: 1290-1295.
(5.) Sirak TE, Jelic S, Le Jemtel TH. Therapeutic update: non-selective beta- and alpha-adrenergic blockage in patients with coexisting chronic obstructive pulmonary disease and chronic heart failure. J Am Coil Cardiol 2004; 44:497-502.
(6.) Finnish Medical Society Duodecim. Chronic Obstructive Pulmonary Disease (COPD). Helsinki, Finland: Duodecim Medical; 2002.
(7.) Braunwald E, Antman EM, Beasley JW, et al. ACC/AHA 2002 guideline update for the management of patients with unstable angina and non-ST-segment elevation myocardial infarction: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee on the Management of Patients With Unstable Angina). 2002. Available at: vwvw.acc.org/clinical/guidelines/unstable/unstable.pdf.
(8.) Croxton TL, Weinmann GG, Senior RM, Wise RA, Crapo JD, Buist AS. Clinical research in chronic obstructive pulmonary disease: needs and opportunities. Am J Respir Crit Care Med 2003; 167:1142-1149.
FAST TRACK
Cardioselective beta-blockers do not significantly worsen shortterm pulmonary status in COPD
COPYRIGHT 2005 Dowden Health Media, Inc.
COPYRIGHT 2005 Gale Group