The cytotoxic agent bleomycin is feared for its induction of sometimes fatal pulmonary toxicity, also known as bleomycin-induced pneumonitis (BIP). The central event in the development of BIP is endothelial damage of the lung vasculature due to bleomycin-induced cytokines and free radicals. Ultimately, BIP can progress in lung fibrosis. The diagnosis is established by a combination of clinical symptoms, radiographic alterations, and pulmonary function test results, while other disorders resembling BIP have to be excluded. Pulmonary function assessments most suitable for detecting BIP are those reflecting lung volumes. The widely used transfer capacity of the lungs for carbon monoxide appeared recently not to be specific when bleomycin is used in a polychemotherapeutic regimen. There are no proven effective treatments for BIP in humans, although corticosteroids are widely applied. When patients survive BIP, they almost always recover completely with normalization of radiographic and pulmonary function abnormalities. This review focuses on BIP, especially on the pathogenesis, risk factors, and its detection. (CHEST 2001; 120:617-624)
Key words: bleomycin; pneumonitis; pulmonary toxicity
Abbreviations: BEP = bleomycin, etoposide, cisplatin; BIP = bleomycin-induced pneumonitis; BOOP = bronchiolitis obliterans with organizing pneumonia; EP = etoposide, cisplatin; G-CSF = granulocyte-colony stimulating factor; IL-interleukin; TGF = transforming growth factor; TLC = total lung capacity; TLCO = transfer capacity of the lungs for carbon monoxide; TNF = tumor necrosis factor; VC = vital capacity
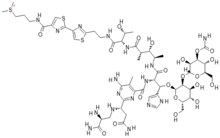
Bleomycin is an antibiotic agent with antitumor activity discovered by Umezewa et al[1] in 1966 and was originally isolated from the fungus Streptomyces verticillus. It is commonly used as part of the cytostatic treatment of several tumor types, such as germ-cell tumors, lymphomas, Kaposi's sarcoma, cervical cancer, and squamous cell carcinomas of head and neck.
Bleomycin exerts its antitumor effect by inducing tumor cell death, while inhibition of tumor angiogenesis may also be important.[2] Its cytotoxicity occurs by induction of free radicals. Bleomycin forms a complex with Fe (II), which is subsequently oxidized to Fe (III), resulting in reduction of oxygen to free radicals. These free radicals cause DNA breaks leading to cell death ultimately.[3-5] Bleomycin can be given by several routes: IV, IM, or subcutaneously; in case of malignant effusion, it can be administered intrapleurally or intraperitoneally. The elimination of bleomycin is mainly by the kidneys; in the first 24 h after its administration, approximately 60% of unchanged drug is excreted.[6] Furthermore, bleomycin can be deactivated by the enzyme bleomycin hydrolase, which can be found predominantly in the liver, spleen, bone marrow, and intestine.[7]
The application of bleomycin is featured by the occurrence of sometimes fatal side effects. Due to the lack of the bleomycin-inactivating enzyme, bleomycin hydrolase, in the lungs and the skin,[8] bleomycin-induced toxicity occurs predominantly in these organs. Directly after its administration, the occurrence of fever, chills, and sometimes hypotension is well known.[9,10] Other side effects are dermal hyper-pigmentation and fibrosis, stomatitis, and fatigue.[11] The most feared and dose-limiting side effect of bleomycin is its induction of pulmonary toxicity. Several distinct pulmonary syndromes have been associated with the use of bleomycin, such as bronchiolitis obliterans with organizing pneumonia (BOOP),[12] eosinophilic hypersensitivity,[13] and, most commonly, interstitial pneumonitis, which ultimately may progress into fibrosis. The latter, bleomycin-induced pneumonitis (BIP), occurs in 0 to 46% of the patients treated with bleomycin-containing chemotherapy, depending on the criteria used for the diagnosis.[14-18] The mortality of patients with BIP has been reported to be approximately 3% of all patients treated with bleomycin.[18,19] This review will focus on BIP, especially on its pathogenesis, risk factors, and the detection by pulmonary function assessments.
CLINICAL FEATURES
Often, BIP starts gradually during treatment, but the development of BIP up to 6 months after discontinuation of bleomycin therapy has also been reported.[20] The clinical diagnosis of BIP is rather hampered by its resemblance to other conditions often encountered in cancer patients, such as pneumonia, pulmonary metastases, or lymphangitic carcinoma.
Patients with BIP present initially with a nonproductive cough, exertional dyspnea, and sometimes fever. With progressive pneumonitis, dyspnea at rest, tachypnea, and cyanosis may occur. At physical examination, fine bibasilar crepitations can be found initially, progressing to rhonchi and sometimes pleural rubbing.[17]
Typical chest radiographic findings are bilateral, bibasilar infiltrates, sometimes followed by diffuse interstitial and alveolar infiltrates, and lobar consolidation ultimately. However, BIP can also present with unilateral abnormalities and focal infiltrates. 17,21
On CT scanning, bleomycin-induced alterations may appear earlier than on chest radiographs. In most patients, small linear and subpleural nodular lesions in the lung bases are noticed.[22]
Histologic material, for instance, obtained by transbronchial biopsies is often not conclusive. There are no real pathognomic alterations, but the most characteristic lesions are squamous metaplasia of bronchiolar epithelium, inflammatory cells infiltrating into alveoli and alveolar septa, edema plus focal collagen depositions in these septa, and fibrotic areas.[23,24]
Because of the resemblance of the symptoms of BIP with other diseases, the diagnosis of BIP is often one of exclusion. Other diseases are often excluded by culture and Gram-staining of sputum, polymerase chain reaction on pathogens such as viruses, or serology or determination of antigens of pathogens leading to a specific pneumonia. Often these patients have been treated unsuccessfully with antibiotics because of the suspicion of pneumonia before the diagnosis BIP is established. When patients survive the episode of BIP, they almost always recover completely with disappearance of symptoms, signs, and pulmonary function disturbances.[17,25]
PATHOGENESIS
The pathogenesis of BIP has been intensively studied in animals, but data derived from human studies are scarce. In animals, the first event noted is endothelial damage of the lung vasculature accompanied by edema.[26] This is followed by influx of inflammatory cells such as macrophages, lymphocytes, and neutrophils into the lung parenchyma and subsequently by fibroblasts leading to pulmonary fibrosis.[26] Studies in patients who developed clinically evident BIP showed that alterations in lung function assessments and chest radiography abnormalities are reversible in time,[17,25] suggesting that the pulmonary changes due to bleomycin can be reversible, probably before the process of fibrosis starts definitely.
The mechanism of the endothelial damage, the primary event in the development of BIP, is not exactly known, but evidence is mounting that the induction of cytokines and free radicals is involved. These cytokines and free radicals can damage endothelial cells. Furthermore, the induced cytokines activate lymphocytes and upregulate adhesion molecules on endothelial cells, enabling the adhesion of activated inflammatory cells to the endothelium, the first step required for influx of these cells into the interstitium.[27] The adhered lymphocytes also contribute to the endothelial damage by inducing apoptosis.[28,29] After bleomycin exposure, increased expression of Fas messenger RNA in pulmonary endothelial cells and upregulation of its ligand, FasL, on lymphocytes resulting in apoptosis of the endothelial cells have been described.[28] The progression of BIP could be prevented by pretreatment with soluble Fas antigen and anti-FasL-antibodies demonstrating the important role of this system.[29]
One of the primary sources of the cytokines involved in BIP is the macrophage. In vitro, bleomycin activates human alveolar macrophages that subsequently produce cytokines such as tumor necrosis factor (TNF)-[Alpha] and interleukin (IL)-1[Beta].[30] In animals, several studies[31-34] have shown significant increases in protein or messenger RNA of TNF-[Alpha] and IL-1[Beta] in lungs after systemic or intratracheal administration of bleomycin. In humans, TNF-[Alpha] is also induced by bleomycin. A significant rise in TNF-[Alpha] plasma levels has been described 3 h, 4.5 h, and 24 h after administration of bleomycin in testicular cancer patients.[35] Animal studies underlining the important role of these cytokines in the development of BIP showed that the development of BIP can be prevented by the administration of antibodies against TNF-[Alpha][34] or by IL-1--receptor antagonists.[36]
The free radicals that contribute to the endothelial damage[37] are produced by bleomycin directly after oxidation of the bleomycin-Fe (II) complex[3-5] and by activated polymorphonuclear leukocytes.[38] The importance of iron and free radicals in the pathogenesis of BIP is shown by prevention of BIP by dexrazoxane[39] or amifostine,[40] respectively.
After the damage of the endothelial cells and the subsequent infiltration of inflammatory cells into the interstitium, fibroblasts are activated with the accompanying deposit of collagen. These fibroblasts are activated by bleomycin directly[41] and indirectly by bleomycin-induced cytokines such as TNF-[Alpha].[42,43] In the process of collagen production by fibroblasts, transforming growth factor (TGF)-[Beta] is one of the central mediators, as has been shown by a study in animals[44] showing the prevention of BIP by antibodies against TGF-[Beta]. After administration of bleomycin to animals, TGF-[Beta] has been shown in several cell types in the lungs, such as in macrophages, fibroblasts, endothelial cells, and eosinophils.[45] Also, this TGF-[Beta] can be induced by bleomycin[46] as well as the other cytokines induced by bleomycin.[47]
PULMONARY FUNCTION ASSESSMENTS
Numerous methods such as cell counts in BAL fluid, gallium lung scanning, angiotensin-converting enzyme plasma levels, chest radiographs, or CT scans have been evaluated to detect BIP at an early stage, in order to avoid the further development of severe BIP by withholding further treatment with bleomycin.[16] Pulmonary function assessments, however, seem to be the most proper tool.
Comis et al[48] were the first to show a decrease in the transfer capacity of the lungs for carbon monoxide (TLCO) during bleomycin-containing multidrug chemotherapy. This observation was confirmed by several subsequent studies.[49-51] Based on the histologic changes observed in the lungs after bleomycin exposure in animals, this decline in TLCO was considered to be due to bleomycin alone. Several studies[48-50,52-54] have examined whether deterioration of TLCO was sensitive for detecting BIP and predictive for the development of clinical significant BIP. Although data from these studies are rather conflicting, several authors[48,55-58] advised stopping further treatment with bleomycin when TLCO decreases [is greater than] 40% or 60% of the pretreatment value.
Because bleomycin is almost always used in combination with other drugs that may also affect pulmonary function assessments, we previously performed a study to test the specificity of pulmonary function tests for bleomycin-induced pulmonary alterations.[59] Pulmonary function assessments were carried out in 54 patients with disseminated testicular cancer randomized to treatment with 360 mg of bleomycin, etoposide, and cisplatin (BEP) or with etoposide and cisplatin (EP) only. During treatment, a decline of TLCO was found in both groups, and only at the end of therapy the TLCO was significantly decreased in the BEP compared with the EP group.[59] It can be concluded that alterations in TLCO during bleomycin-containing multidrug chemotherapy are not a proper tool for monitoring BIP and, thus, cannot be used for decisions regarding further bleomycin treatment.
Two other pulmonary function tests, however, the vital capacity (VC) and the pulmonary capillary blood volume, showed decreased values only in the patients treated with BEP, while remaining stable in the EP patients.[59] Therefore, these two parameters are more specific for bleomycin-induced changes. The VC has been shown to decrease more in patients developing BIP.[50] Also, the total lung capacity (TLC), a parameter that, like the VC, reflects changes in lung volume, has been reported[49,60] to decrease significantly in patients developing BIP compared with those who did not.
Therefore, combined with clinical symptoms, lung function assessments reflecting lung volumes such as VC and TLC can be used for patients suspected of developing BIP. It has to be kept in mind, however, that there is no association between pulmonary symptoms and decline of lung function assessments.[57]
RISK FACTORS
Many studies have been performed to identify risk factors for the development of BIP. However, most of these studies have used different criteria for its diagnosis. Furthermore, for establishing BIP, many studies used lung function assessments that have been shown later not to be specific for BIP when bleomycin is used in a multidrug regimen. In these circumstances and by these lung function assessments, pulmonary toxicity of bleomycin cannot be distinguished from pulmonary effects of other agents used. Therefore, comparison between studies is severely hampered, while others are not suitable for the purpose for which they were designed. Only studies that use BIP-specific lung function assessments, clinical symptoms or signs, or postmortem data are suitable for identification of risk factors of BIP.
Some studies[61,62] suggest that the route by which bleomycin is administrated may affect bleomycin-induced toxicity. Bleomycin continuously infused may induce less toxicity than bolus injection.[61,62] Decreased toxicity has also been described for IM administration compared to the IV route. However, other studies[21,63] failed to show a relation between route of administration and toxicity. Therefore, bleomycin is mostly given IV in 30 to 60 min, enabling administration in an outpatient setting.
In animals, a linear positive relation between dose and severity of BIP has been found.[64,65] Several studies[11,66,67] suggested a similar relation in humans as well. For instance, in patients receiving a cumulative dose of [is less than] 300 mg of bleomyein, the incidence of BIP is 3 to 5%, while in patients treated with [is greater than] 500 mg, 20% of the patients develop BIP.[67] However, this dose-toxicity relationship in humans is less dear than it is in animals. Fatal BIP has been described in patients treated with [is less than] 100 mg of bleomyein, while in others receiving [is greater than] 500 mg, no pulmonary toxicity occurred.[68-70] Recently, Simpson et al[19] described 180 patients treated with bleomycin and they did not find a significant difference in the cumulative dose of bleomycin between patients who died of BIP and those who did not. However, because of the increased incidence of BIP in patients treated with high doses, it is generally recommended to keep the total dose of bleomycin [is less than] 400 mg.
Age of the patients is also an established risk factor for the development of BIP. Elderly patients have an increased susceptibility to develop BIP, especially those [is greater than] 70 years,[17,21] but BIP has been reported also in much younger patients. One study[19] described that the occurrence of fatal BIP increased with each decade after the age of 30 years. The exact reason for this increased risk is not known; it may be that decreased radical scavenging or a physiologic decline of renal function of elderly is involved.
Several studies[71,72] aimed to reveal whether a smoking history increased the risk for BIP. An increased risk in smokers is strongly suggested by the study by Lower et al.[72] These authors showed radiographic alterations consistent with BIP in 55% of the smoking patients receiving bleomycin compared with 0% of the nonsmokers.[72]
Bleomycin is mainly excreted by the kidneys, and deterioration of renal function has been shown to prolong bleomycin clearance. Crooke et al[6] showed that terminal elimination half-life of bleomycin is not increased until a creatinine clearance of 25 to 35 mL/min, suggesting increased risk of BIP only in case of severe renal dysfunction. However, the study by Hall et al[73] showed that bleomycin clearance is positively correlated with serum creatinine, suggesting enhanced bleomycin-induced effects in lesser degrees of renal dysfunction already. In accordance with this, many other studies[19,74,75] showed a relationship between decline of renal function and increased bleomycin lung effects. Because bleomycin is often combined with nephrotoxic agents such as cisplatin, special attention should be paid for the development of BIP in patients with prior or developing renal dysfunction during therapy.
Radiotherapy exerts its function by the induction of free radicals, and radiotherapy of the chest is feared for the development of pulmonary fibrosis. Theoretically, the combination of radiotherapy and bleomycin could be a synergistic one. However, the most recent studies[57,76] found only a slightly increased occurrence of pulmonary symptoms in patients treated with the combination compared to patients treated with bleomycin or radiotherapy alone. Pulmonary symptoms are most pronounced during therapy, while there is no evident increase of long-term sequelae. For instance, in patients with Hodgkin's disease, [is greater than or equal to] 3 years after treatment with mediastinal radiotherapy (median dose, 44 Gy) and bleomycin (median dose, 120 U/[m.sup.2]), 37% of the patients had a FVC of [is less than] 80% predicted compared with 32% and 19% of the patients treated, respectively, with mediastinal radiotherapy or bleomycin alone.[76] Hirsch et al[57] showed that in patients with Hodgkin's disease treated with bleomycin-containing multidrug therapy (median dose, 120 U/[m.sup.2]) followed by radiotherapy (median dose 36 Gy), a significantly higher percentage of patients developed pulmonary symptoms such as cough, shortness of breath, and oxygen requirement within 6 months after treatment compared with patients treated with chemotherapy only (50% vs 21%). However, 15 months after treatment there were no significant differences between both groups regarding pulmonary symptoms or functions.[57] It can be concluded that the combination of bleomycin-containing chemotherapy and radiation is not paralleled with an excess of toxicity, but that especially during treatment, physicians must be beware of the development of pulmonary toxicity.
Because bleomycin is assumed to induce its toxicity partially by the induction of free radicals, the administration of high inspired oxygen could be hazardous. In most studies[64,77,78] carried out in animals, such a relation has been shown. For instance, in hamsters treated with bleomycin and 70% oxygen for 72 h, the mortality was 90% compared with 15% in those animals that received bleomycin only.[64] In humans, clear data showing an increased risk of BIP with concomitant oxygen supplementation are lacking; however, because of the data obtained from animal studies, oxygen supplementation is discouraged during bleomycin treatment. Because it is also not clear whether prior bleomycin therapy increases pulmonary toxicity induced by the administration of oxygen during surgery, Donat and Levy[79] studied 77 patients with disseminated germ-cell tumors undergoing surgical resection for residual mass after bleomycin-containing chemotherapy (mean, 6.4 months). These authors did not show a significant difference in length and dose of administered fractional inspired oxygen between the 58 patients with no problems and the 19 patients with postoperative pulmonary problems, such as decreased oxygen saturation, pulmonary edema, or dyspnea, requiring treatment.[79]
Because of the important role of bleomycin-induced cytokines in the development of BIP, the increased application of growth factors in patients receiving chemotherapy could theoretically be paralleled by an increased incidence of BIP. These growth factors such as granulocyte-colony stimulating factor (G-CSF) can induce other cytokines involved in the pathogenesis of BIP. Although some case reports[80,81] suggested increased risk of BIP in patients treated with growth factors such as G-CSF, one study found no increase of BIP in 29 patients coadministered G-CSF and bleomycin-containing chemotherapy compared with 57 patients receiving bleomycin-containing therapy only.[60]
PREVENTION AND TREATMENT OF BIP
Probably one of the most efficient ways to prevent BIP is to lower the total cumulative dose of bleomycin. Therefore, several studies[18,82,83] have been performed in good-prognosis germ-cell cancer to establish the role of bleomycin; these studies showed that bleomycin could not be omitted completely from combination chemotherapy. However, Einhorn et al[84] showed that lowering the total dose of bleomycin from 360 to 270 mg does not reduce efficacy of the treatment of good-prognosis disseminated testicular cancer.[84] Therefore, 270 mg of bleomycin is considered to be the total dose in combination chemotherapy for disseminated good-prognosis germ-cell cancer in Europe as well as in the United States.[85,86]
In case of an unacceptable high risk for the development of BIP, physicians can consider treating patients with germ-cell cancer with etoposide, ifosfamide, and cisplatin instead of with the standard therapy, BEP. Etoposide, ifosfamide, and cisplatin have been shown to have an equal efficacy as BEP but at the costs of increased bone marrow suppression.[87,88]
The other malignancy for which bleomycin is often applied is Hodgkin's disease. The total cumulative dose of bleomycin is 120 mg/[m.sup.2] in many regimens. Although the main cause of pulmonary toxicity during treatment is the applied radiotherapy, in case of a high risk of BIP, nonbleomycin-containing regimens such as mechlorethamine, vincristine, procarbazine, and prednisone[89] or procarbazine, melphalan, and vinblastine[90] can be used.
In animals, several agents have been successfully tested for prevention or attenuation of BIP, such as soluble Fas antigen,[28] IL-1-receptor antagonists,[36] keratinocyte growth factor,[91] cyclosporin[92] or antibodies against TNF-[Alpha],[34] CD3 receptor,[93] Fas ligand,[29] or TGF-[Beta].[44] Also, dexrazoxane[39] and amifostine,[40] which both affect bleomycin-induced free radicals and which are already clinically applied for decreasing chemotherapy-induced toxicity, have been shown to be effective in animals. Drugs that turned out not to be capable of affecting BIP are enoxaparin,[94] pentoxifylline, and linomide.[95] Studies establishing agents that may prevent BIP in humans have, however, not been performed yet (to my knowledge).
When clinical BIP occurs, the most widely applied agents are corticosteroids in high dosages (prednisone, 60 to 100 mg/d). In animals, the data on the efficacy of corticosteroids for BIP are rather conflicting.[28,96] In humans, several case reports describe successful treatment of pulmonary symptoms during bleomycin treatment with corticosteroids. However, it might be possible that in several of these cases, the diagnosis was not BIP, but BOOP or eosinophilic hypersensitivity, both of which are known to react on treatment with corticosteroids. The study of White and Stover[20] suggests some effects of corticosteroids in the treatment of BIP. These authors describe 10 patients with clinically evident BIP, 7 of whom were treated with corticosteroids. Initially, all treated patients showed clinical and radiographic improvement, while lowering the dose of corticosteroids resulted in recurrence of symptoms in five of the seven patients. All three untreated patients died early, while three of seven of the treated patients died 12 to 15 months after the beginning of BIP.[20] However, besides this study, there are no other studies supporting the efficacy of corticosteroids in the treatment of BIP, while randomized studies are missing.
So, it can be concluded that when pulmonary symptoms start suddenly during bleomycin treatment and infections are excluded, the administration of corticosteroids is indicated because of a high risk of BOOP or eosinophilic hypersensitivity. For pulmonary symptoms starting more gradually and compatible with BIP, there are no convincing data for corticosteroids. In case of BIP, most important is that further bleomycin administration is withheld. When patients survive BIP, the pulmonary symptoms and disturbances in function assessment will almost always normalize in time.[17,25]
CONCLUSION
BIP is a severe and sometimes fatal side effect of bleomycin therapy. Numerous studies have been performed to identify methods capable of detecting BIP at an early preclinical stage. Combined with clinical signs and symptoms, pulmonary function tests reflecting lung volume such as TLC and VC are probably most suitable for this purpose. Identification of risk factors has probably resulted in decreased bleomycin-induced morbidity and mortality, but this has never been examined (to my knowledge). Increased knowledge of the pathogenesis may lead to agents capable of attenuating or preventing BIP, such as dexrazoxane, which may even permit higher bleomycin doses. Until that time, physicians administrating bleomycin have to be aware of the development of BIP, especially in the presence of risk factors (Table 1).
REFERENCES
[1] Umezawa H, Meaeda K, Takeuchi T, et al. New antibiotics, bleomycin A and B. J Antibiot Ser A 1966; 19:200-205
[2] Schirner M, Hoffmann J, Menrad A, et al. Antiangiogenic chemotherapeutic agents: characterization in comparison to their tumor growth inhibition in human renal cell carcinoma models. Clin Cancer Res 1998; 4:1331-1336
[3] Sausville EA, Peisach J, Horwitz SB. Effect of chelating agents and metal ions on the degradation of DNA by bleomycin. Biochem 1978; 17:2740-2746
[4] Sausville EA, Stein RW, Peisach J, et al. Properties and products of the degradation of DNA by bleomycin and iron. Biochemistry 1978; 17:2746-2754
[5] Burger RM, Pesach J, Horwitc SB. Activated bleomycin: a transient complex of drug, iron and oxygen that degradates DNA. J Biol Chem 1981; 256:11636-11644
[6] Crooke ST, Comis RL, Einhorn LH, et al. Effects of variations in renal function on the clinical pharmacology of bleomycin administrated as an iv bolus. Cancer Treat Rep 1977; 61:1631-1636
[7] Umezawa H, Takeiuechi T, Hosi S, et al. Studies on the mechanism of antitumor effect of bleomycin in squamous cell carcinoma. J Antibiot 1972; 25:409-420
[80] Ohnuma T, Holland JF, Masuda H, et al. Microbiological assay of bleomycin: inactivation, tissue distribution, and clearance. Cancer 1974; 33:1230-1238
[9] Rosenfelt F, Palmer J, Weinstein I, et al. A fatal hyperpyrexial response to bleomycin following prior therapy: a case report and literature review. Yale J Biol Med 1982; 55:529-531
[10] Leung WH, Lau JYN, Chan TK, et al. Fulminant hyperpurexia induced by bleomycin. Postgrad Med J 1989; 65:417-419
[11] Blum R, Carter SK, Agre K. A clinical review of bleomycin: a new antineoplastic agent. Cancer 1973; 31:903-914
[12] Santrach PJ, Askin FB, Wells RJ, et al. Nodular form of bleomycin-related pulmonary injury in patients with osteogenic sarcoma. Cancer 1989; 64:806-811
[13] Holoye PY, Luna MH, Mackay B, et al. Bleomycin hypersensitivity pneumonitis. Ann Intern Med 1978; 88:47-49
[14] Van Barneveld PWC, Van der Mark TW, Sleijfer DT, et al. Predictive factors for bleomycin-induced pneumonitis. Am Rev Respir Dis 1984; 130:1078-1081
[15] Dearnaley DP, Horwich A, A'Hern R, et al. Combination chemotherapy with bleomycin, etoposide and cisplatin (BEP) for metastatic testicular teratoma: long-term follow-up. Eur J Cancer 1981; 27:684-691
[16] Jules-Elysee K, White DA. Bleomycin-induced pulmonary toxicity. Clin Chest Med 1990; 11:1-20
[17] De Lena M, Guzzon A, Monfardini S, et al. Clinical, radiologic and histopathological studies on pulmonary toxicity induced by treatment with bleomycin (N.S.C.-125066). Cancer Chemother Rep 1972; 56:343-355
[18] Levi JA, Raghaven D, Harvey V, et al. The importance of bleomycin in combination chemotherapy for good-prognosis germ cell carcinoma. J Clin Oncol 1993; 11:1300-1305
[19] Simpson AB, Paul J, Graham J, et al. Fatal bleomycin pulmonary toxicity in the west of Scotland 1991-95; a review of patients with germ cell tumours. Br J Cancer1998; 78: 1061-1066
[20] White DA, Stover DE. Severe bleomycin-induced pneumonitis: clinical features and response to corticosteroids. Chest 1984; 86:723-728
[21] Yagoda A, Makherjib, Young C, et al. Bleomycin: an antitumor antibiotic; clinical experience in 274 patients. Ann Intern Med 1972; 77:861-870
[22] Rimmer MJ, Dixon AK, Flower CDR, et al. Bleomycin-lung: CT observations. Br J Radiol 1985; 58:1041-1045
[23] Jones AW. Bleomycin lung damage: the pathology and nature of the lesion. Br J Dis Chest 1978; 72:321-326
[24] Bedrossian LWM, Luna MA, Mackay B, et al. Ultrastructure of pulmonary bleomycin toxicity. Cancer 1973; 32:44-51
[25] Van Barneveld PWC, Sleijfer DT, Van der Mark TW, et al. The natural course of bleomycin induced pneumonitis (BIP): a follow-up study in eight patients. Am Rev Respir Dis 1987; 135:48-51
[26] Adamson IYR, Bowden DH. The pathogenesis of bleomycin-induced pulmonary fibrosis in mice. Am J Pathol 1974; 77:185-191
[27] Piguet PF, Rosen H, Vesin C, et al. Effective treatment of the pulmonary fibrosis elicited in mice by bleomycin or silica with anti-CD-11 antibodies. Am Rev Respir Dis 1993; 147:435-441
[28] Hagimoto N, Kuwano K, Nomoto Y, et al. Apoptosis and expression of Fas/Fas ligand mRNA in bleomycin-induced pulmonary fibrosis in mice. Am J Respir Cell Mol Biol 1997; 16:91-101
[29] Kuwano K, Hagimoto N, Kawasaki M, et al. Essential roles of the Fas/Fas ligand pathway in the development of pulmonary fibrosis. J Clin Invest 1999; 104:13-19
[30] Scheule RK, Perkins RC, Hamilton R, et al. Bleomycin stimulation of cytokine secretion by the human alveolar macrophage. Am J Physiol 1992; 262:L386-L391
[31] Phan SH, Kunkel SL. Lung cytokine production in bleomycin-induced pulmonary fibrosis. Exp Lung Res 1992; 18: 29-43
[32] Santana A, Saxena B, Noble NA, et al. Increased expression of transforming growth factor [Beta] isoforms ([Beta] 1, [Beta] 2, [Beta] 3) in bleomycin-induced pulmonary fibrosis. Am J Respir Cell Mol Biol 1995; 13:34-44
[33] Gurujeyalakshmi G, Giri SN. Molecular mechanisms of antifibrotic effect of interferon gamma in bleomycin-mouse model of lung fibrosis: downregulation of TGF-[Beta] and procollagen I and III gene expression. Exp Lung Res 1995; 21:791-808
[34] Piguet PF, Collart MA, Grau GE, et al. Tumor necrosis factor/cachectin plays a key role in bleomycin-induced pneumopathy and fibrosis. J Exp Med 1989; 170:655-663
[35] Sleijfer S, Vujaskovic Z, Limburg PC, et al. Induction of tumor necrosis factor-[Alpha] as a cause of bleomycin-related toxicity. Cancer 1998; 4:970-974
[36] Piguet PF, Vesin C, Grau GE, et al. Interleukin 1 receptor antagonist (IL1-ra) prevents or cures pulmonary fibrosis elicited in mice by bleomycin or silica. Cytokine 1993; 5:57-61
[37] Doelman CJA, Bast A. Oxygen radicals in lung pathology. Free Radio Biol Med 1990; 9:381-400
[38] Moseley PL, Shasby DM, Brady M, et al. Lung parenchymal injury induced by bleomycin. Am Rev Respir Dis 1984; 130:1082-1086
[39] Herman EH, Hasinoff BB, Zhang J, et al. Morphologic and morphometric evaluation of the effect of ICRF-187 on bleomycin-induced pulmonary toxicity. Toxicology 1995; 98: 163-175
[40] Nici L, Calabresi P. Amifostine modulation of bleomycin-induced lung injury in rodents. Semin Oncol 1999; 26:28-33
[41] Moseley PL, Hemken C, Hunninghake GW. Augmentation of fibroblast proliferation by bleomycin. J Clin Invest 1986; 78:1150-1154
[42] Sugerman BJ, Aggarwal BB, Figari IS, et al. Recombinant human tumor necrosis factor [Alpha]: effects on proliferation of normal and transformed cells in vitro. Science 1985; 230:943-945
[43] Schmidt JA, Mizel SB, Cohen D, et al. Interleukin-1: a potential regulator of fibroblast proliferation. J Immunol 1982; 128:2177-2182
[44] Giri SN, Hyde DM, Hollinger MA. Effect of antibody to transforming growth factor [Beta] on bleomycin induced accumulation of lung collagen in mice. Thorax 1993; 48:959-966
[45] Zhang K, Flanders KC, Phan SH. Cellular localization of transforming growth factor-[Beta] expression in bleomycin-induced pulmonary fibrosis. Am J Pathol 1995; 147:352-361
[46] Phan SH, Gharaee-Kermani M, Wolber F, et al. Stimulation of rat endothelial cell transforming growth factor-[Beta] production by bleomycin. J Clin Invest 1991; 87:148-154
[47] Phan SH, Gharaee-Kermani M, McGarry B, et al. Regulation of rat pulmonary artery endothelial cell transforming growth factor-[Beta] production by IL-1-[Beta] and tumor necrosis factor-[Alpha]. J Immunol 1992; 149:103-106
[48] Comis RL, Kuppinger MS, Ginsberg SJ, et al. Role of single-breath carbon monoxide diffusing capacity in monitoring the pulmonary effects of bleomycin in germ cell tumor patients. Cancer Res 1979; 39:5076-5080
[49] Wolkowicz J, Sturgeon J, Ravji M, et al. Bleomycin-induced pulmonary function abnormalities. Chest 1992; 101:97-101
[50] Van Barneveld PWC, Veenstra G, Sleijfer DT, et al. Changes in pulmonary functions during and after bleomycin treatment in patients with testicular carcinoma. Cancer Chemother Pharmacol 1985; 14:168-171
[51] Luursema PB, Star-Kroesen MA, Van der Mark TW, et al. Bleomycin-induced changes in the carbon monoxide transfer factor of the lung and its components. Am Rev Respir Dis 1983; 128:880-883
[52] Sorensen PG, Rossing N, Roth M. Carbon monoxide diffusing capacity: a reliable indicator of bleomycin-induced pulmonary toxicity. Eur J Respir Dis 1985; 66:333-340
[53] Lucraft HH, Wilkinson PM, Stretton TB, et al. Role of pulmonary function tests in the prevention of bleomycin pulmonary toxicity during chemotherapy for metastatic testicular teratoma. Eur J Cancer Clin Oncol 1982; 18:133-139
[54] McKeage MJ, Evans BD, Atkinson C, et al. Carbon monoxide diffusing capacity is a poor predictor of clinically significant bleomycin lung. J Clin Oncol 1990; 8:779-783
[55] Comis RL. Detecting bleomycin pulmonary toxicity: a continued conundrum. J Clin Oncol 1990; 8:765-767
[56] Comis RL. Bleomycin pulmonary toxicity: current status and future directions. Semin Oncol 1992; 19(suppl 5):64-70
[57] Hirsch A, Vander Els N, Straus DJ, et al. Effect of ABVD chemotherapy with and without mantle or mediastinal irradiation on pulmonary function and symptoms in early-stage Hodgkin's disease. J Clin Oncol 1996; 14:1297-1305
[58] Jensen JL, Goel R, Venner PM. The effect of corticosteroid administration on bleomycin lung toxicity. Cancer 1990; 65:1291-1297
[59] Sleijfer S, Van der Mark TW, Schraffordt Koops H, et al. Decrease in pulmonary function during bleomycin-containing combination chemotherapy for testicular cancer: not only a bleomycin effect. Br J Cancer 1995; 71:120-123
[60] Saxman SB, Nichols CR, Einhorn LH. Pulmonary toxicity in patients with advanced-stage germ cell tumors receiving bleomycin with and without granulocyte colony stimulating growth factor. Chest 1997; 111:657-660
[61] Cooper KR, Hong WK. Prospective study of the pulmonary toxicity of continuously infused bleomycin. Cancer Treat Rep 1981; 65:419-425
[62] Carlson RW, Sikic BJ. Continuous infusion or bolus injection in cancer chemotherapy. Ann Intern Med 1983; 99:823-833
[63] Samuals MI, Johnson PE, Holoye PY, et al. Large-dose bleomycin therapy and pulmonary toxicity. JAMA 1976; 235:1117-1120
[64] Tryka AF, Skornik WA, Godleski JJ, et al. Potentiation of bleomycin-induced lung injury by exposure to 70% oxygen. Am Rev Respir Dis 1982; 126:1074-1076
[65] Catravas LD, Laza JS, Dobuler KJ, et al. Pulmonary endothelial dysfunction in the presence or absence of interstitial injury induced by intratracheally injected bleomycin in rabbits. Am Rev Respir Dis 1983; 128:740-746
[66] Haas CD, Coltman CA, Gottlieb JA, et al. Phase II evaluation of bleomycin: a southwest oncology group study. Cancer 1976; 38:8-12
[67] Collis CH. Lung damage of cytotoxic drugs. Cancer Chemother Pharmacol 1980; 4:17-27
[68] Bauer KA, Skarin AT, Balikian JP, et al. Pulmonary complications associated with combination chemotherapy programs containing bleomycin. Am J Med 1983; 74:557-563
[69] Wilson KS, Worth SA, Richards AG, et al. Low-dose bleomycin lung. Med Pediatr Oncol 1982; 10:283-288
[70] McLeod BF, Lawrance HJ, Smith DW, et al. Fatal bleomycin toxicity from a low cumulative dose in a patient with renal insufficiency. Cancer 1987; 60:2617-2622
[71] Parvinen LM, Kilkku P, Markinen E, et al. Factors affecting the pulmonary toxicity of bleomycin. Acta Radiol 1983; 22:417-422
[72] Lower EE, Strohofer S, Baughman RP. Bleomycin causes alveolar macrophages from cigarette smokers to release hydrogen peroxide. Am J Med Sci 1988; 295:193-197
[73] Hall SW, Strong JE, Broughton A, et al. Bleomycin clinical pharmacology by radioimmunoassay. Cancer Chemother Pharmacol 1982; 9:22-25
[74] Sleijfer S, Van der Mark TW, Schraffordt Koops H, et al. Enhanced effects of bleomycin on pulmonary function assessments in patients with decreased renal function due to cisplatin. Eur J Cancer 1996; 32A:550-552
[75] Dalgleish AG, Woods RL, Levi JA. Bleomycin pulmonary toxicity: its relationship to renal dysfunction. Med Pediatr Oncol 1984; 12:313-317
[76] Horning SJ, Adhikari A, Rizk N, et al. Effect of treatment for Hodgkin's disease on pulmonary function: results of a prospective study. J Clin Oncol 1994; 12:297-305
[77] Sogal RN, Gottlieb AA, Boutros AR, et al. Effect of oxygen on bleomycin-induced lung damage. Cleve Clin J Med 1987; 54:503-509
[78] Blom-Muilwijk MC, Vriesendorp R, Veninga TS, et al. Pulmonary toxicity after treatment with bleomycin alone or in combination with hyperoxia. Br J Anaesth 1988; 60:91-97
[79] Donat SM, Levy DA. Bleomycin associated pulmonary toxicity: is perioperative oxygen restriction necessary? J Urol 1998; 160:1347-1352
[80] Dirix L, Schrijvers D, Drawe P, et al. Pulmonary toxicity and bleomycin [letter]. Lancet 1997; 344:56
[81] Matthews J. Pulmonary toxicity of ABVD chemotherapy and G-CSF in Hodgkin's disease: possible synergy. Lancet 1993; 342:988
[82] Loehrer PJ, Johnson D, Elson P, et al. Importance of bleomycin in favorable-prognosis disseminated germ-cell tumors: an Eastern Co-operative Oncology Group trial. J Clin Oncol 1995; 13:470-476
[83] De Wit R, Stoter G, Kaye SB, et al. Importance of bleomycin in combination chemotherapy for good-prognosis testicular non-seminoma: a randomised study of the EORTC genito-urinary tract cancer co-operative group. J Clin Oncol 1997; 15:1837-1843
[84] Einhorn LH, Williams SD, Loehrer PJ, et al. Evaluation of optimal duration of chemotherapy in favorable-prognosis disseminated germ-cell tumors: a Southeastern Cancer Study Group protocol. J Clin Oncol 1989; 7:387-391
[85] De Wit R. Treatment of disseminated non-seminomatous testicular cancer: the European experience. Semin Surg Oncol 1999; 17:250-256
[86] Bosl GJ. Germ cell tumor clinical trials in North America. Semin Surg Oncol 1999; 17:257-262
[87] Nichols CR, Catalano PJ, Crawford ED, et al. Randomised comparison of cisplatin and etoposide and either bleomycin or ifosfamide in treatment of advanced disseminated germ-cell tumors: an Eastern Cooperative Oncology Group, Southwest Oncology Group, and Cancer and Leukemia Group study. J Clin Oncol 1998; 16:1287-1293
[88] De Wit R, Stoter G, Sleijfer DT, et al. Four cycles of BEP vs. four cycles of VIP in patients with intermediate-prognosis metastatic non-seminoma: a randomised study of the EORTC Genitourinary Tract Cancer Cooperative Group. Br J Cancer 1998; 78:828-832
[89] Canellos G, Anderson J, Propert K. Chemotherapy of advanced Hodgkin's disease with MOPP, ABVD, or MOPP alternating with ABVD. N Engl J Med 1992; 327:1478-1484
[90] Horning SJ, Ang PT, Hoppe RT, et al. The Stanford experience with combined procarbazine, alkeran and vinblastine (PAVe) and radiotherapy for locally extensive and advanced stage Hodgkin's disease. Ann Oncol 1992; 3:747-754
[91] Sugahara K, Iyama K, Kuroda MJ, et al. Double intratracheal installation of keratinocyte growth factor prevents bleomycin-induced lung fibrosis in rats. J Pathol 1998; 186:90-98
[92] Lossos IS, Or R, Goldstein RH, et al. Amelioration of bleomycin-induced pulmonary injury by cyclosporin A. Exp Lung Res 1996; 22:337-349
[93] Sharma SK, MacLean JA, Pinto C, et al. The effect of an anti-CD3 monoclonal antibody on bleomycin induced lymphokine production and lung injury. Am J Respir Dis 1996; 154:193-200
[94] Laxer U, Lossos IS, Gillis S, et al. The effect of enoxaparin on bleomycin-induced lung injury in mice. Exp Lung Res 1999; 25:531-541
[95] Kremer S, Breuer R, Lossos IS, et al. Effect of immunomodulators on bleomycin-induced lung injury. Respiration 1999; 66:455-462
[96] Nettelbladt O, Tengblad A, Hallgren R. High-dose corticosteroids during bleomycin-induced alveolitis in the rat do not suppress the accumulation of hyaluronan (hyaluronic acid) in lung tissue. Eur Respir J 1990; 3:421-428
(*) From the Department of Internal Medicine Sint Franciscus Gasthuis, Rotterdam, The Netherlands.
Manuscript received July 31, 2000; revision accepted January 23, 2001.
Correspondence to: Stefan Sleijfer, MD, PhD, Department of Internal Medicine, Sint Franciscus Gasthuis, Kleiweg 500, 3045 PM Rotterdam, The Netherlands; e-mail: sleijfer@hotmail.com
COPYRIGHT 2001 American College of Chest Physicians
COPYRIGHT 2001 Gale Group