Once upon a time, not too long ago, heart failure (HF) was easy. We understood that the heart was a pump and that it functioned poorly in a variety of situations. We then used medication, such as a digitalis preparation, to increase contractility. We treated the edema and other symptoms with diuretics, sodium restriction, and bed rest. Our patients usually felt better, particularly after the loss of excess fluid. However, their 2-year survival was often no better than patients with cancer: 50%.
Well, things have changed greatly, and for the better. Dr. Wilbert Aronow's excellent review of cardiac resynchronization therapy (CRT) and the implantable cardioverter-defibrillator (ICD) demonstrates the more recent changes (see pages 24--28). (1)
Today, we understand better the molecular, cellular, and anatomical changes that occur with myocardial injury. (2) We are cognizant of the pathophysiology of HF, particularly the neurohormonal compensations involving the sympathetic and the renin--angiotensin--aldosterone systems that often are excessive and harmful--and we base our therapy on these. (2) We speak about compensatory cardiac remodeling and the vicious cycle this causes in congestive heart failure. (2) Now, our evaluation and therapy has become much more complicated and involved, but with outstanding improvement in morbidity and mortality. (3)
Until a few years ago, we classified our HF patients on the basis of symptoms alone using the New York Heart Association Classification. This allowed us to assign a prognosis for our patients. Now, with all of our new treatment modalities, we wish to intervene early and prevent the progression of HF and diminish both its morbidity and mortality. Toward this end, the American Heart Association and the American College of Cardiology have added a second classification based not on symptoms, but on risk factors and structural alterations--the Stages of Heart Failure Classification. (3)
We also are aware that there is both systolic and diastolic heart failure. The latter is associated with a normal or near normal ejection fraction and is due to such things as hypertrophic cardiomyopathy, hypertension, and other conditions that either stiffen or restrict the filling of the heart. Diastolic failure is treated differently than the usual patient with systolic heart failure. (3)
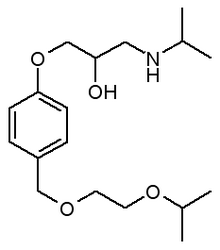
Our treatment of systolic heart failure now begins with investigation of the cause of cardiac difficulty and any structural abnormality, particularly with the use of echocardiography and, occasionally, nuclear cardiology. (3) Treatment of reversible causes is essential. These include the elimination of drugs that depress cardiac function (table) and aggressive treatment for potentially reversible diseases that adversely impact the heart, such as myocardial ischemia, thyroid dysfunction, sleep apnea, renal failure, anemia, and hypoxemia, to name just a few.
Standard therapy includes an angiotensin converting enzyme (ACE) inhibitor or an angiotensin receptor blocker (ARB). If an ACE inhibitor is not tolerated, a beta-blocker (BB), an aldosterone inhibitor (AI), or possibly a diuretic or digoxin may be prescribed. (3) Significant symptomatic relief is accompanied often with anatomical improvement (eg, better ejection fraction, some reversal of remodeling), and best of all, decreased mortality. Recent literature debates include discussion of whether one ACE inhibitor is superior to another; whether ARBs--often used when patients are intolerant to ACE inhibitors--are as good as or better than ACE inhibitors as initial therapy (given the lesser side effects), and whether the combination of an ACE inhibitor and an ARB might prove beneficial in some patients. (4,5,6)
There is contention as to which of the 3 approved BB for HF to use (carvedilol, long-acting metoprolol, or bisoprolol). (7,8) Some are now advocating that we start with the BB before the ACE inhibitor or ARB.
Debate also continues regarding the place of digoxin in the HF patient in sinus rhythm. The new aldosterone inhibitor, eplerenone, seems to theoretically have less endocrine side effects than spironolactone, but it costs much more. Aldosterone inhibitors in low dose are now Class 1 recommended by the cardiology guidelines for all HF patients. (9,10)
We are learning to use diuretics--which can cause dehydration, decrease renal blood flow, and increase rennin-angiotensin-aldosterone production--in smaller dosages. The use of hydralazine plus nitrates for the patient who is unable to tolerate an ACE inhibitor or ARB is always an option, as is the use of this combination as a supplement for the patient who fails usual therapy. A recent study adding this combination to standard therapy (BB+ACE inhibitor +AI) in African-American patients resulted in further improvement in survival. (11)
Anticoagulation raises yet another controversy. Certainly the HF patient in atrial fibrillation or a patient who has experienced a previous embolic episode benefits from this therapy. But what about the rest of the HF patients? Are they not also at risk with a dilated ventricle (often the atrium too) and stasis of blood flow? Another debate and another unanswered question. (3)
Increased survival has also been documented when a statin is included in the HF regimen. (3)
On the near horizon, possible future interventions include vasopeptidase inhibitors, endothelin receptor antagonists, natriuretic peptides, and stem cell therapy. (3)
Cardiac assist devices have captured our imagination for many years, but have yet not proven to be a long-term success. Cardiac transplantation has an excellent record, but the available resources (eg, human hearts) markedly limit its use. (12)
The majority of our HF patients have ventricular premature beats and many have episodes of ventricular tachycardia (VT). We have known for some time that up to one-third of the deaths in patients with HF are from sudden cardiac death (SCD), and that many of these might be prevented by an implanted defibrillator. Drug trials to suppress VT and prevent SCD have not been very successful, (13,14) but several trials have demonstrated a mortality benefit with the implantable cardioverter-defibrillator (ICD). (12,14,15)
Now the debate is over to whom this device should be offered. It should certainly be offered for secondary protection to patients at risk for SCD, ventricular fibrillation, and sustained or symptomatic nonsustained VT. But what about primary therapy for the patient at risk, such as those with reduced left ventricular ejection fraction (LVEF) post MI or congestive cardiomyopathy? Several clinical trials have shown not only significant benefit, but also improved survival, (12,14,15) and many now recommend that all patients with an ejection fraction less than 30% to 35% should receive an ICD in addition to the standard medical therapy as noted above. (14,15) The economics of this alone is staggering: An ICD, including the device, hospitalization, and professional fees, can cost $40,000 or more.
Now we come to an even greater economic dilemma, biventricular pacing. Cardiac dyssynchrony in HF has been demonstrated for some time. This occurs usually in association with a conduction delay, most often left bundle branch block. There have been numerous trials, as detailed in Dr. Aronow's article, showing improvement functionally and symptomatically with this device in the HF patient who has an abnormal LVEF and a QRS duration of 120 msec or more. (16,17,18,19) A significant reduction in mortality with CRT was also found in a recent trials. (18,19) Unlike a pacemaker or an ICD, CRT requires a good deal of expertise. The third lead must be placed in the coronary sinus, and not all invasive cardiologists are adept at this. This can be further complicated by altered cardiac anatomy in dilated cardiomyopathy, and the procedure is associated with significant complications as well as great difficulty if this lead needs to be removed.
Many now are advocating a combined CRT-ICD as appropriate therapy for all patients with decreased LVEF and conduction delay. But what about the cost? The combined CRT-ICD devices cost upwards of $25,000, not including hospital and professional fees. Dr. Aronow suggests that 35,000 patients annually, in addition to the 100,000 or more eligible for ICD alone, will possibly need the CRT-ICD! The projected costs are staggering and will be in the billions!
As our knowledge and abilities continue to grow, we can expect even more benefit coupled with more controversy. There are now implantable devices in development that can monitor and display almost all aspects of cardiac function. (12) These devices may enable us to better select the most appropriate treatment for each patient. Several of these in stage 3 development will allow the patient to self monitor with his or her PDA, and daily adjust medical therapy similar to patient glucose monitoring!
Who knows what other new modifications in our therapy linger just around the corner? We have come a long, long way since the era of digitalis, diuretics, and bed rest therapy. For those of us in practice in that era, the therapies of today are wondrous and exciting, but the concern for the price tag lingers.
References
(1.) Aronow W. CRT plus ICD in congestive heart failure: Use of cardiac resynchronization therapy and an implantable cardioverter-defibrillator in heart failure patients with abnormal left ventricular dysfunction. Geriatrics 2005; 60(5):24-28.
(2.) Pina IL. Etiology, pathophysiology, and diagnosis of heart failure; Cardiology review 2003; 20(11 Suppl): 6-11.
(3.) Hunt SA, Baker DW, Chin MH, et al, and the American College of Cardiology and the American Heart Association Task Force on Practice Guidelines. (Committee to revise the 1995 Guidelines for the Evaluation and Management of Heart Failure). ACC/AHA guidelines for the evaluation and management of chronic congestive heart failure in the adult. American College of Cardiology website. Available at: http://www.acc.org/clinical/ guidelines /failure/hf_index.htm. Accessed January 21, 2005.
(4.) Garg R, Yusuf S, and the Collaborative Group on ACE Inhibitor Trials. Overview of randomized trials of angiotensin-converting enzyme inhibitors on mortality and morbidity in patients with heart failure. Collaborative Group on ACE-Inhibitor Trials. JAMA 1995; 273(18):1450-6.
(5.) Pitt B, Poole-Wilson PA, Segal R, et al. Effects of Losartan compared with captopril on mortality in patients with symptomatic heart failure: randomized trial-the Losartan Heart Failure Survival Study ELITE II. Lancet 2000; 355(9215):1582-7.
(6.) McMurray JJ, Ostergen J, Swedberg K, et al, and the CHARM Investigators and Committees. Effects of candesartan in patients with chronic heart failure and reduced left-ventricular function taking angiotensin-converting-enzyme inhibitors: the CHARM-Added trial. Lancet 2003; 362(9386):767-71.
(7.) Newton GE, Parker JD. Acute effects of beta 1-selective and nonselective beta-adrenergic receptor blockade on cardiac sympathetic activity in congestive heart failure. Circulation 1996; 94(3):353-8.
(8.) Poole-Wilson PA, Swedberg K, Cleland JG, et al, and the Carvedilol Or Metoprolol European Trial Investigators. Comparison of carvidolol and metropolol on clinical outcomes in patients with chronic heart failure in the Carvedilol or Metoprolol European Trial (COMET): a randomized trial. Lancet 2003; 362(9377):7-13.
(9.) Pitt B, Zannad F, Remme WJ, et al. The effects of spironolactone on morbidity and mortality in patients with severe heart failure. N Engl J Med 1999; 341(10):709-17.
(10.) Pitt B, Remme W, Zannad F, et al, and the Eplerenone Post-Acute Myocardial Infarction Heart Failure Efficacy and Survival Study Investigators. Eplerenone, a selective aldosterone blocker, in patients with left ventricular dysfunction after myocardial infarction. N Engl J Med 2003; 348(14):1309-21.
(11.) Taylor AL, Ziesche S, Yancy C, et al. Combination of isosorbide dinitrate and hydralazine in blacks with heart failure. N Engl J Med 2004; 351(20):2049-57.
(12.) Boehmer JP. Device therapy for heart failure. Am J Cardiol 2003; 91(6A) 53D-59D.
(13.) Massie BM, Fisher SG, Radford M, et al, and the African-American Heart Failure Trial Investigators. Effect of amiodarone on clinical status and left ventricular function in patients with congestive heart failure. Circulation 1996; 93(12):2128-34.
(14.) Bardy GH, Lee KL, Mark DB, et al, and the Sudden Cardiac Death in Heart Failure Trial (SCD-HeFT) Investigators. Amiodarone or an implantable cardioverter-defibrillator for congestive heart failure. N Engl J Med 2005; 352(3):225-37.
(15.) Greenberg H, Case RB, Moss AJ, Brown MW, Carroll ER, Andrews MC, and the MADIT-II Investigators. Analysis of mortality events in the Multi-Center Automatic Defibrillator Implantation Trial (MADIT-II). J Am Coll Cardiol 2004; 43(8):1459-65.
(16.) Abraham WT, Fisher WG, Smith AL, et al, and the MIRACLE study group. Multicenter InSync Randomized Clinical Evaluation. Cardiac resynchronization in chronic heart failure. N Engl J Med 2002; 346(24):1845-53.
(17.) Bristow MR, Saxon LA, Boehmer J, et al, and the Comparison of Medical Therapy, Pacing, and Defibrillation in Heart Failure (COMPANION) Investigators. Cardiac-resynchronization therapy with or without an implantable defibrillator in advanced chronic heart failure. N Engl J Med 2004; 350(21):2140-50.
(18.) Auricchio A, Stellbrink C, Sack S, et al, and the Pacing Therapies in Congestive Heart Failure (PATH-CHF) Study Group. Long-term clinical effect of hemodynamically- optimized cardiac resynchronization therapy in patients with heart failure and ventricular conduction delay. J Am Coll Cardiol 2002; 39(12):2026-33.
(19.) Bradley DJ, Bradley EA, Baughman KL, et al. Cardiac resynchronization and death from progressive heart failure: a meta-analysis of randomized controlled trials. JAMA 2003; 289(6):730-40.
Dr. Leibovitch is senior attending physician and coordinator of internal medicine education, Ventura County Medical Center, and adjunct professor of medicine, University of California, Los Angeles, School of Medicine. Disclosure: The author has no real or apparent conflict of interest related to the suject under discussion.
COPYRIGHT 2005 Advanstar Communications, Inc.
COPYRIGHT 2005 Gale Group