Imatinib mesylate is a potent and specific tyrosine kinase inhibitor against c-ABL, BCR-ABL, and c-KIT, and has been demonstrated to be highly active in chronic myeloid leukemia and gastrointestinal stromal tumors. We examined the antifibrotic effects of imatinib using a bleomycin-induced lung fibrosis model in mice because imatinib also inhibits tyrosine kinase of platelet-derived growth factor receptors (PDGFRs). Imatinib inhibited the growth of primary murine lung fibroblasts and the autophosphorylation of PDGFR-β induced by PDGF. Administration of imatinib significantly prevented bleomycin-induced pulmonary fibrosis in mice, partly by reducing the number of mesenchymal cells incorporating bromodeoxyuridine. Analysis of bronchoalveolar lavage cells demonstrated that imatinib did not suppress early inflammation on Days 7 and 14 caused by bleomycin. These results suggest that imatinib has the potential to prevent pulmonary fibrosis by inhibiting the proliferation of mesenchymal cells, and that imatinib might be useful for the treatment of pulmonary fibrosis in humans.
Keywords: fibroblast; platelet-derived growth factor; tyrosine kinase
Idiopathic pulmonary fibrosis (IPF) is a progressive and lethal lung disease characterized by the proliferation of fibroblasts and deposition of extracellular matrix, including fibrillar collagens, fibronectin, elastic fibers, and proteoglycans (1, 2). Although corticosteroids and other immunosuppressants have been used for the treatment of patients with IPF, the response rate to these agents was low, and the 5-year survival rate of patients with IPF is less than 50% (3, 4). For this reason, novel therapeutic modalities are of strong interest.
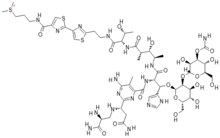
Imatinib mesylate (previously called STI571; Gleevec in the United States, and Glivec in Europe) is a potent and specific tyrosine kinase inhibitor against c-ABL, BCR-ABL, and C-KIT. Imatinib has been demonstrated to be highly active in chronic myeloid leukemia and gastrointestinal stromal tumors (5-8). The reported data regarding the specificity of imatinib for various tyrosine kinases show that imatinib also specifically inhibits platelet-derived growth factor receptor (PDGFR) tyrosine kinase (9). It is known that PDGF is one of the growth factors that plays a role in the pathogenesis of pulmonary fibrosis (10, 11). Maeda and coworkers (12) reported that expression of the PDGF-A gene increased in bleomycin-induced pulmonary fibrosis models in mice using semiquantitative reverse transcriptase-polymerase chain reaction (12). Adoptive transfer of an adenovirus expressing the PDGF-B gene into the lung induced severe fibrosis in mice (13). On the other hand, enhanced expression of PDGF in the epithelial cells and alveolar macrophages in lungs of patients with IPF has been reported (14, 15). These results suggest that inhibition of PDGF action might be a major target for pulmonary fibrosis.
Therefore, we examined whether imatinib could prevent pulmonary fibrosis induced by bleomycin in mice. This article reports the profound antifibrotic effects of imatinib for pulmonary fibrosis, and these results suggest that imatinib might be useful for the treatment of patients with pulmonary fibrosis as a novel antifibrotic agent. Some of the results of these studies have been previously reported in the form of abstracts (16, 17).
METHODS
Detailed methods are described in the online supplement.
Mice and Material
Eight-week-old C57BL/6 female mice were purchased from Charles River Japan, Inc. (Yokohama, Japan). Mice were maintained in the animal facility of the University of Tokushima under specific pathogen-free conditions according to the guidelines of our university (18). Imatinib mesylate was provided by Dr. Elisabeth Buchdunger (Novartis, Basel, Switzerland). Bleomycin was purchased from Nippon Kayaku Co. (Tokyo, Japan). PDGF-AA and PDGF-BB were obtained from Sigma-Aldrich (St. Louis, MO). Epidermal growth factor and fibroblast growth factor 2 were purchased from R&D Systems (Minneapolis, MN). Antimurine PDGFR-β (M-20), antiphosphorylated tyrosine (PY99), and horseradish peroxidase-conjugated antimouse IgG antibodies were purchased from Santa Cruz Biotechnology (Santa Cruz, CA).
Bleomycin Treatment
Osmotic minipumps (model 2001; Alza Pharmaceuticals, Palo Alto, CA) containing 200 µl of saline with or without bleomycin (125 mg/kg) were implanted subcutaneously (19). Each experiment was performed in at least four mice per group.
Administration of Imatinib
The imatinib powder was dissolved in distilled water (Otsuka Pharmaceutical Co., Tokushima, Japan). Imatinib (25 or 50 mg/kg/day) or water was injected intraperitoneally.
Bronchoalveolar Lavage
Bronchoalveolar lavage was performed live times with saline (1 ml) using a soft cannula. After counting cell number of the bronchoalveolar lavage fluid, cells were cytospun onto glass slides and stained with Diff-Quick (Baxter, Miami, FL) for cell classification.
Collagen Assay
The right lungs harvested on Day 28 were used for collagen assay. Total lung collagen was determined using the Sircol Collagen Assay kit (Biocolor Ltd., Belfast, Northern Ireland) according to the manufacturer's instructions (20).
Histopathology
The left lungs were fixed in 10% buffered formalin and embedded in paraffin. Sections (3-4 µm) were stained with hematoxylin and eosin. For the quantitative histologic analysis, a numeric fibrotic scale was used (Ashcroft score) (21). The mean score was considered the fibrotic score. Masson's trichromc staining was also performed.
Fibroblast Isolation
Murine lung fibroblasts were generated according to the method reported by Phan and colleagues (22). These fibroblasts were used at 5 to 10 passages.
Proliferation Assay
Cell proliferation was determined by the incorporation assay of [^sup 3^H]thymidine deoxyribose (18). In some experiments, the cell proliferation was also evaluated by counting the number of cells. The experiments were performed in triplicate cultures.
Immunoblotting
Fibroblasts were cultured in RPMI 1640 (GIBCO, Grand Island, NY) with PDGF-BB (10 ng/ml) and various concentrations of imatinib for 10 minutes. These cells were lysed and used for immunoblotting as previously described (23). The intensity of the bands was quantified using the public domain National Institutes of Health image program (W. Rasband, Research Service Branch, National Institutes of Health, Bethesda, MD).
Bromodeoxyuridine Immunohistochemistry
Bromodeoxyuridine (Brdu) labeling reagent and Brdu staining kit (Zymed Laboratories, Inc., South San Francisco, CA) were used for the detection of the proliferating cells in vivo according to the manufacturer's instruction.
Statistical Analysis
Comparisons among multiple groups were analyzed using the one-way analysis of variance with Newman-Keuls post hoc correction (GraphPad Prism, version 3.0; GraphPad Software, Inc., San Diego, CA). Differences were considered statistically significant if p values were less than 0.05.
RESULTS
Effect of Imatinib on the Growth of Lung Fibroblasts Stimulated by PDGF
As shown in Figures 1A and 1B, both PDGF-AA and PDGF-BB induced DNA synthesis of NIH3T3 and primary lung fibroblasts. The addition of imatinib significantly inhibited the proliferative responses of these fibroblasts in a dose-dependent manner. These results were confirmed directly by counting the number of fibroblasts (Figure 1C). However, imatinib did not affect the proliferative responses of lung fibroblasts stimulated with epidermal growth factor and fibroblast growth factor 2 (Figure 1D). The growth-inhibitory effects of imatinib were observed even when imatinib was used at 0.1 to 0.3 µM. Imatinib at a dose of 10 µM was slightly toxic to NIH3T3 cells as described previously (24), but not to primary lung fibroblasts (data not shown).
Imatinib Inhibited the Tyrosine Kinase Activity of PDGFR in Lung Fibroblasts
Next, we examined the effect of imatinib on the tyrosine kinase activity of PDGFR in lung fibroblasts. The cells were stimulated with PDGF-BB in the presence of various doses of imatinib for 10 minutes. The autophosphorylation of tyrosine of PDGFR-β was analyzed by immunoblotting. As shown in Figure 2, PDGF-BB stimulated the tyrosine phosphorylation of PDGFR-β in both NIH3T3 and primary lung fibroblasts. Imatinib dose-dependently inhibited the tyrosine phosphorylation of PDGFR-β in both cells, which was consistent with the growth-inhibitory effects shown in Figure 1.
Administration of Imatinib Ameliorated Bleomycin-induced Lung Fibrosis in Mice
We further examined the in vivo antifibrotic effects of imatinib using a bleomycin-induced lung fibrosis model in C57BL/6 mice. As shown in Figure 3, administration of imatinib alone did not generate any changes in lung morphology. However, when imatinib was administered in bleomycin-treated mice, a reduction of fibrotic lesions in the subpleural areas of lung was observed at doses of 25 and 50 mg/kg/day. The quantitative histologic analysis demonstrated that the fibrotic score in mice treated with bleomycin and 50 mg/kg/day of imatinib was significantly lower than that treated with bleomycin alone (0.57 ± 0.53 vs. 2.11 ± 0.6, p
Cell Analysis of Bronchoalveolar Lavage Fluid
Next, we analyzed the cells in bronchoalveolar lavage fluid to evaluate the effect of imatinib on the accumulation of inflammatory cells to the lung induced by bleomycin. Administration of bleomycin elevated the number of inflammatory cells, including macrophages, lymphocytes, and neutrophils, on Days 7, 14, and 28 (Table 1). Analysis of cell classification also showed that bleomycin treatment enhanced the percentages of lymphocytes and neutrophils on Days 7, 14, and 28. Treatment with imatinib did not change the number or classification of these inflammatory cells on Days 7 and 14, whereas it significantly reduced the percentage of lymphocytes on Day 28 (Table 1).
Inhibition of Mitogenesis In Vivo by Treatment with Imatinib in Bleomycin-induced Lung Fibrosis
To analyze the mechanisms by which imatinib attenuates bleomycin-induced lung fibrosis, we examined whether imatinib inhibits the proliferation of lung fibroblasts in vivo using Brdu on Day 14. In nontreated mice, some Brdu-positive cells, which indicate the proliferating cells, were observed in the alveolar walls, but not in interalveolar spaces of the lung (Figure 5A). The treatment with bleomycin apparently increased the number of Brdu-positive cells in interalveolar spaces, but not in the alveolar walls, suggesting the existence of proliferating mesenchymal cells (Figures 5A and 5B). The coadministration of imatinib with bleomycin significantly reduced the number of Brdu-positive cells in interalveolar spaces, but not in the alveolar walls, indicating that imatinib inhibited the proliferation of mesenchymal cells.
Time Kinetics of Bleomycin-induced Pulmonary Fibrosis and Antifibrotic Effects of Imatinib
Figure 6 shows the kinetics of lung fibrosis induced by bleomycin in this model. Fourteen days after bleomycin administration, fibrotic lesions clearly developed in the subpleural area of the lung and progressed to Day 28. Treatment with imatinib apparently prevented the development of fibrotic lesions in the lung from Day 14. To further examine the time kinetics of the antifibrotic effects of imatinib, mice were separately treated with imatinib from Days 0 to 14 (early treatment) or Days 14 to 28 (late treatment). As shown in Figure 7, early treatment with imatinib significantly prevented the development of pulmonary fibrosis, whereas the late treatment failed to attenuate the lung fibrosis. Quantitative analysis of fibrotic changes in the lung demonstrated that early treatment, but not late treatment with imatinib resulted in a significant reduction in both fibrotic score and collagen content.
DISCUSSION
The present study demonstrated that imalinib effectively inhibited the growth of lung fibroblasts in vitro and suppressed the autophosphorylation of PDGFR. Furthermore, imatinib significantly attenuated bleomycin-induced lung fibrosis in mice. These in vivo antifibrotic effects of imatinib were partly mediated by inhibiting the proliferation of mesenchymal cells.
PDGF has been reported to play a role in the pathogenesis of pulmonary fibrosis (10, 11). There were two reports describing targeted therapy for PDGF to prevent pulmonary fibrosis. Yoshida and coworkers (25) reported that the in vivo gene transfer of an extracellular domain of PDGFR-β reduced bleomycin-induced pulmonary fibrosis. Another report by Rice and colleagues (26) demonstrated that AG1296, the inhibitor for the tyrosine kinase of PDGFR, prevented pulmonary fibrosis induced by vanadium pentoxide (V^sub 2^O^sub 5^) in rats. These results together with our findings suggest that inhibition of PDGF action might be a possible strategy in preventing pulmonary fibrosis. However, imatinib also suppresses the tyrosine kinase activities of c-ABL and c-KIT. We cannot rule out the possibility that the inhibitory activities for other tyrosine kinases, including these kinases, as well as other biochemical actions of imatinib were involved in the ability to attenuate bleomycin-induced pulmonary fibrosis. Further studies to clarify the mechanisms of antifibrotic effects of imatinib in vivo are required.
The present study used a bleomycin-induced murine model, which has been extensively used to analyze the mechanism of pulmonary fibrosis. Although there is no completely satisfactory animal model of human IPF, the bleomycin-induced model is relatively well characterized and does exhibit certain features found in the human disease. Furthermore, the murine model using a high-dose continuous infusion system of bleomycin with an osmotic minipump produced patchy fibrosis in the subpleural lesion, partly resembling IPF in humans (19, 27, 28).
Imatinib did not affect the number or classification of inflammatory cells in bronchoalveolar lavage fluid induced by bleomycin on Days 7 and 14, indicating that imatinib attenuates bleomycin-induced pulmonary fibrosis without inhibiting early inflammation. Nakao and coworkers (28) and Wang and colleagues (29) reported that blocking the signal pathway of transforming growth factor β using transduction of adenovirus expressing Smad7 or injection of soluble transforming growth factor-β receptor resulted in the reduction of pulmonary fibrosis without antiinflammatory effects in the bleomycin model. The present study demonstrated that imatinib reduced the number of Brdu-incorporating cells in interalveolar spaces of the lung treated with bleomycin, indicating that imatinib can inhibit the proliferation of mesenchymal cells, presumably including fibroblasts in vivo. These results suggest that targeted inhibition for growth factors that stimulate the migration, proliferation, and collagen production of fibroblasts may reduce fibrosis independent of accumulation of inflammatory cells. On the other hand, we observed the significant reduction of lymphocytes in mice treated with bleomycin and imatinib on Day 28 as compared with those treated with bleomycin alone. The reason for the difference in the number of lymphocytes on Day 28 is still unclear. Imatinib may have direct effects on the lymphocyte population during the late phase of the bleomycin model that are different from the early phase, or activated fibroblasts may affect the recruitment or proliferation of lymphocytes in the late stage of fibrosis. This finding is a target of future experiments.
Interestingly, the early treatment (from Days 0 to 14) with imatinib significantly inhibited bleomycin-induced pulmonary fibrosis. However, the late treatment (from Days 15 to 28) failed to attenuate it. The reason for lack of antifibrotic effects of imatinib in the late treatment is not clear. However, we clearly demonstrated that imatinib inhibited the proliferation of mesenchymal cells in vivo using Brdu-incorporation assay (Figure 5). In our model, the fibrotic lesions in the subpleura of the lung appear from Days 10 to 14 (Figure 6). Imatinib may effectively inhibit the growth of fibroblasts at the early fibrolic stage, whereas it is ineffective for the late stage in the pathogenesis of pulmonary fibrosis. On the other hand, this may be simply because the growth of lung fibroblasts is greatest early, and there is little proliferation later in our model.
More recently, Daniels and coworkers (30) reported that imatinib could also inhibit the activity of transforming growth factor β via inhibiting c-ABL kinase (30). They also demonstrated that imatinib prevented bleomycin-induced pulmonary fibrosis, whereas the mechanism involved in in vivo antifibrotic effects of imatinib is still unclear because the investigators examined no mechanistic study in a murinc model. Transforming growth factor β is known to be a critical growth factor that usually plays a role in the latter stage of fibrosis. Because imatinib did not show antifibrotic effects when administered in the late fibrotic stage (Figure 7), transforming growth factor β may not be mainly involved in the action of imatinib in vivo.
Imatinib has already been used as a therapeutic drug in clinics for many patients with chronic myeloid leukemia and gastrointestinal stromal tumors (5-8). Although it has been reported that the most frequent adverse effects related with imatinib in humans are nausea (40-55%), edema (35-75%), myalgia (20-45%), diarrhea (17-45%), and vomiting (13-41%), these adverse events were mild and moderate, indicating that long-term treatment with imatinib was generally well tolerated. On the basis of preliminary findings and the fact that imatinib is already in use for other disease states, it is a promising therapy that should be studied in clinical pulmonary fibrosis as well because we do not have a good therapy for IPF.
In summary, our preclinical study clearly demonstrated that imatinib inhibited the development of pulmonary fibrosis in bleomycin-treated mice. Recently, it has been reported that imatinib inhibited other fibrotic diseases such as myelofibrosis in chronic myeloid leukemia as well as in hypereosinophilic syndrome in humans (31, 32). Our results together with these reports provide in vivo evidence that imatinib may have therapeutic potential for the treatment of patients with fibrotic diseases, including pulmonary fibrosis, as an antifibrotic agent.
Conflict of Interest Statement: Y.A. does not have a financial relationship with a commercial entity that has an interest in the subject of this manuscript; Y.N. does not have a financial relationship with a commercial entity that has an interest in the subject of this manuscript; M.I. does not have a financial relationship with a commercial entity that has an interest in the subject of this manuscript; M.U. does not have a financial relationship with a commercial entity that has an interest in the subject of this manuscript; J.K. does not have a financial relationship with a commercial entity that has an interest in the subject of this manuscript; H.U. does not have a financial relationship with a commercial entity that has an interest in the subject of this manuscript; K.I. does not have a financial relationship with a commercial entity that has an interest in the subject of this manuscript; S.S. does not have a financial relationship with a commercial entity that has an interest in the subject of this manuscript.
Acknowledgment: The authors thank Dr. Yuka Matsumori for her technical assistance.
References
1. Gross TJ, Hunninghake GW. Idiopathic pulmonary fibrosis. N Engl J Med 2001;345:517-525.
2. Selman M, King TE Jr, Pardo A. Idiopathic pulmonary fibrosis: prevailing and evolving hypotheses about its pathogenesis and implications for therapy. Ann Intern Med 2001;134:136-151.
3. American Thoracic Society. Idiopathic pulmonary fibrosis: diagnosis and treatment. International consensus statement. Am J Respir Crit Care Med 2000;161:646-664.
4. Collard HR, King TE Jr. Demystifying idiopathic interstitial pneumonia. Arch Intern Med 2003;163:17-29.
5. Druker BJ, Talpaz M, Resta DJ, Peng B, Buchdunger E, Ford JM, Lydon NB, Kantarjian H, Capdeville R, Ohno-Jones S, et al. Efficacy and safety of a specific inhibitor of the BCR-ABL tyrosine kinase in chronic mycloid leukemia. N Engl J Med 2001;344:1031-1037.
6. Druker BJ, Sawyers CL, Kantarjian H, Resta DJ, Reese SF, Ford JM, Capdeville R, Talpaz M. Activity of a specific inhibitor of the BCR-ABL tyrosine kinase in the blast crisis of chronic myeloid leukemia and acute lymphoblastic leukemia with the Philadelphia chromosome. N Engl J Med 2001;344:1038-1042.
7. Demetri GD, von Mehren M, Blanke CD, Van den Abbeele AD, Eisenberg B, Roberts PJ, Heinrich MC, Tuveson DA, Singer S, Janicek M, et al. Efficacy and safety of imatinib mesylate in advanced gastrointestinal stromal tumors. N Engl J Med 2002;347:472-480.
8. van Oosterom AT, Judson I, Verweij J, Stroobants S, Donato di Paola E, Dimitrijevic S, Martens M, Webb A, Sciot R, Van Glabbeke M, et al. European Organisation for Research and Treatment of Cancer Soft Tissue and Bone Sarcoma Group. Safety and efficacy of imatinib (STI571) in mctastatic gastrointestinal stromal tumours: a phase I study. Lancet 2001;358:1421-1423.
9. Druker BJ, Tamura S, Buchdungcr E, Ohno S, Segal GM, Fanning S, Zimmermann J, Lydon NB. Effects of s selective inhibitor of the abl tyrosine kinase on the growth of bcr-abl positive cells. Nat Med 1996;2:561-566.
10. Heldin CH, Westermark B. Mechanism of action and in vivo role of platelet-derived growth factor. Physiol Rev 1999;79:1283-1316.
11. Li X, Eriksson U. Novel PDGF family members: PDGF-C and PDGF-D. Cytokine Growth Factor Rev 2003;14:91-98.
12. Maeda A, Hiyama K, Yamakido H, Ishioka S, Yamakido M. Increased expression of platelet-derived growth factor A and insulin-like growth factor-I in BAL cells during the development of bleomycin-induced pulmonary fibrosis in mice. Chest 1996;109:780-786.
13. Yoshida M, Sakuma J, Hayashi S, Abe K, Saito I, Harada S, Sakatani M, Yamamoto S, Matsumoto N, Kaneda Y. A histologically distinctive interstitial pneumonia induced by overexpression of the interleukin 6, transforming growth factor beta 1, or platelet-derived growth factor B gene. Proc Natl Acad Sci USA 1995;92:9570-9574.
14. Antoniades HN, Bravo MA, Avila RE, Galanopoulos T, Neville-Golden J, Maxwell M, Selman M. Platelet-derived growth factor in idiopathic pulmonary fibrosis. J Clin Invest 1990;86:1055-1064.
15. Homma S, Nagaoka I, Abe H, Takahashi K, Seyania K, Nukiwa T, Kira S. Localization of platelet-derived growth factor and insulin-like growth factor I in the fibrotic lung. Am J Respir Crit Care Med 1995;152:2084-2089.
16. Nishioka Y, Aono Y, Inayama M, Ugai M, Kishi J, Uehara H, Izumi K, Sone S. Imatinib as a novel PDGF receptor-targeted drug to prevent bleomycin-induced lung fibrosis [abstract]. J Jpn Respir Soc 2004;42:250A.
17. Aono Y, Nishioka Y, Uehara H, Izumi K, Sone S. Anti-fibrotic effects of STI571 (Gleevec) in bleomycin-induced pulmonary fibrosis [abstract]. Am J Respir Crit Care Med 2004;169:A776.
18. Nishioka Y, Yano S, Fujiki F, Mukaida N, Matsushima K, Tsuruo T, Sone S. Combined therapy of multidrug-resistant human lung cancer with anti-P-glycoprotein antibody and monocyte chemoattractant protein-1 gene transduction:the possibility of immunological overcoming of multidrug resistance. Int J Cancer 1997;71:170-177.
19. Harrison JH, Lazo JS. High dose continuous infusion of bleomycin in mice: a new model for drug-induced pulmonary fibrosis. J Pharmacol Exp Ther 1987;243:1185-1194.
20. Tokuda A, Itakura M, Onai N, Kimura H, Kuriyama T, Matsushima K. Pivotal role of CCR1-positive leukocytes in blcomycin-induced lung fibrosis in mice. J Immunol 2000;164:2745-2751.
21. Ashcroft T, Simpson JM, Timbrell V. Simple method of estimating severity of pulmonary fibrosis on a numerical scale. J Clin Pathol 1988;41:467-470.
22. Phan SH, Varani J, Smith D. Rat lung fibroblast collagen metabolism in bleomycin-induced pulmonary fibrosis. J Clin Invest 1985;76:241-247.
23. Mitani K, Nishioka Y, Yamabe K, Ogawa H, Miki T, Yanagawa H, Sone S. Soluble Fas in malignant pleural effusion and its expression in lung cancer cells. Cancer Sci 2003;94:302-307.
24. Greco A, Roccato E, Miranda C, Cleris L, Formelli F, Pierotti MA. Growth-inhibitory effects of STI571 on cells transformed by the COL1A1/PDGFB rearrangement. Int J Cancer 2001;92:354-360.
25. Yoshida M, Sakuma-Mochizuki J, Abe K, Arai T, Mori M, Goya S, Matsuoka H, Hayashi S, Kaneda Y, Kishimoto T. In vivo gene transfer of an extracellular domain of platelet-derived growth factor beta receptor by the HVJ-liposome method ameliorates blcomycin-induced pulmonary fibrosis. Biochem Biophys Res Commun 1999;265:503-508.
26. Rice AB, Moomaw CR, Morgan DL, Bonner JC. Specific inhibitors of platelet-derived growth factor or epidermal growth factor receptor lyrosine kinase reduce pulmonary fibrosis in rats. Am J Pathol 1999;55:213-221.
27. Yaekashiwa M, Nakayama S, Ohnuma K, Sakai T, Abe T, Satoh K, Matsumoto K, Nakamura T, Takahashi T, Nukiwa T. Simultaneous or delayed administration of hepatocyte growth factor equally represses the fibrotic changes in murine lung injury induced by bleomycin: a morphologic study. Am J Respir Crit Care Med 1997;156:1937-1944.
28. Nakao A, Fujii M, Matsumura R, Kumano K, Saito Y, Miyazono K, Iwamoto I. Transient gene transfer and expression of Smad7 prevents bleomycin-induced lung fibrosis in mice. J Clin Invest 1999;104:5-11.
29. Wang Q, Wang Y, Hyde DM, Gotwals PJ, Koteliansky VE, Ryan ST, Giri SN. Reduction of bleomycin induced lung fibrosis by transforming growth factor β soluble receptor in hamsters. Thorax 1999;54:805-812.
30. Daniels CE, Wilkes MC, Edens M, Kottom TJ, Murphy SJ, Limper AH, Leof EB. Imatinib mesylate inhibits the profibrogenic activity of TGF-β and prevents bleomycin-mediated lung fibrosis. J din Invest 2004;114:1308-1316.
31. Beham-Schmid C, Apfelbeck U, Sill H, Tsybrovsky O, Hofler G, Haas OA, Linkesch W. Treatment of chronic myelogenous leukemia with the tyrosinc kinase inhibitor ST1571 results in marked regression of bone marrow fibrosis. Blood 2002;99:381-383.
32. Klion AD, Robyn JA, Akin C, Noel P, Brown MR, Law MA, Metcalfe DD, Dunbar CE, Nutman TB. Molecular remission and reversal of myelofibrosis in response to imatinib mesylate treatment in patients with the myeloproliferative variant of hypereosinophilic syndrome. Blood 2003;103:473-478.
Yoshinori Aono, Yasuhiko Nishioka, Mami Inayama, Momoyo Ugai, Jun Kishi, Hisanori Uehara, Keisuke Izumi, and Saburo Sone
Departments of Internal Medicine and Molecular Therapeutics, and Molecular and Environmental Pathology, Course of Medical Oncology, University of Tokushima School of Medicine, Tokushima, Japan
(Received in original form April 23, 2004; accepted in final form February 16, 2005)
Supported by grants from the Ministry of Health and Welfare and the Ministry of Education, Science, Sports, and Culture of Japan.
Correspondence and requests for reprints should be addressed to Saburo Sone, M.D., Ph.D., Department of Internal Medicine and Molecular Therapeutics, Course of Medical Oncology, University of Tokushima School of Medicine, 3-18-15 Kuramotocho, Tokushima 770-8503, Japan. E-mail: ssone@clin.med.tokushima-u.ac.jp
This article has an online supplement, which is accessible from this issue's table of contents at www.atsjournals.org
Am J Respir Crit Care Med Vol 171. pp 1279-1285, 2005
Originally Published in Press as DOI: 10.1164/rccm.200404-531OC on February 25, 2005
Internet address: www.atsjournals.org
Copyright American Thoracic Society Jun 1, 2005
Provided by ProQuest Information and Learning Company. All rights Reserved