The prognosis remains poor for patients with congestive heart failure (CHF), despite reduced mortality rates resulting from the addition of angiotensin converting enzyme inhibitors to traditional treatment regimens. Because much of the myocardial damage that occurs in patients with CHF may be related to sympathetic activation, interest in the use of beta blockers has grown. Recent studies have shown the benefits of beta blocker therapy in many patients with heart failure. Carvedilol, the first beta blocker labeled in the United States specifically for the treatment of heart failure, has been shown to improve left ventricular ejection fraction and may reduce mortality.
The prognosis remains poor for many patients with congestive heart failure (CHF) despite the addition of angiotensin converting enzyme (ACE) inhibitors to the traditional medical therapy of diuretics and digitalis.[1-4] Even with the addition of ACE inhibitors, the overall one-year mortality rate remains at 10 percent in patients with mild or moderate heart failure; at 26 percent in patients with New York Heart Association (NYHA) functional class III impairment; and at 42 percent in patients with NYHA functional class IV impairment (Table 1). Moreover, patients with CHF tend to experience progressive declines in exercise tolerance and functional ability.[1] Thus, there is a need for new therapies that will improve symptoms and survival rates in patients with CHF.
Use of Beta Blockers
CHF is a progressive syndrome resulting from the heart's inability to adequately perfuse and oxygenate peripheral tissues. This syndrome is manifested by symptoms of fatigue, dyspnea and congestion.[1,5] Chronic heart failure is associated with worsening ventricular dysfunction and pathologic ventricular remodeling, resulting in adverse hemodynamic changes.[6] It is not surprising, therefore, that physicians have chosen therapies aimed primarily at reversing these changes. Physicians treating patients with heart failure have traditionally selected agents with positive inotropic or peripheral vasodilatory effects and have avoided agents such as beta blockers, which exert negative inotropic effects.[7] Until recently, beta blockers were contraindicated in the treatment of CHF, largely because heart failure was viewed primarily as a hemodynamic disorder.[7-9]
It has become increasingly apparent that the view of heart failure as primarily a hemodynamic disorder is incomplete. Although drugs with positive inotropic effects can produce short-term symptomatic improvements in patients with heart failure,[10,11] their long-term use does not prolong life. In fact, some positive inotropic agents, such as beta agonists (e.g., dobutamine [Dobutrex]) and phosphodiesterase inhibitors (e.g., milrinone [Primacor]), have actually been shown to decrease survival rates.[7,10,11]
In addition to the familiar hemodynamic changes, heart failure also results in widespread neurohumoral activation. Aortic and ventricular baroreceptors are reset to permit less sympathetic inhibition, ultimately resulting in increased adrenergic tone. Decreased glomerular flow also activates the reninangiotensin system. Both of these systems-adrenergic and renin-angiotensin--activate each other.
Initially, these neurohumoral changes are compensatory, functioning to retain fluid and maintain cardiac output. Unfortunately, with prolonged activation, such neurohumoral changes have detrimental effects on the heart[2,12] The benefits of ACE inhibitors on disease progression are well documented, and survival in patients with heart failure is believed to be due in large part to the effects of these drugs on the neurohumoral changes of CHEF.[13-15]
Activation of the sympathetic nervous system has been described as "one of the cardinal pathophysiologic abnormalities in patients with congestive heart failure"[16] and as "one of the most important mechanisms that may be responsible for progression of heart failure."[17] Catecholamine levels are known to increase in proportion to the severity of symptoms in patients with heart failure. Patients with the highest levels of norepinephrine have the least favorable prognosis.[18,19 ]In animal models, interference with the actions of norepinephrine has been shown to retard the progression of heart failure.[12,16]
Moreover, because the sympathetic nervous system is the principal neurohumoral system activated in patients with mild symptoms of heart failure, the use of medications such as beta blockers, which inhibit sympathetic activity, might reduce the risk of disease progression in patients with mildly symptomatic heart failure.[17]
Recent controlled studies of patients with heart failure who received beta blockers have indeed shown that, with long-term use, these agents can improve left ventricular function[20-22] and symptoms of CHF.[20,23] Results of the Metoprolol in Dilated Cardiomyopathy (MDC) trial,[20] which included 383 patients with ejection fractions of less than 40 percent, showed that patients treated with metoprolol had improved exercise time, decreased left ventricular filling pressures and a reduced need for heart transplantation.
In addition, results of the Cardiac Insufficiency Bisoprolol Study (CIBIS)[23] demonstrated a significant reduction in hospital readmissions due to worsening CHF among patients treated with this beta blocker. However, neither the MDC trial nor the CIBIS study were able to demonstrate reductions in overall mortality.[20,23]
Carvedilol (Coreg) is the first beta blocker labeled in the United States specifically for the treatment of mild to moderate (NYHA class II or III) heart failure of ischemic or cardiomyopathic origin. The benefits of using carvedilol in patients with CHF have been demonstrated in both single-center[24-26] and multicenter[2,16,17,27] trials. The Australia-New Zealand Research Collaborative Group[28] studied 415 patients with stable heart failure of ischemic origin and found that treatment with carvedilol improved left ventricular function and decreased the risk of the combined end points of death or hospitalization over a 19-month period. However, the use of carvedilol was not shown to significantly reduce either mortality or hospitalization.[28]
The U.S. Carvedilol Study Group[16] enrolled 1,094 patients with chronic heart failure who were stratified into one of four groups on the basis of their performance on a six-minute walking test. This study was terminated early after researchers concluded that treatment with carvedilol resulted in a 65 percent relative reduction in the mortality rate among patients with heart failure. Although this conclusion has been challenged,[11,29,30] even critics of this study have acknowledged that the results of carvedilol trials are "promising."[11] Thus, findings to date suggest that carvedilol, and quite possibly other beta blockers, may not only improve left ventricular ejection fraction in patients with heart failure, but also reduce their risk of hospitalization and death.
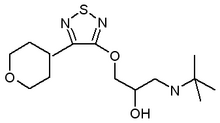
Pharmacology
Carvedilol is a nonselective beta-adreno-receptor antagonist and an [alpha.sub.1]-adreno-receptor antagonist. It has no intrinsic sympathomimetic activity.[31] Like many other classes of medications, beta blockers can be divided into three distinct groups. The first group consists of nonselective beta blockers without ancillary properties and includes such drugs as propranolol (Inderal) and timolol maleate (Blocadren).
The second group consists of selective blockers of beta receptor subtypes without ancillary properties. This group includes metoprolol (Lopressor) and atenolol (Tenorrain). The third group consists of nonselective beta blockers that have the ancillary property of vasodilation. Included in this group are labetalol (Normodyne), carvedilol and bucindolol (currently in phase 3 trials). Bucindolol and carvedilol produce less "inverse agonism" than most other beta blockers. Inverse agonism is the ability of a beta blocker to inactivate active state receptors. The beta blockers with the most inverse agonism, like propranolol, produce the greatest negative chronotropic and inotropic effects. Thus, bucindolol and carvedilol produce relatively fewer negative chronotropic and inotropic effects when compared with beta blockers like propranolol.[6]
The beta-blocking actions of carvedilol are generally evident in humans within one hour of administration, and the alpha-mediated vasodilatory effects, manifested by decreased peripheral resistance and decreased blood pressure, are evident within about 30 minutes of administration. The clinical significance of alpha blockade in conjunction with beta blockade in the treatment of CHF is not known. The use of alpha blockers alone, however, does not appear to reduce mortality in patients with symptomatic CHE.[32]
At high dosages, carvedilol exerts calcium channel blocking activity.[33] It also has significant antioxidant properties.[34,35] Carvedilol inhibits the generation of oxygen free radicals and prevents low-density lipoprotein (LDL) oxidation, which, in turn, reduces the uptake of LDL into the coronary vasculature. This antioxidant activity may contribute to carvedilol's cardioprotective effects.[36] In fact, compared with captopril, carvedilol has demonstrated similarly favorable effects on the lipid profiles of hypertensive patients with dyslipidemia.[37]
Carvedilol is rapidly absorbed following oral administration, achieving peak plasma concentrations within one to two hours. The apparent mean terminal elimination half-life of carvedilol generally ranges from seven to 10 hours. The rate of absorption is delayed by taking carvedilol with food. Carvedilol is metabolized by the liver and undergoes extensive first-pass metabolism. Three active metabolites of carvedilol have been identified, but none of these compounds appears to contribute to carvedilol's beta-blocking activity. Carvedilol is primarily metabolized by the liver, with less than 2 percent of a given dose excreted unchanged in the urine. Plasma concentrations of carvedilol are nevertheless increased in patients with renal failure. Carvedilol is highly bound to plasma proteins and is, therefore, not cleared significantly by hemodialysis.[13,31]
Precautions and Contraindications
Carvedilol is contraindicated in patients with bronchial asthma or related bronchospastic conditions, decompensated NYHA functional class IV heart failure requiring intravenous inotropic therapy, severe liver impairment, second- or third-degree atrioventricular block, sick sinus syndrome (unless a permanent pacemaker is in place), cardiogenic shock, severe bradycardia or known hypersensitivity to the drug.
Although carvedilol has not been demonstrated to have adverse effects on lipids, beta blockers without intrinsic sympathomimetic activity can worsen lipid profiles. Family physicians should, therefore, pay careful attention to lipid levels in patients with hyperlipidemia who are treated with carvedilol. Parameters of glycemic control should also be monitored. Patients with diabetes or thyroid disease should be warned that carvedilol, like other beta blockers, can mask the signs and symptoms of hypoglycemia and hyperthyroidism, including tachycardia. Moreover, nonselective beta blockers, like carvedilol, can potentiate insulin-induced hypoglycemia. Carvedilol should be used with caution in patients with peripheral vascular disease because beta blockers can precipitate or aggravate symptoms of arterial insufficiency.
Finally, carvedilol therapy should be avoided in patients with known hepatic impairment, since mild hepatocellular injury has occurred, although rarely, among patients treated with the drug.[13,31,38]
Adverse Reactions
Carvedilol is generally well-tolerated. In clinical trials comparing carvedilol monotherapy with placebo, 4.9 percent of patients treated with less than 50 mg of carvedilol and 5.2 percent of patients taking placebo discontinued use because of adverse effects. Discontinuation of therapy because of postural hypotension was more common among patients treated with carvedilol (1 percent versus zero percent).[31] Dizziness, hypotension and fatigue were the most frequently reported adverse effects[13,16,31] Less common adverse effects included diarrhea (2.2 percent in patients taking carvedilol versus 1.3 percent in patients taking placebo), bradycardia (2.1 percent versus 0.2 percent), edema (1.4 percent versus 0.4 percent), insomnia (1.6 percent versus 0.6 percent), dyspnea (1.4 percent versus 0.9 percent), pharyngitis (1.5 percent versus 0.6 percent) and urinary tract infections (1.8 percent versus 0.6 percent).[31] Rare reports of liver function abnormalities have been noted; however, no deaths have been reported, and the mild hepatic injury appears to have been reversed once the drug was discontinued. Rare cases of thrombocytopenia have also been reported.[13,31,38]
Much of the initial study of carvedilol's tolerability did not include patients with heart failure. Nevertheless, the U.S. Carvedilol Heart Failure Study Group[16] also found that dizziness and fatigue were the most common adverse reactions reported by patients treated with carvedilol. They also noted increased reports of dyspnea (25 percent with carvedilol versus 22 percent with placebo), heart failure (21 percent versus 16 percent) and cough (10 percent versus 8 percent). The Australia-New Zealand Heart Failure Research Collaborative Group[2] reported the following as the most frequent reasons for withdrawal from treatment during the double-blind phase of their study: worsening heart failure (5 percent in patients taking carvedilol versus 2 percent in patients taking placebo), dizziness/hypotension (3 percent versus zero percent), bradycardia/heart block (3 percent versus zero percent), headache, tiredness, irritability and worsening control over diabetes (1 percent versus zero percent).
Drug Interactions
Because of carvedilors extensive oxidative liver metabolism, its pharmacokinetics can be profoundly affected by certain drugs that significantly induce or inhibit oxidation. Rifampin (Rifadin), an inducer of hepatic metabolism, can reduce plasma concentrations of carvedilol by 70 percent when these drugs are coadministered. In contrast, cimetidine (Tagamet), an inhibitor of the cytochrome [P.sub.450] 2D6 isoenzyme (the same isoenzyme involved in the metabolism of carvedilol), can increase carvedilol's plasma concentration by 30 percent. Other inhibitors of the cytochrome [P.sub.450] 2D6 isoenzyme, such as quinidine, fluoxetine (Prozac), paroxetine (Paxil) and propafenone (Rythmol), could be expected to have similar effects on carvedilol's plasma concentrations.[13,31]
Digoxin (Lanoxin) concentrations increase by approximately 15 percent in patients also taking carvedilol. Consequently, digoxin levels should be closely monitored when initiating, adjusting or discontinuing carvedilol therapy. As with other beta blockers, combining carvedilol with verapamil (Calan) or diltiazem (Cardizem) should be done with caution. When these agents are combined, it is recommended that blood pressure and electrocardiographic changes be closely monitored. Coadministration of beta blockers and catecholamine-depleting drugs, such as reserpine (Serpasil) or monoamine oxidase (MAO) inhibitors can result in severe hypotension. These agents should be combined with great caution, and patients taking these drugs should be closely monitored. Similarly, coadministration of carvedilol and clonidine (Catapres) should be undertaken carefully because beta blockers can potentiate blood pressure and heart rate reductions in such patients. When clonidine therapy is discontinued, it is recommended that the beta blocker be discontinued first. Then, after several days, clonidine can be gradually tapered and discontinued in the hope of avoiding reflex tachycardia and hypertensive crisis.[13,31] Drugs that interact with carvedilol are listed in Table 2.[31]
Dosing and Administration
Carvedilol is indicated for the treatment of heart failure in patients with clinically stable NYHA functional class II or III heart failure. Patients taking diuretics, digitalis or ACE inhibitors should be taking stable dosages of these medications before carvedilol therapy is initiated. Carvedilol may also be used in patients unable to tolerate an ACE inhibitor and in those not taking digoxin, hydralazine (Apresoline) or nitrate therapy. In most cases, however, ACE inhibitor therapy should be initiated and stabilized before the introduction of carvedilol therapy. Finally, it is important to remember that, initially, beta-blocker therapy causes negative inotropic and chronotropic effects while the improvements in left ventricular function develop over time. Therefore, patients hospitalized for heart failure, those in a fluid-overload state and those who are symptomatically hypotensive should not be given carvedilol.[6,13,38]
The starting dosage of carvedilol is 3.125 mg orally twice daily for two weeks. This dosage is the same regardless of the patient's age or weight. Because food slows the rate (but not the extent) of absorption, carvedilol should be taken with food to reduce the incidence of orthostatic hypotension. Patients should be observed in the physician's office for adverse reactions, especially dizziness, lightheadedness and hypotension, for one hour after the first dose and again after each dosage increase. Blood pressure should be measured with the patient standing. Patients should be instructed to weigh themselves every day and to contact their physician immediately if they experience a weight gain of 0.91 to 1.36 kg (2 to 3 lb) above their usual "dry" weight. If, after two weeks, the initial dosage of carvedilol has been well-tolerated, it should be doubled. The dosage should be doubled every two weeks to the maximum dosage or the highest tolerated dosage. The maximum recommended dosage for carvedilol is 25 mg twice daily in patients weighing less than 85 kg (187 lb) and 50 mg twice daily in patients weighing 85 kg (187 lb) or more.[6,13,36] Recommendations for the administration and titration of carvedilol are summarized in Tables 3 and 4.
TABLE 3 Administration of Carvedilol (Coreg) in Patients with Congestive Heart Failure
Starting dosage
3.125 mg taken twice daily for two weeks. This dosage is the same regardless of the age or weight of the patient. Carvedilol should be taken with food. Patient should be observed in the office for one hour after initial dose is given.
Titration
If previous dosage was well-tolerated, dosage should be doubled every two weeks to the maximum dosage or the highest tolerated dosage. Patient should be observed in the office for one hour after every dosage adjustment.
Maximum dosage
Patients weighing [is less than] 85 kg (187 lb):. 25 mg twice daily Patients weighing [is greater than] 85 kg (187 lb): 50 mg twice daily
Monitoring
Patient should be weighed daily. Any weight gain of 0.91 to 1.36 kg (2 to 3 lb) should be reported to the physician. Blood presslute measurements should be taken with the patient standing. Parameters of glycemic and lipid control should be monitored, and medicines should be adjusted appropriately.
Indication
Clinically stable NYHA functional class II or class III heart failure. Therapy with ACE inhibitors should be initiated and stabilized before the introduction of carvedilol therapy. Patients should not be in the hospital for heart failure or in a fluid-overload state.
Contraindications
Bronchial asthma or related bronchospastic conditions; decompensated NYHA functional class IV heart failure requiring intravenous inotropic therapy; should not be used in patients with severe hepatic impairment, severe bradycardia, second- or third-degree arteriovenous block or sick sinus syndrome without a pacemaker, or in patients with a known hypersensitivity to carvedilol.
Precautions
May affect lipid and blood sugar levels. May mask signs or symptoms of hypoglycemia and hyperthyroidism. Should be used with caution in patients with peripheral vascular disease.
NYHA = New York Heart Association.
TABLE 4 Suggested Titration of Carvedilol (Coreg) Based on Clinical Signs and Reported Symptoms
ACE = angiotensin converting enzyme.
It may also be necessary, based on clinical signs and symptoms, to adjust the dosages of the patient's other heart failure medications when carvedilol is introduced. When patients have signs and symptoms of excessive vasodilation, such as dizziness, lightheadedness or orthostatic hypotension, consideration should be given to decreasing diuretic, vasodilator or ACE inhibitor dosages. If these signs and symptoms persist, the dosage of carvedilol should be decreased. In patients with signs and symptoms of worsening heart failure, such as edema, weight gain or dyspnea, the dosage of diuretic therapy should be increased. If evidence of worsening heart failure persists, the dosage of carvedilol should be decreased. In patients with bradycardia or first-degree atrioventricular block, carvedilol should be titrated to maintain a heart rate greater than 55 beats per minute. Finally, patients should be advised not to stop taking carvedilol abruptly or without a physician's advice. When carvedilol therapy must be discontinued, the drug should be tapered slowly over seven to 14 days.[6,13,31,38]
Cost and Available Forms
Carvedilol is supplied in tablet form and is available in four dosage strengths: 3.125 mg, 6.25 mg, 12.5 mg and 25 mg. The average wholesale price for all strengths is $1.55 per tablet.[13,38]
REFERENCES
[1.] Eichhorn EJ. Do beta-blockers have a role in patients with congestive heart failure? Cardiol Clin 1994; 12:133-42.
[2.] Effects of carvedilol, a vasodilator-beta-blocker, in patients with congestive heart failure due to ischemic heart disease. Circulation 1995;92:212-8.
[3.] Sharpe N. Beta-blockers in heart failure. Future directions. Eur Heart J 1996;17(Suppl B):39-42.
[4.] Sackner-Bernstein JD, Mancini DM. Rationale for treatment of patients with chronic heart failure with adrenergic blockade. JAMA 1995;274:1462-7 [Published erratum in JAMA 1996;275:686].
[5.] Cohn JN. The management of chronic heart failure. N Engl J Med 1996;335:490-8.
[6.] Eichhorn EJ, Bristow MR. Practical guidelines for initiation of beta-adrenergic blockade in patients with chronic heart failure [Editorial]. Am J Cardiol 1997;79:794-8.
[7.] Packer M. Beta-blockade in the management of chronic heart failure. Eur Heart J 1996;17(Suppl B):21-3.
[8.] Waagstein F. The role of beta-blockers in dilated cardiomyopathy. Curr Opin Cardiol 1995; 10:322-31.
[9.] Neubauer GE, Gaudron P, Horn M, Hu K, Tian R, Krahe T. Beta-blockers in cardiac failure. Eur Heart J 1994; 15(Suppl C): 16-24.
[10.] Kjekshus J, Swedberg K. Treatment of heart failure. J Intern Med 1996;239:335-43.
[11.] Pfeifer MA, Stevenson LW. Beta-adrenergic blockers and survival in heart failure [Editorial]. N Engl J Med 1996:334:1396-7.
[12.] Hash TW 2d, Prisant LM. Beta-blocker use in systolic heart failure and dilated cardiomyopathy. J Clin Pharmacol 1997;37:7-19.
[13.] Chen BP, Chow MS. Focus on carvedilol: a novel beta-adrenergic blocking agent for the treatment of congestive heart failure. Formulary 1997;32(8): 795-805.
[14.] Effect of enalapril on mortality and the development of heart failure in asymptomatic patients with reduced left ventricular ejection fractions. N Engl J Med 1992;327:685-91.
[15.] Pfeifer MA, Braunwald E, Moye LA, Basta L, Brown EJ Jr, Cuddy TE, et al. Effect of captopril on mortality and morbidity in patients with left ventricular dysfunction after myocardial infarction. Results of the survival and ventricular enlargement trial. N Engl J Med 1992;327:669-77.
[16.] Packer M, Bristow MR, Cohn JN, Colucci WS, Fowler MB, Gilbert EM, et al. The effect of carvedilol on morbidity and mortality in patients with chronic heart failure. N Engl J Med 1996;334:1349-55.
[17.] Colucci WS, Packer M, Bristow MR, Gilbert EM, Cohn JN, Fowler MB, et al. Carvedilol inhibits clinical progression in patients with mild symptoms of heart failure. Circulation 1996;94:2800-6.
[18.] Cohn JN, Levine TB, Olivari MT, Garberg V, Lura D, Francis GS, et al. Plasma norepinephrine as a guide to prognosis in patients with chronic congestive heart failure. N Engl J Med 1984;311:819-23.
[19.] Levine TB, Francis GS, Goldsmith SR, Simon AB, Cohn JN. Activity of the sympathetic nervous system and renin-angiotensin system assessed by plasma hormone levels and their relation to hemodynamic abnormalities in congestive heart failure. Am J Cardiol 1982;49:1659-66.
[20.] Waagstein F, Bristow MR, Swedberg K, Camerini F, Fowler MB, Silver MA, et al. Beneficial effects of metoprolol in idiopathic dilated cardiomyopathy. Lancet 1993;342:1441-6.
[21.] Gilbert EM, Anderson JL, Deitchman D, Yanowitz FG, O'Connell JB, Renlund DG, et al. Long-term beta-blocker vasodilator therapy improves cardiac function in idiopathic dilated cardiomyopathy: a double-blind, randomized study of bucindolol versus placebo. Am J Med 1990;88:223-9.
[22.] Bristow MR, O'Connell JB, Gilbert EM, French WJ, Leatherman G, Kantrowitz NE, et al. Dose-response of chronic beta-blocker treatment in heart failure from either idiopathic dilated or ischemic cardiomyopathy. Circulation 1994;89:1632-42.
[23.] The Cardiac Insufficiency Bisoprolol Study (CIBIS). A randomized trial of beta-blockade in heart failure. Circulation 1994.;90:1765-73.
[24.] Olsen SL, Gilbert EM, Rentund DG, Taylor DO, Yanowitz FD, Bristow MR. Carvedilol improves left ventricular function and symptoms in chronic heart failure: a double-blind randomized study. J Am Coil Cardiol 1995;25:1225-31.
[25.] Metra M, Nardi M, Giubbini R, Del Cas L. Effects of short- and long-term carvedilol administration on rest and exercise hemodynamic variables, exercise capacity and clinical conditions in patients with idiopathic dilated cardiomyopathy. J Am Coil Cardiol 1994;24.1678-87.
[26.] Krum H, Sackner-Bernstein JD, Goldsmith RL, Kukin ML, Schwartz B, Penn J, et al. Double-blind, placebo-controlled study of the long-term efficacy of carvedilol in patients with severe chronic heart failure. Circulation 1995;92:1499-506.
[27.] Packer M, Colucci WS, Sackner-Bernstein JD, Liang CS, Goldscher DA; Freeman I, et al. Double-blind, placebo-controlled study of the effects of carvedilol in patients with moderate to severe heart failure. Circulation 1996;94:2793-9.
[28.] Randomised, placebo-controlled trial of carvedilol in patients with congestive heart failure due to ischaemic heart disease. Lancet 1997;349:375-80.
[29.] Moye LA, Abernethy D. Carvedilol in patients with chronic heart failure [Letter]. N Engl J Med 1996;335:1318.
[30.] von Olshausen K, Pop T, Berger J. Carvedilol in patients with chronic heart failure [Letter]. N Engl J Med 1996;335:1318-9.
[31.] Carvedilol. In: Drug facts and comparisons. St. Louis: Facts and Comparisons, 1997:901-4.
[32.] Cohn JN, Archibald DG, Ziesche S, Franciosa JA, Harston WE, Tristani FE, et al. Effect of vasodilator therapy on mortality in chronic congestive heart failure. N Engl J Med 1986;314:1547-52.
[33.] Nichols A J, Gellai M, Ruffolo RR Jr. Studies on the mechanism of arterial vasodilation produced by the novel antihypertensive agent, carvedilol. Fundam Clin Pharmacol 1991;5:25-38.
[34.] Yue TL, Cheng HY, Lysko PG, McKenna PJ, Feuerstein R, Gu JL, et al. Carvedilol, a new vasodilator and beta adrenoceptor antagonist, is an antioxidant and free radical scavenger. J Pharmacol Exp Ther 1992;263:92-8.
[35.] Ruffolo RR Jr, Gellai M, Heibie JR Willette RN, Nichols AJ. The pharmacology of carvedilol. Eur J Clin Pharmacol 1990;38(Suppl 2):82-8.
[36.] Cleland JG, Swedberg K. Carvedilol for heart failure, with care. Lancet 1996;347:1199-201.
[37.] Hauf-Zachariou U, Widmann L, Zulsdorf B, Hennig M, Lang PD. A double-blind comparison of the effects of carvedilol and captopril on serum lipid concentrations in patients with mild to moderate essential hypertension and dyslipidaemia. Eur J Clin Pharm 1993;45:95-100.
[38.] Carvedilol (Coreg). Package insert. Philadelphia: SmithKline Beecham Pharmaceuticals, May 1997.
RELATED ARTICLE: Managing Your Congestive Heart Failure
What is CHF?
Congestive heart failure, or CHF, is a type of heart disease. When the heart can't pump blood properly to the rest of the body, we call it CHF. This may be a temporary problem, or it may last a long time.
What causes CHF?
Heart attacks, rheumatic heart disease, heart muscle damage caused by alcohol or viruses,, high blood pressure, heart valve abnormalities and certain medicines are the major causes of CHF.
How does my doctor know I have CHF?
Your doctor can tell if you have CHF by asking you some questions and giving you a physical exam. Some of the signs of CHF are: reduced ability to exercise, fatigue, breathing problems (especially when lying flat) and swelling of the legs. Your doctor may want you to have an echocardiogram (say: eck-oh-car-dee-oh-gram). This is a special kind of picture. It can tell your doctor how well your heart is pumping and how serious your CHF is.
How is CHF treated?
Several medicines may be used to help prevent or treat the symptoms of CHF. The main medicines are digoxin, diuretics (for example, furosemide or hydrochlorothiazide), ACE inhibitors, vasodilators (for example, nitroglycerin) and beta blockers. These medicines all work in different ways to prevent and treat CHF, so your doctor might have you take more than one of them. Always talk about the side effects of medicines with your doctor. In addition to giving you medicine, your doctor may recommend that you eat a diet low in salt and limit the fluids you drink.
What is carvedilol?
Carvedilol is a medicine known as a beta blocker. It's useful in the treatment of CHF because it decreases the work your heart has to do. The brand name for carvedilol is Coreg.
Should all people with heart failure take carvedilol?
Carvedilol generally isn't used in people who have had severe heart failure, severe liver disease, some heart arrhythmias or asthma. People who had a bad reaction to carvedilol in the past shouldn't take it again.
How and when should I take carvedilol?
Always take carvedilol with food. Take it two hours after you have taken other blood pressure medicines. Never stop taking carvedilol without talking with your doctor first. Your doctor will start you on a low dosage of carvedilol and increase the dosage slowly every two weeks. This way your doctor can watch out for any side effects. In some people, symptoms of heart failure may get worse when they first start taking this medicine.
If I have side effects, should I call my doctor?
Yes. If you feel dizzy or faint when you stand up, call your doctor. You may need to have your dosage adjusted. Weigh yourself every day. If your weight goes up by more than 2 pounds or if you are getting short of breath more easily, call your doctor.
What if I have diabetes?
If you have diabetes and take carvedilol, it may be harder for you to tell when your blood sugar level is too low. Monitoring your blood sugar level more often will help you with this problem.
This information provides a general overview on congestive heart failure and may not apply to everyone. Talk to your family doctor to find out if this information applies to you and to get more information on this subject.
This handout is provided to you by your family doctor and the American Academy of Family Physicians. Other health-related information is available from the AAFP on the World Wide Web (http://www.aafp.org/healthinfo). Information may also be obtained from HealthAnswers[R] (http://www.healthanswers.com). 11/98
BRUCE T. VANDERHOFF, M.D., is associate director of the Grant Family Practice Residency at Grant/Riverside Methodist Hospitals, Columbus, Ohio, and medical director of Grant Family Practice, Grove City, Ohio. He received a medical degree from the University of Pennsylvania School of Medicine, Philadelphia, and completed a residency in family practice at York (Pa.) Hospital.
HEATHER M. RUPPEL, M.D., is a resident in the Grant Family Practice Residency at Grant/Riverside Methodist Hospitals. She received a medical degree from Michigan State University College of Human Medicine, East Lansing.
PETER B. AMSTERDAM, M.D., is staff cardiologist at Grant Medical Center, Columbus, Ohio. He received a medical degree from Harvard Medical School, Boston, and completed a residency in internal medicine at Brigham and Women's Hospital, also in Boston, and a fellowship in cardiology at Duke University Medical Center, Durham, N.C.
Address correspondence to Bruce T. Vanderhoff, M.D., Grant Family Practice Residency, 111 S. Grant Ave., Columbus, OH 43215. Reprints are not available from the authors.
Richard W. Sloan, M.D., R. PH., coordinator of this series, is chairman and residency program director of the Department of Family Medicine at York (Pa.) Hospital and clinical associate professor in family and community medicine at the Milton S. Hershey Medical Center, Pennsylvania State University, Hershey, Pa.
COPYRIGHT 1998 American Academy of Family Physicians
COPYRIGHT 2000 Gale Group